This study highlights the importance of personalized 3D-printed implants in revision THA, especially for managing Paprosky type 3A and 3B acetabular defects with the use of advanced imaging and virtual planning; thereby ensuring optimal implant positioning, better stability and reducing the risk of re-revision.
Dr. Tarun Jayakumar, Department of Orthopaedics, Sunshine Bone and Joint Insitute, KIMS-Sunshine Hospitals, Hyderabad-500016, Telangana, India. E-mail: tarunjaykumar@gmail.com
Introduction: Total hip arthroplasty (THA) is recognized as one of the most effective surgical procedures for the treatment of end-stage hip arthritis. However, the increasing number of primary THA cases has led to a corresponding rise in the frequency of revision surgeries, which are often more complex and challenging due to severe acetabular bone loss. In such cases, managing Paprosky type 3A and 3B defects requires precise implant design and advanced surgical techniques. Standard acetabular augments and anti-protrusio cages are commonly used, but they often fail to provide the necessary stability, leading to re-revision rates as high as 36% within 10 years. This case series explores the efficacy of custom-made 3D-printed acetabular augments and cages in managing severe acetabular bone loss during revision THA.
Case Report: This retrospective case series includes seven patients who underwent revision THA for Paprosky grade 3 acetabular bone loss between January 2023 and April 2024 at two high-volume tertiary care centers. The mean age of the patients was 45 years, with three males and four females included in the study. Pre-operative planning involved advanced imaging techniques, including 3D-computed tomography scans and custom virtual modeling, to design the acetabular components tailored to each patient’s specific anatomical requirements. During the surgeries, custom-made 3D-printed titanium augments and cages were used. These implants were fabricated using in-house software, and the turnaround time from the decision to surgery was approximately 10 days. Post-operatively, the planned 3D model was superimposed on post-operative radiographs to assess implant placement accuracy. The Harris hip score at the final follow-up averaged 69.16, with no signs of implant loosening observed.
Conclusion: Custom-made 3D-printed acetabular augments and cages offer a reliable and cost-effective solution for managing severe acetabular bone loss in revision THA. Despite the small sample size and short follow-up period, the results demonstrate the potential of these custom implants to improve outcomes in complex acetabular reconstructions. Further studies with larger sample sizes and longer follow-up periods are needed to confirm these findings and establish long-term efficacy.
Keywords: Acetabular bone loss, 3D reconstruction, custom augments, custom cages, patients-specific implant, 3D-printing.
Total hip arthroplasty (THA) is one of the most successful surgical procedures for managing end-stage hip arthritis. Despite its success, approximately 12% of THAs require revision within 10 years, and only 75% demonstrate revision-free survival at 15–20 years [1]. As the volume of primary THA cases continues to rise, the burden of revision THAs is expected to increase significantly in the coming years. Each subsequent revision, being more complex, is associated with increasing challenges in managing acetabular bone loss [2]. The classification system proposed by Paprosky et al. is widely used and highly reliable for categorizing and managing acetabular bone loss [3]. Managing type 3A and 3B defects requires careful pre-operative planning, precise implant design, advanced surgical skills, and sophisticated technology. Anti-protrusio cages and standardized acetabular augments are commonly used in these situations. However, the amount of bone loss and the quality of available bone stock significantly affect the stability of acetabular implants. The re-revision rate of acetabular components 10 years after revision THA is reported to be as high as 20–36%, suggesting that these cases may require more than just standard augments or cages [2]. Given the variability in defect morphology and patient anatomy, custom-made implants may offer a superior alternative for managing Paprosky type 3A and 3B defects [4]. There is limited evidence to suggest that custom-made acetabular implants offer good accuracy and have a short- to mid-term survival rate. However, existing studies have mainly focused on custom-made acetabular components and not on augments and cages. Moreover, these studies often do not report on the cost and time required to manufacture these implants [5-10]. In our experience, these factors are significantly high, which limits the widespread use of custom-made augments for managing bone loss. This study aimed to assess the functional outcomes and complications of patients operated with custom 3D-printed acetabular augments or cages in a revision scenario with severe acetabular bone loss. This study also presents the approach to planning and manufacturing these implants and illustrates various cases managed using this technique.
