Chronic ruptures of the pectoralis major are becoming increasingly common; we discuss the latest concepts regarding the indications for surgical treatment and the various operative techniques.
Dr. Igor Gossuin, Service de Chirurgie orthopédique et de traumatologie, Centre Hospitalier Universitaire Vaudois (CHUV), Rue du Bugnon 46, CH – 1010 Lausanne. Phone: +41 21 311 11 11, E-mail: igor.gossuin@gmail.com
Introduction: Various surgical repair techniques, including autograft and allograft reconstructions, have been reported for the management of chronic pectoralis major ruptures, but outcome reporting remains highly heterogeneous. This narrative review aimed to provide a deeper understanding of these techniques, emphasizing the need for larger-scale prospective trials to support evidence-based recommendations for surgeons.
Materials and Methods: We conducted a search of PubMed/Medline, Cochrane Library, Embase, and Google Scholar for English-language articles published between 1822 and 2023, using the following keywords: “chronic pectoralis major ruptures,” “chronic pectoralis major tears,” and “patient outcomes.”
Results: Overall, more than 60 reported cases were retrieved, along with a few prospective studies and review articles. Based on the compiled literature, most pectoralis major tears tend to arise at the tendo-osseus junction. In the absence of contra-indications such as old age and multiple comorbidities, surgical intervention is considered the golden care standard. The most commonly performed repair techniques include suture anchor fixation, transosseous fixation (TOS), and cortical bone fixation. Among the three techniques, no significant differences in cyclic loading or load-to-failure properties of the constructs were recorded. In chronic cases, in which direct repair is not possible, various autograft and allograft reconstructions were described, with quite heterogeneous outcome reporting, rendering comparative analyses difficult.
Conclusion: Currently, no single technique has been established as the gold standard for the treatment of chronic pectoralis major ruptures. The most commonly performed repair techniques include suture anchor fixation, TOS, and cortical bone fixation. In chronic cases where direct repair is not feasible, various autograft and allograft reconstructions are employed. There is a need for larger-scale prospective trials with standardized outcome reporting to develop evidence-based recommendations, providing surgeons with safe and effective guidelines for treatment.
Keywords: Pectoralis major, chronic ruptures, chronic tears, shoulder, therapeutic options, repair techniques, reconstruction techniques.
Although pectoralis major injuries are relatively rare, their incidence has steadily increased over the past two decades, driven by the rise in weight-lifting exercises and other demanding sports, along with the potential dysplastic effects of increased steroid use on collagen fibrils [1]. The injury was first described by Patissier et al. in 1822 in a French boy lifting a heavy piece of meat [2]; however, the majority of cases have been reported in the last two decades. If left untreated or improperly managed, acute pectoralis major injuries can lead to chronic conditions, deformities, and physical disabilities. Chronic injuries are generally defined as those persisting for more than 6 weeks, although the exact definition varies among reports. Appropriate repairs are often delayed due to misdiagnosis and post-poned treatment initiation. Historically, these injuries were commonly managed nonoperatively, particularly in elderly patients, through physical therapy, activity modifications, and oral anti-inflammatory agents. Nonetheless, most experts agree that surgical repair is now the gold standard for treating chronic pectoralis major ruptures, especially to help young, active patients regain full strength. Consequently, surgical management of chronic pectoralis major injuries, typically through a deltopectoral approach, is now widely preferred, as it has consistently demonstrated better outcomes in terms of function, strength, subjective scores, and return to pre-injury performance compared to non-surgical treatment [3,4]. , it is important to note that surgical interventions can present significant challenges, even for experienced surgeons, due to factors such as tendon retraction, poor tendon quality, muscle atrophy, scar formation, and altered anatomy. These structural abnormalities complicate direct repairs and often necessitate the use of autograft or allograft reconstruction techniques [5]. Despite the critical nature of these injuries, the literature on chronic pectoralis major ruptures remains limited, primarily consisting of case studies. This narrative review aims to provide a concise overview of the various surgical approaches employed in managing chronic pectoralis major ruptures while emphasizing the need for larger scale, controlled trials to develop evidence-based recommendations that enhance patient care and satisfaction.
