Due to the rarity of localized pigmented villonodular synovitis of the wrist presenting as carpal tunnel syndrome, a systematic treatment approach needs to be followed which includes adequate pre-operative investigations and ensuring total excision of the lesion along with carpal tunnel release intraoperatively to obtain good long-term outcomes without any recurrence.
Dr. Aashiket Sable, Department of Orthopaedics, Bharatratna Dr. Babasaheb Ambedkar Municipal General Hospital, Mumbai, Maharashtra, India. E-mail: aashiketsable67@gmail.com
Introduction: A form of tenosynovial giant cell tumors (GCTs) that diffusely affects the soft tissue lining of joints and tendons is called pigmented villonodular synovitis or PVNS. About equal percentages of men and women are often affected, and it typically affects young individuals. The most typical sites of PVNS are the knee and ankle, making PVNS of the wrist a rare presentation. Patients with PVNS might develop symptoms of carpal tunnel syndrome (CTS) and only a handful of cases are reported in the literature. The gold standard of treatment has traditionally been surgical excision for localized lesions and additional total synovectomy of the affected joint in cases of diffuse PVNS. The objective of this article is to present a patient with PVNS of the right wrist leading to CTS, resolved with surgical treatment which led to satisfactory results.
Case Report: A 29-year-old right-hand dominant female patient arrived at our out-patient department with complaints of swelling, pain, tingling, and numbness of the right palm. The patient had similar complaints 1 year ago when carpal tunnel release surgery was done for her elsewhere. After 1 year of surgery, the symptoms persisted along with diffuse swelling. Clinical examination of the patient confirmed the presence of CTS. A tenosynovial mass around the flexor tendons located along the carpal tunnel at the level of the distal radioulnar joint was visible on magnetic resonance imaging. The median nerve’s conduction velocity was found to be lowered on electrodiagnostic testing. Total lesion excision was done along with carpal tunnel release, and the mass was excised and sent for histopathology. Histopathological evaluation of the extracted material confirmed the diagnosis of PVNS. At the 5-year follow-up, there were no complaints or indications of recurrence.
Conclusion: Localized PVNS of the wrist presenting as CTS is a rare condition. To diagnose this illness, several investigations and a high index of suspicion are needed. Total excision of the lesion, along with surgical release of the carpal tunnel, should be ensured to avoid recurrence.
Keywords: Pigmented villonodular synovitis, carpal tunnel syndrome, carpal tunnel release.
Pigmented villonodular synovitis (PVNS) is a form of tenosynovial giant cell tumor (GCT) that diffusely affects the soft tissue lining of joints and tendons. GCT of the tendon sheath was originally documented by Chassaignac in 1852, and at the time, he thought that the lesions were sarcomata. Because it was defined using a variety of names, including giant-cell tumor and benign synovioma, earlier research on the subject was contentious [1]. These lesions were identified by Masson as xanthoma, and he further classified them into two forms: an extended form and a nodular mass form. The tumor was described as being composed of variously sized yellow-orange lobes that were enclosed in a thin capsule [2]. Jaffe et al. reviewed twenty instances, including bursae, tendon sheaths, and joints, before coining the name PVNS in 1941. He concluded that the lesions were an inflammatory reaction to an unidentified chemical rather than malignancies after noting that the “nodular” and “diffuse” lesions shared similar histological characteristics [3]. Conversely, a few publications endorsed the theory that PVNS was caused by the neoplastic growth of histiocytes and synovial fibroblasts [4,5]. Fisk linked PVNS to recurrent mild trauma, which is generally not credible. To sum up, despite all these attempts to elucidate the pathogenesis, the actual causing agent remains uncommon [6]. PVNS, common in the knee and hip, is only used for intraarticular lesions and PVNS of the wrist is very rare, with just a few examples documented in the literature [7,8]. The gold standard of treatment has traditionally been surgical excision for localized lesions and additional total synovectomy of the affected joint in diffuse PVNS. However, PVNS has a 50% chance of recurrence even after surgery, which has led researchers to look at alternative therapeutic solutions [8]. The most prevalent compression neuropathy affecting the upper limb is carpal tunnel syndrome (CTS). Because of the anatomical proximity of the median nerve, any pathological process in the carpal tunnel may be expected to affect the median nerve. The frequency with which PVNS appears in the wrist is rare, and it is not expected to present as a cause of CTS [8]. Therefore, the objective of this article is to present a rare case of PVNS of the right wrist leading to CTS, resolved with surgical treatment which led to satisfactory results.
