OAT plugs transplanted in knees remain with normal cartilage 18 years after primary OAT surgery.
Dr. Takahiro Maeda, Department of Orthopedic Surgery, Shiga Medical Center for Children, Postal Address: 30-7-5 Moriyama, Moriyama City, Shiga Prefecture, 524-0022, Japan. E-mail: mae.taka.711@gmail.com
Background: Despite the good clinical outcomes of osteochondral autograft transplantation (OAT), reports of re-arthroscopic findings after OAT have been limited to short-term, and there are no reports of findings after long-term follow-up. This is the first report that describes re-arthroscopic findings long-term after OAT.
Case Report: A male patient underwent OAT on the lateral femoral condyle (LFC) of the knee and lateral meniscus (LM) repair at the age of 45. Eighty years after the primary surgery, he underwent re-arthroscopy because of cartilage injury on the medial femoral condyle (MFC) and LM tear. The re-arthroscopic findings showed the retained OAT plugs on LFC and severe damage of LM. After OAT on the LFC and meniscectomy of LM was performed, his knee symptoms improved, so the LFC that had undergone OAT 18 years previously was considered to be on a good clinical course.
Conclusion: OAT plugs were retained at the long-term follow-up while the repaired LM was severely damaged. The structural robustness of OAT was thought to be responsible for good long-term clinical outcomes.
Keywords: Osteoarthritis, osteochondral autograft transplantation, ICRS grade, arthroscopic findings.
Osteochondral autologous transplantation (OAT) was first reported as a method for treating articular cartilage defects in the knee by Matsusue et al. in 1993 [1] and the clinical outcome of OAT is satisfactory in the both short- and long-term [2- 7]. However, reports of re-arthroscopic findings of the knees after OAT have been limited to one or a few years postoperatively, and there are no reports of re-arthroscopic findings after a long-term follow-up. Here, we report on re-arthroscopic findings 18 years after OAT for the lateral femoral condyle (LFC). The patient was informed that data including any accompanying images from the case would be submitted for publication, and gave his consent.
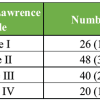
A 63-year-old male presented to our hospital with symptoms of left knee pain and catching. He had no past medical history except for arthroscopic surgery on his left knee. At the age of 45, he had undergone OAT for the left LFC cartilage defect and lateral meniscus (LM) repair for a horizontal tear (Fig. 1). At that time his lower limb had a neutral coronal alignment (femorotibial angle; 178.4°/174.2°, joint line convergence angle; 2.3°/0.6°) and the Japanese Orthopaedic Association (JOA) score for knee osteoarthritis was 80 (walking; 25, stairs; 20, range of motion; 30, and joint effusion; 5) [8]. The cartilage lesion in LFC was rated International Cartilage Repair Society (ICRS) grade 4 with an area of 160 square mm. Three donor plugs with a diameter of 6.5 mm were harvested from the non-weight-bearing area of the lateral side of the trochlear groove with MOSAICPLASTY (Smith & Nephew, Watford, UK) and transplanted to the lesion. Second-look arthroscopy performed 14 months after OAT revealed that the transplanted osteochondral plug was integrated with the surrounding cartilage, and the repaired LM had healed well. The ICRS cartilage repair assessment score was 12 (survival: 4, integration: 4, and macroscopic appearance: 4) and the JOA score was 100, a perfect score.
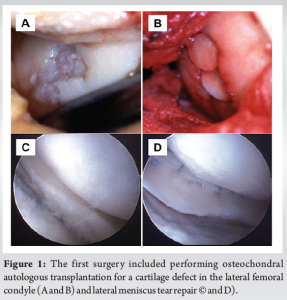
A physical examination conducted 18 years after OAT revealed a slight swelling in the left knee and tenderness of the medial joint space. The left knee had a reduced range of motion (ROM) of 0°–110°, whereas the right knee had a ROM of 0°–150°. However, no joint instability was detected. Magnetic resonance imaging (MRI) showed a cartilage defect in the medial femoral condyle (MFC) and disappearance of the LM, but the transplanted osteochondral plug in the LFC still remained (Fig. 2).
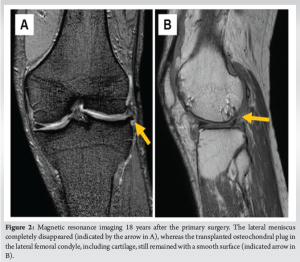
We performed re-arthroscopy and found recurrent LM tear and cartilage defect in the MFC, which corresponded to an ICRS grade 4 lesion. Therefore, we performed a partial meniscectomy of the LM and OAT of the MFC. The transplanted osteochondral plug in the LFC remained, and the ICRS cartilage repair assessment score was 10 (survival: 3, integration: 4, and macroscopic appearance: 3) (Fig. 3). In addition, the non-weight-bearing area of the lateral side of trochlear groove, which was the donor site of the primary OAT, was replaced with fibrocartilage-like tissue, and no apparent impingement was observed.
A year after the latest OAT, the patient had no symptoms in his knee including ROM; thus, he enjoyed playing tennis as a hobby.