Anatomical Reminder
The pectoralis major is a thick, fan-shaped, superficial muscle that covers the anterior chest wall and contributes to thoraco-brachial motion. It consists of two heads: the clavicular and sternocostal, named for their points of origin. The muscle fibers from both heads converge to form a single tendon that inserts into the crest of the greater tubercle of the humerus. The primary functions of the pectoralis major include adducting, medially rotating, and transversally adducting the upper arm at the shoulder joint. Due to its anatomy, the pectoralis major is prone to rupture when subjected to maximum tension during abduction and external rotation [6]. Typically, such injuries occur in muscular young adults, pre-dominantly males, during activities such as bench pressing, weight lifting, and strength training, although other demanding sports, such as rugby, wrestling, and boxing, have also been implicated [7]. The concomitant use of anabolic steroids is considered a risk factor. While these ruptures mainly affect young adults aged 20–40, a systematic review by ElMaraghy et al. in 2012 reported 11 cases of pectoralis major ruptures in elderly women aged 73–97 [8].
Classification of Pectoralis Major Injuries
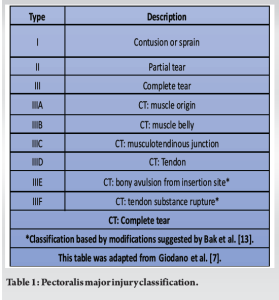
Depending on their degree, these injuries are classified as muscle strain (Type I), partial tear (Type II), and complete tear (Type III), these latter being subdivided depending on their location into Type IIIA muscle origin, Type IIIB muscle belly, Type IIIC myotendinous junction, and Type IIID tendon [9]. Recently, two other subtypes have been added, including Type IIIE referring to a bony avulsion from the insertion site, and Type IIIF corresponding to a muscle tendon substance rupture, as summarized in Table 1 [10]. Of note is that Type IIID is the most common, with a rate of 60%, followed by Type IIIC occurring with a frequency of about 27% [11,12,13].
Clinical Presentation
On physical shoulder examination, an anterior axillary deformity can often be noticed, along with medial retraction of the pectoralis major muscle, tenderness of its tendon insertion, and full passive range of motion (ROM) [13]. In 2012, ElMaraghy created a clinical examination test pertaining to pectoralis major injury, at the acute stage, called pectoralis major index. This test facilitates the diagnosis of pectoralis major tears, being instrumental in avoiding unnecessary delays or failure to establish proper diagnosis [11]. Any delay in treatment initiation, at the acute stage, increases the risk of chronic disease, associated with functional strength loss and hindered return to sport. While conventional X-ray is considered inadequate as a diagnostic tool, ultrasound has proven to be more effective in identifying tears [14], with magnetic resonance imaging (MRI) of the chest being the method of choice to precisely locate the tears [15]. For chronic pectoralis major tears, T1-weighted axial images are most likely to readily identify the typical characteristics of chronic diseases, such as fibrosis, adhesions, and scarring [16].
Definition of Chronic Injury
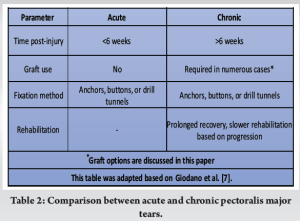
At present, pectoralis injury tears are increasingly classified depending on their chronicity, which considerably influences their therapeutic management. Nevertheless, it must be stressed that the definition of chronic tears remains ambiguous across the scientific literature. In the current review, we have defined chronic tears in line with the recently CiSE-published paper by Giordano et al. [7] According to their and our definition, chronic tears correspond to injuries presenting at least 6 weeks following the initial traumatic event (Table 2).
For this review, we conducted a search of the PubMed/Medline, Embase, Cochrane Library, and Google Scholar databases for articles published in English. The search utilized the following terms: “pectoralis major ruptures,” “pectoralis major tears,” and “patient outcomes.” This was carried out as a narrative study. We briefly reviewed all articles focusing on pectoralis major tears published from 1822 to December 2023, retrieving over 60 reported cases, along with several prospective studies and review. Based on the compiled literature, we aimed to gain a deeper understanding of the various surgical approaches for chronic pectoralis major ruptures. By leveraging insights from contemporary literature and scientific discussions, this review seeks to enhance our understanding of these techniques while emphasizing the need for larger-scale prospective trials to inform clinical practices and policies, ultimately improving patient outcomes and satisfaction.