This retrospective multicenter cohort study included seven cases of revision THA with Paprosky grade 3 acetabular bone loss, [3] operated between January 2023 and April 2024 at two high-volume tertiary care arthroplasty centers after obtaining ethical committee approval. All surgeries were performed with patients in the lateral position using a posterior approach. Following surgery, patients were monitored in the surgical intensive care unit for 24 h before being transferred to the ward. They were mobilized with full weight-bearing and provided with physiotherapy that focused on strengthening the abductor and quadriceps muscles, hip precautions, toilet training, and avoiding hip internal rotation before discharge. During follow-up visits, patients underwent a comprehensive clinical assessment; including evaluation of surgical site healing, pain, function, range of motion, and documentation of the Harris hip score (HHS). Any complications and their effects on the patients’ routine activities were recorded both intraoperatively and post-operatively. Post-operative radiographs were taken at monthly follow-up visits and compared with the immediate post-operative radiographs for any signs of loosening.
Pre-operative planning
Routine Pelvis-anteroposterior (AP), lateral and Judet view radiographs were obtained in all patients (Fig. 1). In addition, as part of our planning for THA, a 3D-non-contrast computed tomography (CT) scan with 1 mm slice thickness and CT-metal artifact reduction sequence in cases where previous implants were present were done for all patients.
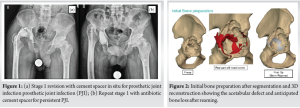
All radiographs and CT scans were provided in digital imaging and communications in medicine format, where the pelvis model was reconstructed in 3D using MySegmenter (Jajal Medical Services, Vadodara, India) software. The radiological data were processed slice by slice, followed by automatic and manual editing to construct the final virtual 3D model. This model was then input into “MyDesign (Jajal Medical Services, Vadodara, India) software, which created landmarks and planes. A virtual acetabular sphere was constructed and appropriately oriented with respect to the Center of rotation and available bone stock (Fig. 2). After virtual acetabular reaming, the cup was placed in the specified orientation, and the remaining defect was reanalyzed to design the final augment or cage. Based on the processed CT scan data, the quality and thickness of the available bone stock were analyzed, and the same software was used to manually design a combination of multiple locking screws. Great care was taken to create space for placing screws through the acetabular component and to avoid intersecting screw trajectories (Fig. 3 and 4)

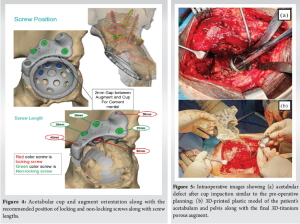
Using the “Flashforge Guider 2” (Zhejiang Flashforge 3D technology Co, Ltd, China), basic 3D-plastic models of the augments, anatomical pelvis, and planned cup were printed. These models were sterilized using ETO and provided during surgery for intraoperative comparison, assessment of accurate fit, and intraoperative practice (Fig. 5). The “Formlab 3B SLA” (Formlabs, Somerville, MA) printer was used to print the final 3D-titanium porous augments and cages, which were then autoclaved before surgery. The total turnaround time from the decision to proceed with surgery to the availability of the final implants and practice models at the respective institutes was 10 days. The mean cost of this entire process was 1000 USD, with variations of up to 200 USD depending on the complexity of the deformity and the size of the augments or cages required. Post-operatively, the planned 3D model was superimposed on the post-operative AP and lateral radiographs to assess the accuracy of the custom-made augments, acetabular cups, and screw placements. The center of rotation and limb lengths were also studied and compared with the opposite side (Fig. 6 and 7).

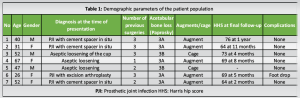
The study included a total of seven patients, three male and four female, with a mean age of 45 years (Standard deviation [SD] = 13.9, range: 26–67). After discharge, six out of the seven patients were available for follow-up, with a mean maximum follow-up period of 7 months (range: 1–12 months). Despite this, all patients were still included, as the main goal of our study is to demonstrate the process of planning, manufacturing, and using custom-made 3D implants. Custom-made acetabular augments were used in five patients, while cages were used in the remaining two (Table 1).
Functional and radiological outcomes
The mean HHS at the final follow-up was 69.16 (SD = 4.8, range: 61–76). When superimposed over the pre-operative plan provided by the software, post-operative radiographs demonstrated 100% accuracy in all cases concerning the position of the cup as well as the augment or cage. Although the direction and length of the screws were not 100% accurate, they were highly consistent with the plan. None of the patients exhibited any signs of implant loosening on the radiographs taken up to the past follow-up.
Complications
One 26-year-old female patient with a grade 3A acetabular defect, who was treated with a custom-made acetabular augment, developed a foot drop on the operated side immediately post-operatively. At her past follow-up (5 months post-operatively), she showed no recovery in ankle dorsiflexion power. However, she is comfortably ambulating outdoors with an ankle-foot orthosis and a stick. No other complications were noted perioperatively or post-operatively.