OAT is an established joint-preservation surgery for patients with chondral lesions in the knee with satisfactory long- and short-term clinical outcomes [2-7]. Despite the good clinical outcomes, reports of re-arthroscopic findings after OAT are limited for the short term. Nakagawa reported on re-arthroscopic findings on recipient sites 1 year post-OAT. The recipient site surfaces were smooth, with an ICRS cartilage repair assessment score of ≧10 in 30 of the 40 patients [9]. Gudas also reported second-look arthroscopic results 3 years after OAT with smooth and strong cartilage of osteochondral grafts in the MFC. In their case, the gaps between the graft plugs were filled with stable fibrocartilage reparative tissue without degenerative changes of the transplanted cartilage surface [5]. Barber reported re-arthroscopic and histologic findings of the knee 2–5 years post-OAT [6]. They performed re-arthroscopy and needle biopsy for nine patients; of these, seven showed complete healing, whereas two showed partial healing. Needle biopsy revealed normal hyaline cartilage in patients who had healed completely. As in these reports, OAT has been reported to have good cartilage findings at rescoping in the short term, and in our case, the cartilage findings were good even after 18 years, confirming that the clinical results of OAT are satisfactory in the long term. Donor site morbidity such as pain in the patellofemoral joint (PFJ) is one of the adverse events of concern in OAT. While donor sites in healthy knees have been reported to be more prone to symptoms than ipsilateral knee donors, symptoms or revision surgeries to donor sites are reported to be caused by arthrofibrosis rather than abnormal cartilage in the donor site [10-12]. In our case, donor sites were filled with fibrocartilage-like tissue, and no significant arthropathic changes in PFJ were observed at 18 years after OAT. Meniscus repair tends to improve knee function and symptoms such as swelling, pain, and difficulty in walking and stair climbing, but it has a higher re-operation rate than partial meniscectomy [13]. The failure rate of meniscus repair in the long term is reported 22.3–30.1% whereas that in the short term is reported 17–19% [14,15], and re-injury after a long-term meniscus repair can occur with a certain probability. In the present case, the transplanted plug in the LFC was retained while the repaired LM was severely damaged. This structural strength of OAT is considered to result in good short- and long-term clinical outcomes.
We reported on re-arthroscopic findings of the knee 18 years post-OAT and LM repair. The transplanted osteochondral plug was well integrated, and the cartilage remained; however, the repaired LM was severely damaged. Therefore, it can be concluded that OAT osteochondral plugs remain well for a long time after OAT, and this supports the findings of good clinical outcomes of OAT.
This article describes the status of osteochondral plugs after long-term follow-up of OAT and provides insight to support the good clinical outcomes of OAT for the long term.
References
- 1.Matsusue Y, Yamamuro T, Hama H. Arthroscopic multiple osteochondral transplantation to the chondral defect in the knee associated with anterior cruciate ligament disruption. Arthroscopy 1993;9:318-21. [Google Scholar | PubMed]
- 2.Cognault J, Seurat O, Chaussard C, Ionescu S, Saragaglia D. Return to sports after autogenous osteochondral mosaicplasty of the femoral condyles: 25 cases at a mean follow-up of 9 years. Orthop Traumatol Surg Res 2015;101:313-7. [Google Scholar | PubMed]
- 3.Solheim E, Hegna J, Strand T, Harlem T, Inderhaug E. Randomized study of long-term (15-17 years) outcome after microfracture versus mosaicplasty in knee articular cartilage defects. Am J Sports Med 2018;46:826-31. [Google Scholar | PubMed]
- 4.Gudas R, Gudaite A, Pocius A, Gudiene A, Čekanauskas E, Monastyreckiene E, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med 2012;40:2499-508. [Google Scholar | PubMed]
- 5.Gudas R, Kalesinskas RJ, Kimtys V, Stankevičius E, Toliušis V, Bernotavičius G, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 2005;21:1066-75. [Google Scholar | PubMed]
- 6.Barber FA, Chow JC. Arthroscopic osteochondral transplantation. Arthroscopy 2001;17:832-5. [Google Scholar | PubMed]
- 7.Solheim E, Hegna J, Øyen J, Harlem T, Strand T. Results at 10 to 14 years after osteochondral autografting (mosaicplasty) in articular cartilage defects in the knee. Knee 2013;20:287-90. [Google Scholar | PubMed]
- 8.Okuda M, Omokawa S, Okahashi K, Akahane M, Tanaka Y. Validity and reliability of the Japanese orthopaedic association score for osteoarthritic knees. J Orthop Sci 2012;17:750-6. [Google Scholar | PubMed]
- 9.Nakagawa Y, Mukai S, Yabumoto H, Tarumi E, Nakamura T. Serial changes of the cartilage in recipient sites and their mirror sites on second-look imaging after mosaicplasty. Am J Sports Med 2016;44:1243-8. [Google Scholar | PubMed]
- 10.Andrade R, Vasta S, Pereira R, Pereira H, Papalia R, Karahan M, et al. Knee donor-site morbidity after mosaicplasty - a systematic review. J Exp Orthop 2016;3:31. [Google Scholar | PubMed]
- 11.Bexkens R, Ogink PT, Doornberg JN, Kerkhoffs GM, Eygendaal D, Oh LS, et al. Donor-site morbidity after osteochondral autologous transplantation for osteochondritis dissecans of the capitellum: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2017;25:2237-46. [Google Scholar | PubMed]
- 12.Nakagawa Y, Mukai S, Setoguchi Y, Goto T, Furukawa T, Nakamura T. Clinical outcomes of donor sites after osteochondral graft harvest from healthy knees. Orthop J Sports Med 2017;5:2325967117732525. [Google Scholar | PubMed]
- 13.Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy 2011;27:1275-88. [Google Scholar | PubMed]
- 14.Petersen W, Karpinski K, Bierke S, Müller Rath R, Häner M. A systematic review about long-term results after meniscus repair. Arch Orthop Trauma Surg 2022;142:835-44. [Google Scholar | PubMed]
- 15.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med 2012;40:459-68. [Google Scholar | PubMed]