Ethical Considerations
The selected papers relevant to this review were analyzed anonymously, and the requirement for informed consent was waived due to the retrospective nature of the study. In addition, the study was conducted in accordance with the ethical standards set forth in the 1964 Declaration of Helsinki and its subsequent amendments.
Regarding therapeutic strategies, several authors have previously shown that acute surgical repair yields superior results compared to delayed surgical repair. Furthermore, delayed surgical repair is associated with better outcomes than conservative treatment in terms of pain, strength, and esthetics [5,13,17]. While a few therapeutic interventions can be employed for both acute and chronic injury cases, the following section is primarily focused on chronic tear lesions and their management. Nonoperative measures, which are not the scope of our study, are at times preferred for elderly patients, with a less active lifestyle and less extensive tears, along with numerous comorbidities and poor post-operative compliance [18]. Similarly, such non-operative measures can also be applied at the treating physician’s discretion for chronic partial tears and muscle belly ruptures or for patients with irreparable damage [3,5]. In contrast, in younger patients with an active and high-demand lifestyle, chronic pectoralis major tears are primarily managed operatively by either repair or allograft and autograft reconstructions, depending on patient factors, including patient age, activity, medical comorbidities, and prior use of anabolic steroids, in addition to tear factors, including tear morphology, chronicity, and severity, as well as the number of heads involved [7]. The choice between repair versus reconstruction is primary dependent on the injury location and its chronicity.
Techniques for Tendon Fixation
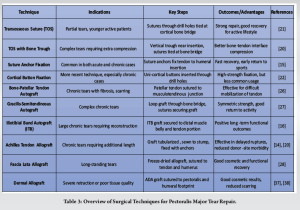
Repair techniques for chronic pectoralis major ruptures vary widely in the scientific literature, particularly regarding fixation methods. Three major fixation techniques are commonly described: transosseous suture (TOS) with fixation through a drill hole, sometimes with the addition of a bone trough; suture anchor fixation; and cortical button fixation [19]. Several other minor repair techniques, such as bone tunnels, were identified but will not be detailed here. Based on our literature review, the TOS technique and suture anchor fixation were the most frequently employed methods for managing partial tears, both yielding successful outcomes for individuals looking to preserve strength and maintain an active lifestyle. The TOS technique involves placing drill holes laterally to the pectoralis major’s insertion, where the suture is threaded inside the tendon and pulled through two different sets of drill holes before being tied to the lateral cortical bone bridge. A modified version, known as TOS with a bone trough, involves creating a vertical trough laterally to the insertion. This technique uses drill holes positioned laterally to the trough, with sutures tied through these holes at the bony bridge, facilitating compression of the bone-tendon interface by allowing the tendon stump to fit into the trough [20]. In contrast, the suture anchor technique involves engaging bone anchors preloaded with high-strength non-absorbable sutures into the pectoralis major insertion. The sutures are then passed through the tendon and secured to its anatomical insertion at the proximal anterior aspect of the humerus. According to our literature search, these two techniques are the most commonly applied, leading to rapid recovery and a prompt return to sports with only minor limitations [15,19]. A more recent technique involves unicortical button fixation, which entails drilling uni-cortical holes at the pectoralis major’s insertion and placing buttons preloaded with high-strength sutures through these holes to serve as fixation points. In addition, bicortical button fixations were also identified in our review, but due to their less frequent use, they will not be discussed further [21]. In a notable biomechanical study, Sherman et al. compared the three most common surgical repair techniques for pectoralis major ruptures using fresh-frozen cadaveric shoulders [22]. Their findings indicated no significant differences in biochemical outcomes, such as cyclic loading or load-to-failure properties, among the three techniques. However, another study focused on the biochemical analysis of these repair methods found a significant increase in load-to-failure properties for TOS with bone trough compared to suture anchor and cortical button fixation procedures [23]. For the TOS technique, with drill holes placed laterally to the pectoralis major’s insertion, the suture positioned inside the tendon is pulled through two different drill hole sets, before being tied at the lateral cortical bone bridge. A modified technique, termed TOS with a bone trough, was also retrieved. This modified TOS consists of implanting a vertical trough laterally to the insertion while setting drill holes laterally to the trough, before tying suture through the drill holes at the bony bridge. By fashioning a trough for the tendon stump to fit in, this technique facilitates compression of the bone-tendon interface. With respect to the suture anchor technique, this procedure consists of engaging bone anchors, being preloaded with high-strength non-absorbable suture, into the pectoralis major’s insertion, then passing the sutures through the tendon before fixating the latter to its anatomic humeral insertion, at the proximal anterior site of the humerus. Based on our literature search, these two techniques were the most commonly applied, clearly leading to a fast recovery, along with a prompt return to sports with only minor limitations [15,20].
