Paraspinal abscesses are rare but can progress broadly if the diagnosis is delayed; therefore, local physical examination for swelling, wave sensation, and heat are most important
Dr. Junya Kusakabe , Department of Orthopaedic Surgery, Miyagi Cancer Center, Natori, Japan, junya.k.0109@gmail.com
Introduction: Paraspinal muscle abscesses are rare, and generally occur due to injections or hematogenous dissemination. Here, we describe a rare case of a paraspinal muscle and the ipsilateral psoas major abscess in the lumbar region that communicated via the interspaces of the costal processes.
Case Report: An 83-year-old man with poorly controlled diabetes mellitus and no history of puncture complained of right low back pain for the past 2 months. He was diagnosed with pyelonephritis and referred to our department for close examination of the low back pain. Magnetic resonance imaging revealed a paraspinal muscle and an ipsilateral psoas major abscess in the lumbar region, which communicated through the interspaces of the costal processes. A definitive diagnosis was made using percutaneous aspiration and the patient was successfully treated conservatively.
Conclusion: This case is very rare and impressive because the paraspinal muscle abscess directly communicated with the ipsilateral psoas major muscle abscess. Spinal infections should always be considered in the differential diagnosis of low back pain, particularly in the absence of long-term improvement. Local physical examinations are essential when examining patients with low back pain. Conservative treatment is effective, even if the abscess is extensive.
Keywords: Spinal infection, paraspinal abscess, physical examination.
Spinal infection is defined as an infectious disease affecting the vertebral body, the intervertebral disc, and/or adjacent paraspinal tissue [1,2]. Paraspinal muscle abscesses are rare and generally occur due to injections [3] or hematogenous dissemination [4]. We describe a rare case of a paraspinal muscle and the ipsilateral psoas major abscess in the lumbar region that communicated through the interspaces of the costal processes.
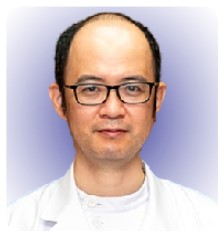
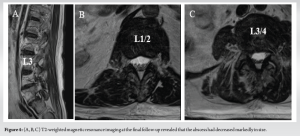
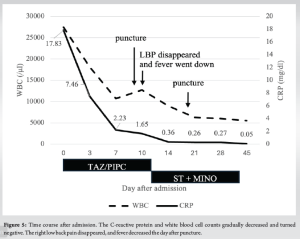
An 83-year-old man was admitted to the department of urology at our hospital for further examination due to urinary retention in the past month. He had no history of lumbar puncture but had a medical history of benign prostate hypertrophy and diabetes mellitus. Fever and elevated C-reactive protein (CRP) levels indicated a diagnosis of pyelonephritis. Methicillin-resistant Staphylococcus aureus (MRSA) was confirmed through blood and urine cultures, and tazobactam piperacillin was changed to trimethoprim-sulfamethoxazole and minocycline based on antibiotic susceptibility. The patient experienced right back pain during physical activity 2 months before admission and was referred to our department on day 8 after admission. On initial examination, his body temperature was 37.2°C; swelling, local heat, fluctuation, and tenderness were detected in the right paraspinal muscle of the lumbar region. Right low back pain develops during forward movement, extension, and bilateral bending. The patient reported no nocturnal pain or neurological deficits. On admission, his white blood cell count was 27,500/μL and the CRP was 17.8 mg/dL, hemoglobin A1c was 12.0%, and blood glucose level was 305 mg/dL. A urologist consulted a diabetologist. Insulin-fortified therapy was initiated, and the blood glucose levels were well controlled. Plain lumbar radiographs revealed sciatic scoliosis on the right side and contrast-enhanced computed tomography (CT) revealed a low-absorption area with rim enhancement in the right paraspinal muscle (Fig. 1a, b, c, d). Magnetic resonance imaging (MRI) of the spine revealed a low-intensity lesion on T1-weighted images compared with the muscle intensity, with rim enhancement extending into the right psoas major muscle through the interspaces of the costal processes at the L1/2 level. There were no signs of an epidural abscess or facet infection (Fig. 1e, f, g, h).
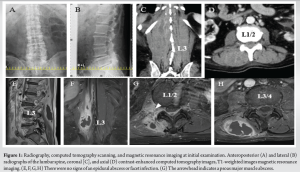
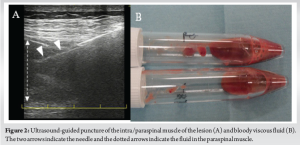
We performed ultrasound-guided puncture of the lesion intra-paraspinal muscle with 14G Fine Core® (Toray Medical Co. Ltd., Tokyo, Japan) (Fig. 2a). Approximately 18 mL of bloody viscous fluid (Fig. 2b) was aspirated and MRSA was detected using a culture test. The antimicrobial sensitivity pattern was similar to that observed in initial urine cultures. Echocardiography revealed no vegetation. Pathological examination of a biopsy specimen obtained from a paraspinal muscle lesion revealed neutrophil infiltration. The day after the percutaneous aspiration, the back pain during movement and tenderness in the right paraspinal muscle disappeared. CRP levels decreased over time, and MRI revealed that the abscess had markedly decreased in size (Fig. 3a, b, c, d). Additional percutaneous aspiration was performed using an 18G needle, and approximately 8 mL of bloody viscous fluid (Fig. 3e) was aspirated; the culture was negative. Antibiotics were administered for approximately 6 weeks. The CRP test results were negative, and MRI revealed a prominent reduction in abscess size with no symptom recurrence (Fig. 4a, b, c and 5).