Revision of the acetabular component in Paprosky type 3 defects is challenging due to the variability in patient anatomy, loss of landmarks, poor supporting bone stock, and soft tissue complications. The high reported failure rates emphasize the need for better management of bone loss and optimal use of available bone stock to achieve a stable and durable structure [8]. A single surgical technique that addresses all these challenges has yet to be developed. Cemented acetabular components over impaction bone grafting, with or without a reconstruction cage or metal augment, is one of the most widely used techniques to manage acetabular bone loss [11-13]. However, its use for larger segmental and uncontained acetabular defects is associated with high failure rates [14-16]. The use of uncemented acetabular components with or without high porosity, multiple screws, modular augments, or cages is another popular approach. Nevertheless, it faces similar challenges in Paprosky type 3 scenarios [8]. Baauw et al. [5] systematically analyzed various available options for reconstructing large acetabular bone defects, concluding that custom-made, patient-specific implants offer superior results in these challenging situations. Several studies have demonstrated good short- to mid-term outcomes with custom-made acetabular components in terms of re-establishing the center of rotation and component positioning [2,7,10]. Some studies also report favorable outcomes with custom-made augments and cages [8,17]. Kong et al. [17] showed that custom-made titanium augments combined with tantalum acetabular cups yielded good mid-term results in terms of function and restoration of acetabular centers. Zampelis and Flivik demonstrated the good accuracy of custom-made implants and component positioning when compared to pre-operative planning [8]. These studies have compared post-operative CT scans with pre-operative CT scans to determine the accuracy of component positioning and reestablishment of the center of rotation (COR) and found similar results to our study. We believe that although CT is more accurate for comparing and determining the implant and component position, it is not always practical or necessary. Zhang et al. [18] conducted a retrospective study of 31 patients who underwent surgery with custom-made acetabular augments, using only AP radiographs instead of CT scans. They utilized surgical simulation to accurately reconstruct the 3D implants, which is similar to our pre-operative planning approach. Moreover, they also provided sterile pelvis and augment models intraoperatively for accurate placement. The present study aligns with this approach, suggesting that when a virtual 3D model is accurate and the sterile pelvis and augment model is available intraoperatively for anatomical comparison, implant placement becomes much easier and more accurate. Therefore, post-operative radiographs are sufficient to determine the success of the planned execution. In addition, we used our software to create a superimposition of the virtual models with the post-operative X-rays to assess the accuracy of positioning and establishment of the COR. This technique significantly enhances the information obtained from radiographs, further reducing the need for post-operative CT scans. While the implant position and component orientation were highly accurate, the screw length and direction varied slightly from the plan. Similar results have been reported in the literature [18]. We attribute this discrepancy to the marginal play available in the drill direction and the locking of the screw holes in the augments. This play was intentionally designed to avoid intersecting with the acetabular screws, whose direction is entirely up to the surgeon’s judgment. Moreover, in the event of a minor variance in the position of the components compared to the plan, the flexibility of the system permits the surgeon to still secure the screws in the most optimal bone available. Given that the custom-made implants consistently provided a secure hold, we do not see this variance as inaccurate, but rather as a demonstration of the system’s adaptability, making it even more practical and beneficial. None of our patients showed any radiological signs of loosening or migration at their past follow-up visit. All patients exhibited significant post-operative functional improvement and are independent ambulators with or without support. These results are consistent with those published in the literature [2,7,10,17,18]. Studies of custom-made acetabular cages and augments, as well as 3D-printed acetabular components, have not reported the cost and time required for their manufacturing. In our case series, the mean cost and time for manufacturing the implants and making them available at the respective institutes were 1000 USD and 10 days, respectively. We believe that this is significantly lower than the cost and time associated with producing custom-made acetabular components, at least in our practice. To the best of our knowledge, this represents one of the best value-for-money products available in the market. We attribute this efficiency to our in-house developed software and the use of titanium instead of tantalum, the former of which has been shown to perform as well as the latter. The small sample size and short follow-up duration are some of the limitations of the present study. However, the detailed explanation of pre-operative planning, implant manufacturing, execution, and the variety of cases managed using this technique are its strengths. We plan to publish the mid-term and long-term outcomes of our cases and explore other applications of our technology in due course.
Our technique of 3D-printed custom-made acetabular augments and cages is a reliable, flexible, and cost-effective option for managing severe acetabular bone loss during revision THA. Long-term follow-up studies with larger sample sizes are required to determine whether this technique can withstand the test of time.
Custom-made 3D-printed acetabular augments and cages are a viable and cost-effective solution for managing severe acetabular bone loss in complex revision total hip arthroplasty (THA). These implants enable precise restoration of anatomical landmarks, improve surgical accuracy, and enhance functional outcomes, even in cases with significant bone loss or distorted anatomy.