A more recently developed technique refers to uni-cortical button fixation by means of drilling uni-cortical humeral holes at the pectoralis major’s insertion, while placing buttons preloaded with a high-strength suture through the drill holes, thus serving as a fixation post [21]. Of note is that bi-cortical button fixations were also retrieved from our literature search [21]. Nevertheless, these procedures are not further discussed below, on account of their less frequent use. In a remarkable biomechanical study, Sherman et al. compared the three most common surgical repair techniques for pectoralis major ruptures, using fresh-frozen cadaveric shoulders. According to the authors’ conclusion, no significant difference in any biochemical outcomes, such as cyclic loading or load-to-failure properties, was recorded among the three repair techniques. Yet, in another similar study focused on biochemical analysis of the three different repair techniques, a significant increase in load-to-failure properties was found for TOS with bone trough versus suture anchor and cortical button fixation procedures [19].
Reconstruction Technique
When sufficient tendon mobilization cannot be achieved through the primary incision, making direct tendon attachment impossible, the primary repair is unlikely to produce satisfactory results. In such cases, autograft or allograft reconstruction is generally more appropriate, as these methods have demonstrated effectiveness with favorable outcomes. However, despite the Bak et al. outcome criteria for assessing post-surgery function — classifying results as excellent, good, fair, or poor — the reported outcomes for pectoralis major reconstructions remain highly heterogeneous across the literature, making comparisons between techniques difficult or even impossible [13]. Our literature search identified numerous autograft and allograft techniques, each associated with varying outcome reports. Among the autografts, several approaches were commonly described, including bone–patellar tendon autografts, gracilis-semitendinosus autografts, and iliotibial band autografts. As for allografts, the techniques used in pectoralis major reconstruction included Achilles tendon allografts, semitendinosus allografts, fascia Lata allografts, and dermal allografts. Below is a brief overview of the most common autograft and allograft techniques identified, along with a summary of their reported outcomes.
Bone–patellar Tendon (BPT) Autograft
In 2005, Zafra et al. reported on two cases of pectoralis major ruptures, in which direct suturing was deemed impossible owing to fibrosis, scarring, and adhesions [21]. In both cases, a bone–patellar tendon autograft was harvested from the knee, with the patellar tendon end sutured to the musculotendinous junction, and the bone fragment inserted into the humerus using a 4.5 mm cortical screw with a washer. The reconstruction technique proved successful in both instances, as evidenced by increased strength and improved recovery at follow-up. Consequently, the authors recommended this approach when direct tendon suturing is not feasible [24].
Gracilis–Semitendinosus Autograft
An autologous gracilis and semitendinosus tendon, previously harvested from the knee in a standard mode, with the tendons looped to create a standard 4-strand graft, was employed by Schachter et al. [19]. The looped graft’s end was then switched together using No. 2 non-adsorbable suture (FiberWire), with the 4-strand end of the graft, left free. The sutures of the graft’s looped end were then passed through the drill holes, before being tied over the bony bridge [25]. At 1-year follow-up, the patient had returned to their preinjury activity level, with symmetric strength and no cosmetic complaints [25].