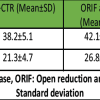
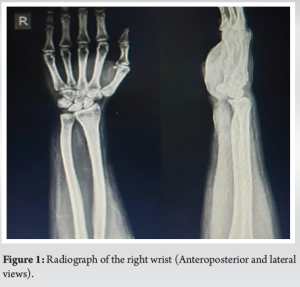
A 29-year-old right-hand dominant female patient arrived at our out-patient department complaints of swelling, pain, tingling, and numbness of the right palm. The patient denied any history of recent trauma, and the cervical spine examination was within normal limits. She had a similar episode 1 year prior, with complaints of moderate wrist pain and mild paresthesia, but without any swelling, for which carpal tunnel release was done elsewhere. The patient was symptom-free after the primary surgery for a year. Still, the symptoms had aggravated in the past 6 months before presenting to us, and complaints were noted around the right wrist, not relieved by analgesics, gabapentin, icing, or elevation. On physical examination, a diffuse swelling of approximately 3 × 4 cm was seen along the wrist’s volar aspect [Zone 5 of flexors]. The swelling was painful on palpation, finger’s range of motion was normal. Still, the wrist had 20° of flexion, 20° of extension, and restricted radial and ulnar deviation, primarily due to pain. Further movement was possible but was painful. Tinel, Phalen, and Durkan tests were attempted which came out positive. Sensations were reduced along median nerve distribution, but the radial pulse was regular. Hematological parameters, as well as radiographs of the right wrist and hand, were normal (Fig. 1). A tenosynovial mass around the flexor tendons located along the carpal tunnel at the level of the distal radioulnar joint, suggestive of PVNS, was discovered on magnetic resonance imaging (MRI), which was performed to further assess the cause of any underlying pathology (Fig. 2). Nerve conduction studies (NCS) showed reduced conduction around median nerve distribution.
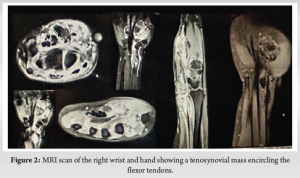
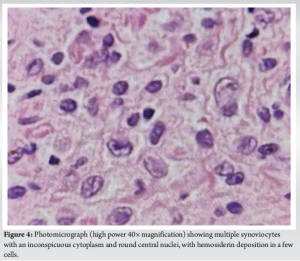
We suspected a confined synovial non-malignant tumor based on the clinic-radiological data. Thus, we decided to operate without first doing a biopsy. Through a brachial plexus block, a regional anesthetic was used. Past the distal palmar crease, an incision was made along the FCR tendon sheath, approximately 10 cm volar longitudinal. Under close supervision, the dissection was continued until the transverse carpal ligament was released (Fig. 3). The dumb-bell-shaped bilobed mass encapsulated by a fine pseudo capsule was excised. Excision in the palm was more critical since it was entangled with the median nerve. The flexor tendons were found to be intact. The removed mass was sent for histopathological analysis, which confirmed PVNS. Macroscopic findings showed a yellowish-brown colored mass with few nodules and fibrous septae in between, and microscopic findings showed multiple synoviocytes with an inconspicuous cytoplasm as well as round central nuclei, with hemosiderin deposition in a few cells (Fig. 4).
The time following surgery was uneventful. A wrist splint was given for 2 weeks and the patient was advised physiotherapy for 3 months. The patient was followed up every week for the 1st 4 weeks and then at 3 monthly intervals for 5 years. The wrist’s flexion and extension range was 70° each, respectively, within 6-months postoperatively, comparable with the opposite wrist. At the past 5 year follow-up, the female was symptom-free. She had been able to resume her activities of daily living satisfactorily and continue her profession without any significant discomfort.
The pathologic processes underlying PVNS and GCT of tendon sheath are the same, and their histopathological appearances are comparable [9]. PVNS is a term used to describe intraarticular lesions, which are frequent in the hip and knee [7]. When referring to extraarticular lesions, GCT of tendon sheath (GCTTS) can be widespread (diffuse) or confined (nodular). Nodular GCTTS frequently manifests as hard, slowly developing nodules in the hand that are well-circumscribed. Compared to the nodular variant, diffuse GCTTS, also known as extraarticular PVNS, is far less prevalent and typically affects the knee [10]. A GCT of the flexor tendon sheath is a rare entity and is all the more unusual as an underlying cause of carpal tunnel syndrome in young adults. Yet, some authors have reported an association between the two [7,8,9]. But as far as PVNS leading to CTS is concerned, the research is further limited [11]. Chidgey in 1988 described an 89-year-old female who developed symptoms following the aspiration of her wrist [12]. Gökay et al. in 2009 reported two cases in young adults, one in the flexor and the other being in the extensor compartment of the respective patients, successfully treated with large tenosynovectomy [8]. These were all diffuse lesions treated with synovectomy and as per our knowledge, ours is the first reported case of localized PVNS presenting as CTS proven histopathologically. PVNS is a progressive and benign condition that rarely progresses destructively [11]. Since the exact etiology of PVNS is still unknown, the best course of treatment has not yet been developed. Complete excision along with total synovectomy is the preferred treatment method in patients with diffuse PVNS without distinctive joint damage and bone erosion, either by open or arthroscopic means. When complete removal is not possible through synovectomy, post-operative radiotherapy has been advocated [8]. As far as our case is concerned, we had an intra-articular localized lesion which was excised thoroughly without the need for a total synovectomy. Although space-occupying lesions (ganglion or fibroma) have been described as the cause of carpal tunnel syndrome, pre-operative imaging studies are not commonly done [13]. We believe that in such cases, a systematic treatment approach should be followed. An MRI should be done to localize the lesion accurately and distinguish between a localized or a diffuse variety. NCS should be advocated to detect neuropathy. In our case, we followed this approach to ensure proper surgical planning using MRI and NCS. This helped us to excise the lesion completely without any recurrences or post-operative complications. In terms of the treatment, experts are of the opinion to perform a total excision for localized lesions and an extensive synovectomy in cases of the diffuse variety; yet, high recurrence rates are high [8]. To avoid recurrence in cases where a space-occupying lesion is considered as one of the differentials of CTS, we think that complete carpal tunnel release, including adequate exploration in between the flexor tendons and down the rest of the tunnel, is a must during excision to avoid leaving any residual mass behind. Our case presented a recurrence after a carpal tunnel release was done for the patient elsewhere. As a secondary definite surgery, a thorough exploration of the carpal tunnel was done, with total excision of the lesion, while protecting the median nerve. We believe adequate pre-operative investigations, proper surgical planning, and adequate intraoperative exploration and release, helped us achieve good long-term results as in our case where we achieved wrist ROM comparable to the opposite normal wrist at the 5-year follow-up. As literature supporting this condition is limited, we believe that this is the first case report with a systematically planned treatment approach along with histopathological evidence, which led to good 5-year outcomes. Yet, we believe that increased vigilance among surgeons and further research is needed as far as PVNS of the wrist leading to CTS is concerned.
