Although MOW-HTO has least complications, a thorough knowledge about the surrounding soft tissue and vigilance toward stretch injuries is paramount.
Dr. Aniket Wagh, Department of Orthopaedic Surgery, Murup Hospital, 2-52, 3 Ga Jungang-dong, Masanhappo-gu, Changwon-si, Gyeongnam 631-423, South Korea. E-mail: muruphospital@gmail.com
Introduction: Medial open wedge-high tibial osteotomy (MOW-HTO) is a standard procedure for treating moderate varus arthritis in active adults. The reason for its popularity is having lesser complications than other types of HTO. However, it is not devoid of challenges. We report tibial nerve injury in a MOW-HTO which is a rare complication not reported much in the past.
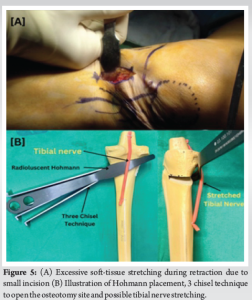
Case Report: A 56-year-old female was operated with MOW-HTO using TomoFix plate for medial joint arthritis and varus malalignment. She developed signs of tibial nerve injury, namely inability to flex the great toe and paresthesia over posterolateral leg and sole of foot. The nerve conduction velocity study confirmed tibial nerve damage with moderate axonotmesis. The patient was treated conservatively with electrical stimulation, interferential current therapy, physiotherapy, and pregabalin. The osteotomy outcome was good with complete union and good angle correction. At the end of 14 years, the motor function was fully recovered, but the patient still had residual paresthesia. After eliminating all other possible causes, the authors concluded that the etiology of the nerve damage was stretch injury. Smaller incisions are related to excessive retraction leading to unreasonable stretching of the soft tissues and nerves. To avoid such injuries during MOW-HTO, the authors propose an adequate length of incision along with other steps like subperiosteal Hohmann placement to protect neurovascular structures, flexing the knee during the procedure, maintaining posterior position of the plate, and using proper size screws. The main goal of this study is to make surgeons conscious about this rare but possible complication of MOW-HTO.
Conclusion: Surgeons need to be aware about this rare complication in MOW-HTO surgery and should be vigilant in recognizing its post-operative signs.
Keywords: Medial open wedge, high tibial osteotomy, tibial nerve, high tibial osteotomy, neurovascular complication, osteoarthritis, varus malalignment, axonotmesis.
High tibial osteotomy (HTO) is established as the surgery of choice in young patients with arthritis and a varus malalignment [1]. These include lateral closing wedge (LCW), medial open wedge (MOW), and dome osteotomy [2]. MOW-HTO first described by Jackson and Waugh in 1961 has shown promising results among these [3]. The osteotomy is performed above the tibial tubercle and a calculated sized wedge opening is done. This corrects the mechanical axis, shifting it laterally, reducing the medial pain, and improving the knee function. MOW is known to have lesser complications as compared to LCW as the later requires dissection of lateral tibia and fibula osteotomy which increases the risk of peroneal nerve injury [4]. Furthermore, there are newer locking plates, especially designed for MOW issuing a rigid fixation and allowing early weight bearing [5,6]. There have been reports of popliteal artery injury [7,8] and even peroneal nerve injury [9]. However, to our knowledge, only one case of tibial nerve injury has been reported after this surgery till now [10]. In this study, we report a similar rare case of tibial nerve injury after MOW-HTO and investigate the etiology and prognosis.