Iliotibial Band (ITB) Autograft
In a case study by Decker et al. [16], a chronic pectoralis major was reconstructed using an ITB autograft. After harvest, the free autologous ITB graft was folded over the lateral pectoralis major’s tendon-deficient end using a 5–6 cm graft, covering the anterior and posterior aspects of distal muscle belly, with the remaining 2 cm graft length employed to reconstruct the all-tendinous portion of the pectoralis major. By sequentially passing sutures anteriorly to posteriorly and back again through both graft and pectoral muscle, secure fixation was ensured [16]. Next, three double-loaded anchors were inserted along the humeral insertion site, being equally spaced, with one at both the insertion site’s proximal and distal ends. A more detailed description of the technique is provided in [16]. Postoperatively, the patient was put in a sling immobilizer for 6 weeks, after which a progressive rehabilitation program was initiated. At 2-year follow-up, the patient had returned to full unrestricted activities and reported no instability. The outcome was thus positive and defined as “excellent” according to the Bak et al. outcome classification scale [13].
Achilles Tendon or Fascia Lata Allograft
Fascia Lata and Achilles tendon allografts have been widely used for pectoralis major tendon reconstruction [14,20,24,25]. Allografts eliminate donor-site morbidity and can be easily customized to bridge the gap. However, drawbacks include the risk of disease transmission, delayed graft incorporation, and a higher likelihood of retear [26]. For delayed rupture repairs, Achilles tendon allografts have been applied to both the sternal and clavicular portions. In this procedure, the graft is first tubularized and sewn circumferentially into the tendon stump at the musculotendinous junction, providing an additional 3–4 cm of length. The repair is then completed with direct humeral fixation using metal suture anchors [27].
Semitendinosus Allograft
The largest series involving six patients with sustained pectoralis major tear managed using the semitendinosus allograft approach was published in 2008 by Long et al. [22]. For this technique, a semitendinosus allograft with a number 2 polyethylene suture was placed in whipstitch fashion in each graft’s end. Using the Pulvertaft technique [28], the graft’s suture limbs were weaved through the pectoralis major muscle belly, with three distinct limbs of the muscle’s most lateral aspect, this attachment being reinforced using a number 2 polyethylene suture, sited through the middle limb, with multiple additional sutures practiced to tie the tendon limbs together. This procedure was associated with excellent functional and subjective outcomes at 1-year follow-up, as based on the American Shoulder and Elbow score, constant score, and Visual Analog Scale (VAS) [32]. In a case study reported by Schachter et al. [25], a standard quadruple-strand hamstring graft was employed to bridge a 2cm gap that was left after maximally mobilizing the chronic pectoralis tendon tear. To this end, the gracilis and semitendinosus were harvested befre being looped to build a standard quadruple-strand graft. Next, the graft’s looped end was stitched together using two FiberWire (Arthrex), which were passed through the humeral drill holes, before being tied to the residual bone bridge, with the graft’s four-strand end sutured medially on the pectoralis major muscle. The outcome was deemed positive. At 1-year follow-up, the patient had returned to their preinjury activity level, with symmetric strength and without any cosmetic complaints [25].
Fascia Lata Allograft
In a case study by Sikka et al. [26], a fascia lata allograft was used to reconstruct a nearly 5-year-old pectoralis major tear. Pre-operative MRI indicated the necessity for allograft augmentation to reattach the tendon to the humerus. A freeze-dried fascia lata allograft was utilized for this reconstruction. To secure the allograft to the pectoralis major tendon, a Pulvertaft stitch was applied, along with the insertion of three suture anchors into the humerus. The allograft was then approximated to the humerus using a running Krackow stitch, employing one limb from each of the proximal and distal anchors. The additional suture limbs were passed through the allograft to facilitate a robust, tension-free repair [26]. Following the surgery, the patient was placed in a sling for 4 weeks, after which progressive stretching commenced, including both passive and active motions. At 8 weeks, the patient was permitted to gradually resume lifting and other activities, and by 10 weeks, they were cleared for unlimited activity and weightlifting. At the 18-month follow-up, the patient had returned to full unrestricted activities without any complaints of instability [26].