Localized PVNS of the wrist presenting as CTS is a rare condition. A high index of suspicion and an array of investigations including MRI and NCS are needed to diagnose this condition, specifically to avoid recurrence. Surgery should be offered in the form of complete excision in case of a localized lesion and total synovectomy in cases of widespread PVNS while protecting the median nerve. Complete excision of the lesion/pathology is of utmost importance to avoid recurrence. In our case presented here, we could adequately investigate and study the lesion before surgery and then excise the lesion totally without any trauma to the median nerve. We believe that staying vigilant and properly investigating this rare condition before surgery, and exploring the carpal tunnel adequately during surgery, is most important, to obtain good long-term outcomes, as were demonstrated in our case where we got an acceptable 5-year outcome.
Due to the rarity of localized pigmented villonodular synovitis of the wrist presenting as carpal tunnel syndrome, a systematic treatment approach needs to be followed which includes adequate pre-operative investigations and ensuring total excision of the lesion along with carpal tunnel release intraoperatively to obtain good long-term outcomes without any recurrence.
References
- 1.Chassaignac C. Cancer de la gaine des tendons. Gaz Hop Civ Milit 1852;47:185-6. [Google Scholar | PubMed]
- 2.Masson M. Tumours of the hand. Surg Gynecol Obstet 1937;64:129-48. [Google Scholar | PubMed]
- 3.Jaffe H, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol 1941;31:731-65. [Google Scholar | PubMed]
- 4.Rao AS, Vigorita VJ. Pigmented villonodular synovitis [giant-cell tumor of the tendon sheath and synovial membrane]. A review of eighty-one cases. J Bone Joint Surg Am 1984;66:76-94. [Google Scholar | PubMed]
- 5.Abdul-Karim FW, El-Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: A clinicopathologic and flow cytometric DNA analysis. Hum Pathol 1992;23:729-35. [Google Scholar | PubMed]
- 6.Fisk GR. Hyperplasia and metaplasia in synovial membrane. Ann R Coll Surg Engl 1952;11:157-70. [Google Scholar | PubMed]
- 7.Schwartz GB, Coleman DA. Pigmented villonodular synovitis involving the wrist: A Case report. Iowa Orthop J 1986;6:129-32. [Google Scholar | PubMed]
- 8.Gökay NS, Yalçin MB, Bagatur E. Pigmented villonodular tenosynovitis at wrist: Presentation of two cases reports. Yeditepe Med J 2009;11:231-4. [Google Scholar | PubMed]
- 9.Ward CM, Lueck NE, Steyers CM. Acute carpal tunnel syndrome caused by diffuse giant cell tumor of tendon sheath: A case report. Iowa Orthop J 2007;27:99-103. [Google Scholar | PubMed]
- 10.Kempson RL, Fletcher CD, Evans HL, Hendrickson MR, Sibley RK. Atlas of Tumor Pathology. In: Tumors of the Soft Tissues. Washington DC: Armed Forces Institute of Pathology; 2001. p. 388-93. [Google Scholar | PubMed]
- 11.Jamieson TW, Curran JJ, Desmet AA, Cotelingam JD, Kimmich H. Bilateral pigmented villonodular synovitis of the wrists. Orthop Rev 1990;19:432-6. [Google Scholar | PubMed]
- 12.Chidgey LK, Szabo RM, Wiese DA. Acute carpal tunnel syndrome caused by pigmented villonodular synovitis of the wrist. Clin Orthop Relat Res 1988;228:254-7. [Google Scholar | PubMed]
- 13.Athanasian EA. Bone and soft tissue tumors. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, editors. Green’s Operative Hand Surgery. Philadelphia, PA: Elsevier Churchill Livingstone; 2005. p. 2221-42. [Google Scholar | PubMed]