Pyomyositis is a rare primary muscle infection that is likely the result of transient bacteremia in most patients. The most common site of infection is the quadriceps muscle (26.3%), followed by the iliopsoas muscle (14%), and the paraspinal muscles (3.8%) [5]. In this case, it was unlikely that pyelonephritis had directly spread into the psoas major because there was no intensity change in the pararenal tissue on MRI. The abscesses in the interspaces of the costal processes and psoas muscle were at the same L2 level. To date, PubMed, Ovid Medline, and Scopus have only one report of an abscess (pyomyositis) directly spreading to the ipsilateral psoas major muscle [6]. One report described a case of a paraspinal muscle abscess extending into the quadratus lumborum muscle [7]. As a paraspinal muscle abscess progresses, it can extend into adjacent tissues such as the psoas major or quadratus lumborum muscles.
The diagnosis of paraspinal muscle abscesses should always be supported by clinical, laboratory, and imaging findings, and MRI remains the most reliable diagnostic imaging method [1]. Delays in the presentation and diagnosis are almost universal in the treatment of spinal infections. Immunosuppressed patients tend to have longer delays in presentation and diagnosis due to less vigorous inflammation and pain generation [8]. Delays in diagnosis and treatment are commonly due to the insidious presentation of physical signs and symptoms, especially in children and the elderly, which may increase morbidity and mortality [9]. In this case, the patient presented with low back pain for 2 months and no history of puncture. Even in the absence of a history of puncture, poorly controlled diabetes mellitus can result in a paraspinal abscess. This report indicates that spinal infections must always be considered in the differential diagnosis of low back pain, especially low back pain with no long-term improvement. Local physical examinations are essential when examining patients with low back pain.
Conservative treatment for paraspinal abscesses is generally reasonable in the early stages with no or minor neurological deficits. Antibiotic treatment reaches the paraspinal tissues more easily than the non-vascularized disc space [1]. Percutaneous CT- or ultrasound-guided drainage may be indicated in cases of large abscesses [1]. Percutaneous drainage of paraspinal muscle abscesses using spinal ultrasonography is an easy-to-perform and less invasive diagnostic and therapeutic procedure [10]. In this case, ultrasound-guided drainage was useful for the identification of organisms, source control, and treatment course evaluation.
A paraspinal abscess could progress if the diagnosis is delayed; therefore, local physical examination is important for early diagnosis and ultrasound sonography is useful modality. We present a rare case of an extensive abscess with rare progressive forms that was treated conservatively.
The key to overlooking paraspinal abscesses and the treatment course of extensive abscesses with rare progressive forms are described in this report.
References
- 1.Lener S, Hartmann S, Barbagallo GM, Certo F, Thomé C, Tschugg A. Management of spinal infection: A review of the literature. Acta Neurochir (Wien) 2018;160:487-96. [Google Scholar | PubMed]
- 2.Duarte RM, Vaccaro AR. Spinal infection: State of the art and management algorithm. Eur Spine J 2013;22:2787-99. [Google Scholar | PubMed]
- 3.Magee M, Kannangara S, Dennien B, Linergan R, Emmett L, Van der Wall H. Paraspinal abscess complicating facet joint injection. Clin Nucl Med 2000;25:71-3. [Google Scholar | PubMed]
- 4.Raj V, Foy J. Paraspinal abscess associated with epidural in labour. Anaesth Intensive Care 1998;26:424-6. [Google Scholar | PubMed]
- 5.Brickels J, Ben-Sira L, Kessler A, Wientorub S. Primary pyomyositis. J Bone Joint Surg 2002;84:2277-86. [Google Scholar | PubMed]
- 6.Unnikrishnan D, Delacruz MA, Saha A, Daniels R. Case of acute paraspinal pyomyositis in an elderly diabetic secondary to spread from urinary tract infection. BMJ Case Rep 2018;2018:bcr2018225739. [Google Scholar | PubMed]
- 7.Hassan FO, Shannak A. Primary pyomyositis of the paraspinal muscles: A case report and literature review. Eur Spine J 2008;17 Suppl 2:S239-42. [Google Scholar | PubMed]
- 8.Cunningham ME, Giradi F, Papadopoulos EC, Cammisa FP. Spinal infections in patients with compromised immune systems. Clin Orthop Relat Res 2006;444:73-82. [Google Scholar | PubMed]
- 9.Govender S. Spinal infections. J Bone Joint Surg Br 2005;87:1454-8. [Google Scholar | PubMed]
- 10.Darrieutort-Laffite C, Hamel O, Glémarec J, Maugars Y, Le Goff B. Ultrasonography of the lumbar spine: Sonoanatomy and practical applications. Joint Bone Spine 2014;81:130-6. [Google Scholar | PubMed]