Dermal Allograft
In cases of tissue retraction and poor tendinous quality, acellular dermal allografts have proven effective as both augmentation and interposition grafts [26,27,30]. Gouk et al. (2021) reported two cases in which an acellular dermal allograft (ADA) was used as an interposition graft to bridge a tissue defect [26]. The ADA was pre-tensioned with two pairs of artery clips, then positioned to overlap the tendinous stump by 2 cm. The medial free edge of the graft was sutured to its body using multiple large, braided, non-absorbable, interrupted sutures. Subsequently, the ADA was secured superiorly to the intact clavicular head tendon in a running stitch and laterally fixed to the humeral footprint of the pectoralis major using three PITON suture anchors, which were attached centrally and 0.5 cm from the lateral borders of the graft [37]. After the procedure, a layered closure was performed, the wound was dressed, and a shoulder immobilizer was applied. At the 12-month follow-up, both patients had returned to work and reported high satisfaction regarding both cosmetic and clinical outcomes [37]. In a retrospective series published by Neumann et al. in 2018, 19 patients with subacute or chronic pectoralis major tears underwent reconstruction using dermal allografts [37]. In these cases, the dermal allograft was sutured to the native pectoralis major tendon and muscle using two FiberWire sutures with the Krackow stitch. For humeral fixation at the anatomic footprint, biocomposite suture anchors, cortical buttons, or a combination of both were employed [37]. In nine patients, stem cells were additionally introduced at the surgical site to enhance healing and reduce scar formation. Analysis of the data revealed a significant improvement in disabilities of the arm, shoulder, and hand (DASH) and VAS scores at a follow-up of 26.4 ± 16.0 months compared to pre-operative values [38].
Post-operative Care and Rehabilitation
Appropriate post-operative care is essential for optimal recovery. The arm should be protected in a sling for at least 6 weeks. Patients must be instructed to avoid active abduction, forward elevation, and external rotation during this period. Gentle passive mobilization can begin at 6 weeks postoperatively to facilitate the recovery of ROM. Concurrently, a gentle periscapular strengthening program and isometric strengthening exercises may be introduced [14].
While pectoralis major injuries are not very common, it must be stressed that their incidence and prevalence have been steadily increasing over the last two decades, especially in the 20–40 years old age group, on account of weight lifting and other high-performance sport activities, including boxing, rugby, football, water skiing, or wrestling [7]. Of note is also that these injuries almost exclusively occurred in men, with only a few cases found in women [24]. The reason for this discrepancy is not precisely clear to us. Perhaps, it can be explained by that high-performance sport is basically a male activity, with a strong male dominance. Conservative treatment can be appropriate in elderly patients, whereas younger patients scarcely tolerate the limitations imposed by pectoralis major ruptures, and surgical interventions are thus required. The meta-analyses of Bak et al. and Bodendorfer et al., involving 112 and 664 pectoralis major ruptures, respectively, revealed that surgical outcomes of tendon repair led to a superior functional outcome, isokinetic strength, isometric strength, cosmesis, and resting deformity, as compared with conservative measures, and the sooner the intervention following the traumatic event, the better the outcome [13,25]. The results emphasize the superiority of early surgical intervention for pectoralis major tears over delayed repair and conservative treatments, particularly regarding pain and function. For chronic tears, the choice between repair and reconstruction depends on factors such as age, activity level, and injury severity. Various fixation techniques, including transosseous suture, suture anchors, and cortical buttons, have demonstrated specific biomechanical outcomes. In addition, outcomes for autograft and allograft reconstructions can be heterogeneous, highlighting the need for a tailored approach considering patient comorbidities. Finally, appropriate post-operative rehabilitation is crucial for optimal recovery and long-term patient satisfaction. Nevertheless, chronic ruptures can turn out challenging for the operating surgeon, given that the mobilization of the musculotendinous junction is more difficult owing to tissue retraction and deep adhesions of the chest wall. The surgeon must thus proceed to blunt dissection while taking great care to avoid damage to the medial and lateral pectoral nerves [14]. The choice between repair versus reconstruction is primarily dependent on the injury location and its chronicity, with the various techniques summarized in Table 3. While various graft types and reconstruction techniques have been reported to provide successful outcomes in patients requiring reconstruction, prospective trials are rather scant. A major outcome of our literature search is the lack of consensus among operating surgeons involved in this surgical domain. In spite the Bak et al. criteria, published in 2000, these principles were scarcely adopted, with a quite heterogeneous presentation of outcome results, rendering comparative analysis rather difficult. Now the time is ripe to conduct larger-scale prospective trials to inform evidence-based recommendation so as to provide surgeons with good work instructions and procedures.