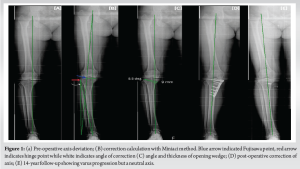
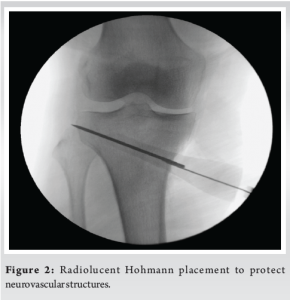
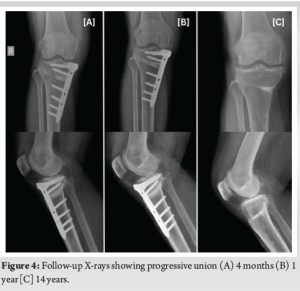
A 56-year-old female was diagnosed with medial compartment osteoarthritis (Kellgren-Lawrence grade 3) with varus malalignment (Fig. 1a) and medial meniscus posterior root tear. The patient was planned for arthroscopic medial meniscus root repair and MOW-HTO. The planned correction angle was 8.5° with opening wedge thickness of 9 mm (Fig. 1c). Meniscus root was repaired with a suture anchor. For the osteotomy, a small vertical incision was taken over the medial aspect of the proximal tibia below the joint line and midway between anterior and posteromedial margins of tibia. The pes anserinus tendon was identified and superficial medial collateral ligament (sMCL) partially released at that level. A radiolucent Hohmann retractor was strategically placed from under the released sMCL going posteromedial to protect the neurovascular structures. The Hohmann was placed obliquely all the way along the osteotomy line which was directing toward the tip of fibula under fluoroscopy guidance (Fig. 2). Osteotomy path was positioned using 2 K-wires starting just above pes anserinus level at the medial metaphyseal flare of tibia aiming toward the tip of fibula. Once sure, osteotomy was done was oscillating saw and opened using “3 chisel technique.” The correction was planned using Miniaci technique at Fujisawa point, i.e., 62% of tibial plateau as measured from medial side (Fig. 1b). Care was taken to maintain the lateral hinge. The open wedge was filled with tricalcium phosphate (TCP) bone substitute toward the cortex to prevent post-operative collapse and loss of correction. Osteotomy site was secured with locking TOMOFIX plate. Drilling for screws was done carefully not to cross far beyond the distal cortex. The TCP and the plate were purposely kept postero-medially and fixed in knee extension to maintain the posterior tibial slope angle. The procedure was uneventful. On post-operative day 1, the patient complained of decreased sensation over the posterolateral area of leg and sole of foot along with generalized tingling in the lower limb with inability to flex the great toe (Video 1a). Rest of the neurovascular examination was normal. Post-operative X-rays showed good fixation with no protruding hardware. Magnetic resonance imaging of lumbosacral spine was done which showed mild disc bulge at L4-L5 and L5-S1 with no nerve compression or canal stenosis. This could not be related to patient’s symptoms. Nerve conduction velocity (NCV) test was done at 3 weeks which showed right tibial nerve injury pattern around knee level with moderate axonotmesis (Fig. 3a). Since the nerve was in axonotmesis, a conservative trial with a close follow-up was planned for the patient. The patient was given electrical stimulation therapy, interferential current therapy, physiotherapy, and pregabalin course. On 2-month follow-up, there was no pain. The patient was mobilizing full weight bearing. However, there was no neural recovery clinically. On 4-month and 1-year follow-up, great toe flexion power was 2/5 and there was a 50% subjective improvement in sensory complaints. The X-rays showed good progressive union (Fig. 4). Unfortunately, after this, the patient was lost to follow-up and came back to us after 5 years (6-year post-surgery). The patient had the osteotomy plate removed at another hospital. At this time, the patient had persistent paresthesia (subjectively around 40%) and great toe flexion was 4/5. The last follow-up is 14-year post-surgery where the motor function has recovered completely with some residual paresthesia (Video 1b).
However, the patient complained of discomfort after walking for long distances. The NCV at this stage was suggestive of chronic tibial nerve injury (Fig. 3b). Long leg X-ray showed some loss of correction with axis passing through 50% point (Fig. 1e), but the patient had no arthritis-related complaints.

MOW-HTO is known to be the safest among different types of HTO. It has become the osteotomy of choice for varus arthritis unless contraindicated. Some well-documented complications of this procedure are stiffness, implant failure, infection, thrombosis, and lateral cortex fracture [11,12]. Another technical complication is increase in posterior tibial slope angle which can cause future degeneration of anterior cruciate ligament [13]. Neurovascular injuries are the least common entities when it comes to MOW-HTO. Among the few reported neurovascular injuries, deep peroneal nerve (DPN) and popliteal artery are common. The DPN is a branch of common peroneal nerve which perforates the anterior intermuscular septum and runs between tibialis anterior and extensor muscles of the toe supplying them [14]. Cases of DPN injury during HTO have been reported in the past either due to protruding distal screws or trauma during drilling for the screws [15]. The popliteal artery lies anterior to the popliteal vein in the popliteal fossa making it the closest neurovascular structure while performing the osteotomy [16]. There have been reports of popliteal artery injury while using the saw during the osteotomy [17]. The tibial nerve being posterior to the popliteal vein naturally is the least likely to get injured [16]. Evidently so, till now, only one such case has been reported which was found out to be because of a long screw in the first distal screw hole [10]. Although nerve injuries are uncommon in MOW-HTO, one needs to have a thorough knowledge about the neurovascular structures