References
- 1.Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019;393:647-54. [Google Scholar | PubMed]
- 2.Di Laura A, Henckel J, Hart A. Custom 3D-printed implants for acetabular reconstruction: Intermediate-term functional and radiographic results. JB JS Open Access 2023;8:e22.00120. [Google Scholar | PubMed]
- 3.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 1994;9:33-44. [Google Scholar | PubMed]
- 4.Baauw M, Van Hellemondt GG, Van Hooff ML, Spruit M. The accuracy of positioning of a custom-made implant within a large acetabular defect at revision arthroplasty of the hip. Bone Joint J 2015;97:780-5. [Google Scholar | PubMed]
- 5.Baauw M, Van Hooff ML, Spruit M. Current construct options for revision of large acetabular defects: A systematic review. JBJS Rev 2016;4:e2. [Google Scholar | PubMed]
- 6.Weber M, Witzmann L, Wieding J, Grifka J, Renkawitz T, Craiovan B. Customized implants for acetabular Paprosky III defects may be positioned with high accuracy in revision hip arthroplasty. Int Orthop 2019;43:2235-43. [Google Scholar | PubMed]
- 7.Durand‐Hill M, Henckel J, Di Laura A, Hart AJ. Can custom 3D printed implants successfully reconstruct massive acetabular defects? A 3D‐CT assessment. J Orthop Res 2020;38:2640-8. [Google Scholar | PubMed]
- 8.Zampelis V, Flivik G. Custom-made 3D-printed cup-cage implants for complex acetabular revisions: Evaluation of pre-planned versus achieved positioning and 1-year migration data in 10 patients. Acta Orthop 2021;92:23-8. [Google Scholar | PubMed]
- 9.Wessling M, Gebert C, Hakenes T, Dudda M, Hardes J, Frieler S, et al. Reconstruction of Paprosky III defects with custom-made implants: Do we get them in the correct position? : Short-term radiological results. Bone Joint J 2022;104-B:1110-7. [Google Scholar | PubMed]
- 10.Romagnoli M, Zaffagnini M, Carillo E, Raggi F, Casali M, Leardini A, et al. Custom-made implants for massive acetabular bone loss: Accuracy with CT assessment. J Orthop Surg Res 2023;18:742. [Google Scholar | PubMed]
- 11.Sheth NP, Nelson CL, Springer BD, Fehring TK, Paprosky WG. Acetabular bone loss in revision total hip arthroplasty: Evaluation and management. J Am Acad Orthop Surg 2013;21:128-39. [Google Scholar | PubMed]
- 12.Slooff TJ, Schimmel JW, Buma P. Cemented fixation with bone grafts. Orthop Clin North Am 1993;24:667-77. [Google Scholar | PubMed]
- 13.Abolghasemian M, Sadeghi Naini M, Tangsataporn S, Lee P, Backstein D, Safir O, et al. Reconstruction of massive uncontained acetabular defects using allograft with cage or ring reinforcement: An assessment of the graft’s ability to restore bone stock and its impact on the outcome of re-revision. Bone Joint J 2014;96-B:319-24. [Google Scholar | PubMed]
- 14.Buttaro MA, Comba F, Pusso R, Piccaluga F. Acetabular revision with metal mesh, impaction bone grafting, and a cemented cup. Clin Orthop Relat Res 2008;466:2482-90. [Google Scholar | PubMed]
- 15.Bonnomet F, Clavert P, Gicquel P, Lefèbvre Y, Kempf JF. Reconstruction by graft and reinforcement device in severe aseptic acetabular loosening: 10 years survivorship analysis. Rev Chir Orthop Reparatrice Appar Mot 2001;87:135-46. [Google Scholar | PubMed]
- 16.van Haaren EH. Heyligers IC, Alexander FG, Wuisman PI. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br 2007;89:296-300. [Google Scholar | PubMed]
- 17.Kong K, Zhao C, Chang Y, Qiao H, Hu Y, Li H, et al. Use of customized 3D-printed titanium augment with tantalum trabecular cup for large acetabular bone defects in revision total hip arthroplasty: A midterm follow-up study. Front Bioeng Biotechnol 2022;10:900905. [Google Scholar | PubMed]
- 18.Zhang Y, Gao Z, Zhang B, Du Y, Ma H, Tang Y, et al. The application of custom-made 3D-printed titanium augments designed through surgical simulation for severe bone defects in complex revision total hip arthroplasty. J Orthop Traumatol 2022;23:37. [Google Scholar | PubMed]