Study Limitations
Our study displays several limitations. The major limitation is its retrospective study design with inherent biases, including limited control over selection bias, recall bias, and missing data. This likely impacts the validity and generalizability of the findings. Moreover, the observational nature of our design leaves the possibility of residual confounding. Still, our study clearly highlights the need for further research in nonoperative and operative treatments of pectoralis major ruptures, in addition to prospective trials to allow for evidence-based recommendations to be published to enable operating surgeons to select the best possible strategy for each individual patient.
Chronic pectoralis major tears or ruptures are challenging for the orthopedic surgeon because of significant tendon retraction, altered anatomy, as well as poor tissue quality. Whereas different repair and graft techniques have so far provided encouraging outcomes in patients suffering from such injuries, based on numerous case reports and small-sized clinical trials retrieved from the scientific literature, there is still a major lack of larger-sized patient series, and prospective studies as well. Orthopedic surgeons should know whether there are superior repair or graft-type techniques to be employed upon operative interventions for optimal outcomes to be achieved. To this end, research must continue, and recommendations must be elaborated for the orthopedic surgeons, ensuring safe interventions for the best possible outcome of every single patient.
Surgical intervention generally improves outcomes for chronic tears, with repair versus reconstruction choices influenced by age and injury severity. The literature does not identify a superior fixation technique, highlighting the need for personalized approaches and effective post-operative rehabilitation.
References
- 1.De Castro Pochini A, Andreoli CV, Belangero PS, Figueiredo EA, Terra BB, Cohen C, et al. Clinical considerations for the surgical treatment of pectoralis major muscle ruptures based on 60 cases: A prospective study and literature review. Am J Sports Med 2014;42:95-102. [Google Scholar | PubMed]
- 2.Patissier P. Traité des Maladies des Artisans. Paris: Jean-Baptiste Baillière; 1882. p. 162-4. [Google Scholar | PubMed]
- 3.Butt U, Mehta S, Funk L, Monga P. Pectoralis major ruptures: A review of current management. J Shoulder Elbow Surg 2015;24:655-62. [Google Scholar | PubMed]
- 4.De Castro Pochini A, Ejnisman B, Andreoli CV, et al. Pectoralis major muscle rupture in athletes: A prospective study. Am J Sports Med 2010;38:92-8. [Google Scholar | PubMed]
- 5.Petilon J, carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: evaluation and management. J AM Acad Orthop Surg 2005;13:59-68. [Google Scholar | PubMed]
- 6.Yu J, Zhang C, Horner N, Ayeni OR, Leroux T, Alolabi B, et al. Outcomes and return to sport after pectoralis major tendon repair: A systematic review. Sports Health 2019;11:134-41. [Google Scholar | PubMed]
- 7.Giordano JR, Klein B, Hershfeld B, Gruber J, Trasolini R, Cohn RM. A review of chronic pectoralis major tears: What options are available? Clin Shoulder Elb 2023;26:330-9. [Google Scholar | PubMed]
- 8.Kakwani RG, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle: Surgical treatment in athletes. Int Orthop 2007;31:159-63. [Google Scholar | PubMed]
- 9.Tsitsilonis S, Panayiotis PE, Athanasios AS, Kourkoulis SK, Vlachos IS, Agrogiannis G, et al. Anabolic androgenic steroids reverse the beneficial effect of exercise on tendon biomechanics: An experimental study. Foot Ankle Surg 2014;20:94-9. [Google Scholar | PubMed]
- 10.ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg 2012;21:412-22. [Google Scholar | PubMed]
- 11.Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma 1980;20:262-4. [Google Scholar | PubMed]
- 12.Bak K, Cameron EA, Henderson IJ. Rupture of the pectoralis major: A meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc 2000;8:113-9. [Google Scholar | PubMed]
- 13.Merolla G, Paladini P, Artiaco S, Tos P, Lollino N, Porcellini G. Surgical repair of acute and chronic pectoralis major tendon rupture: Clinical and ultrasound outcomes at a mean follow-up of 5 years. Eur J Orthop Surg Traumatol 2015;25:91-8. [Google Scholar | PubMed]
- 14.Mooers BR, Westermann RW, Wolf BR. Outcomes following suture-anchor repair of pectoralis major tears: A case series and review of the literature. Iowa Orthop J 2015;35:8-12. [Google Scholar | PubMed]
- 15.Decker KJ, Ghobrial PG, Chudik SC. Pectoralis major tendon reconstruction using an iliotibial band autograft. JSES Rev Rep Tech 2021;1:389-92. [Google Scholar | PubMed]
- 16.Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med 2004;32:1256-62. [Google Scholar | PubMed]
- 17.Carrino JA, Chandnanni VP, Mitchell DB, Choi-Chinn K, DeBerardino TM, Miller MD. Pectoralis major muscle and tendon tears: Diagnosis and grading using magnetic resonance imaging. Skeletal Radiol 2000;29:305-13. [Google Scholar | PubMed]
- 18.Connell DA, Potter HG, Connell DA, Sherman MF, Wickiewicz TL. Injuries of the pectoralis major muscle: Evaluation with MR imaging. Radiology 1999;210:785-91. [Google Scholar | PubMed]
- 19.Rabuck SJ, Lynch JL, Guo X, Zhang LQ, Edwards SL, Nuber GW, et al. Biomechanical comparison of 3 methods to repair pectoralis major ruptures. Am J Sports Med 2012;40:1635-40 [Google Scholar | PubMed]
- 20.Provencher MT, Handfield K, Boniquit NT, Reiff SN, Sekiya JK, Romeo AA. Injuries to the pectoralis major muscle: Diagnosis and management. Am J Sports Med 2010;38:1693-705. [Google Scholar | PubMed]
- 21.Gupton M, Johnson JE, Gupton M, Johnson JE. Surgical treatment of pectoralis major muscle ruptures: A systematic review and meta-analysis. Orthop J Sports Med 2019;7:2325967118824551. [Google Scholar | PubMed]
- 22.Zafra M, Munoz F, Carpintero P. Chronic rupture of the pectoralis major muscle: Report of two cases. Acta Orthop Belg 2005;71:107-10. [Google Scholar | PubMed]
- 23.Schepsis AA, Grafe MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med 2000;28:9-15. [Google Scholar | PubMed]
- 24.Long M, Enders T, Trasolini R, Schneider W, Cappellino A, Ruotolo C. Pectoralis major tendon reconstruction using semitendinosus allograft following rupture at the musculotendinous junction. JSES Open Access 2019;3:328-32. [Google Scholar | PubMed]
- 25.Pulvertaft RG. Tendon grafts for flexor tendon injuries in the fingers and thumb; A study of technique and results. J Bone Joint Surg Br 1956;38:175-94. [Google Scholar | PubMed]
- 26.Zvijac JE, Schurhoff MR, Hechtman KS, Uribe JW. Pectoralis major tears: Correlation of magnetic resonance imaging and treatment strategies. Am J Sports Med 2006;34:289-94. [Google Scholar | PubMed]
- 27.Bodendorfer BM, McCormick BP, Wang DX, Looney AM, Conroy CM, Fryar CM, et al. Treatment of pectoralis major tendon tears: A systematic review and meta-analysis of operative and nonoperative treatment. Orthop J Sports Med 2020;8:2325967119900813. [Google Scholar | PubMed]
- 28.Schachter AK, White BJ, Namkoong S, Sherman O. Revision reconstruction of a pectoralis major tendon rupture using hamstring autograft: A case report. Am J Sports Med 2006;34:295-8. [Google Scholar | PubMed]