around the proximal tibia [18]. Surgical steps need to be modified according to these anatomical considerations. Tibial nerve is the medial terminal branch of the sciatic nerve supplying the flexor muscles of ankle and toes including gasto-soleus, flexor hallucis longus, abductor hallucis, and the intrinsic muscles of the foot [14]. Its root value is L4-S3 and it gives cutaneous supply to the posterolateral part of leg, lateral foot, and sole of foot. In the leg, it passes over tibialis posterior and flexor digitorum longus in the midline, eventually passing under the flexor retinaculum and bifurcating into the lateral and medial plantar nerves. In this case, the symptoms were correlating to tibial nerve supply. Ruling out intervertebral disc herniation compressing the L5 and S1 root was important for documentation as peripheral nerve injury and lumbar disc herniation can mimic each other’s symptom [19]. The NCV revealed moderate axonotmesis which is characterized by disruptive lesion of the axon and its myelin coating. However, the anatomical shape of the nerve is preserved as the perineurium and epineurium are intact. These collagen coverings help the growth of axons during regeneration process, giving such injuries a good prognosis [20]. Thus, a conservative management with a close follow-up was decided for the patient. This included physiotherapy, electrical stimulation therapy, and pregabalin course. Physiotherapy comprised of mobilizing the scar and surrounding tissues, active muscle exercises to pump away the edema, massages to stimulate the muscles [21]. Partial weight bearing was started after 4 weeks and full weight bearing after 6 weeks of surgery. Electrical stimulation is known to enhance reinnervation and accelerate the axonal regeneration process in neural injuries [21]. Similarly, as concluded by Celik et al., pregabalin treatment in axonotmesis improves nerve regeneration by activating anti-inflammatory cytokine transforming growth factor beta-1 as evidenced in their histological studies [22]. Unlike the previously reported case, there were no protruding screws. The surgery was uneventful. There was no post-operative hematoma, the tourniquet time was well within normal bounds, there was no awkward patient positioning. With the help of the above points, a diagnosis of exclusion was reached to be of a stretch injury. The most logical reason for a stretch injury in this case was small size of incision needing excessive retraction. Peripheral nerves are known to get iatrogenic stretch injuries due to excessive and improper retraction. Antoniadis et al. in their study stated that osteotomy is one of the high-risk procedures and popliteal fossa is one of the high-risk sites for iatrogenic nerve injury [23]. Fig. 5 shows excessive stretching of soft tissues during retraction due to small incision, which might result in possible traction on tibial nerve while opening of the osteotomy with chisels. However, literature also says that tibial nerve is one of the least affected lower limb nerves by stretch injury. This is believed to be due to the larger size of the nerve, more numbers of fascicles, and higher amount of extra-fascicular tissue [24]. This further makes our case report a rare occurring. At 14-year follow-up, the patient still had partial residual paresthesia while the great toe flexion was recovered completely. She experienced discomfort on running or long-distance walking. This outcome coincides with a study by Retrouvey et al. which stated that even in cases of successful recovery of tibial nerve, most patients were unable to perform strenuous activities [25]. At this stage, the NCV also showed chronic tibial nerve injury which corroborates the residual paresthesia and discomfort. The author recommends a few awareness points during MOW-HTO. One of the most important and missed out factors is the length of the incision. In the race to keep the surgery minimally invasive, surgeons try to use smallest possible incisions. This creates the need for excessive retraction. As a result, there is an inadvertent pressure and stretch on the surrounding soft tissue which might be one of the major reasons of iatrogenic stretch injuries to peripheral nerves. In addition, a radiolucent Hohmann retractor should be placed vigilantly abutting the bone to avoid injury to the posterior neurovascular bundle. It is important that the plate is placed well posteriorly which not only maintains the posterior tibial slope but also avoids screw trajectory being too close to the important structures posteriorly. Knee should be flexed while performing the procedure pushing the vital structures more posteriorly. Thus, although MOW is the most reproducible type of HTO with least complications, a thorough knowledge about the surrounding soft tissue and related complications is paramount.
The main aim of this case report is to create awareness about this rare but possible complication during MOW-HTO. Sufficient length of incision, strategic soft-tissue retraction, posterior plate positioning, flexion of knee, and watchful use of saw and drill are some points to keep in mind. It is also very important to be diligent about the minute post-operative clinical findings for early diagnose and treatment such injuries. To the authors’ knowledge, this is the first study reporting tibial nerve damage due to stretch injury during MOW-HTO.
- Awareness about stretch injuries to soft tissues and neurovascular structures during HTO is essential.
- Surgeons should not compromise soft-tissue protection for smaller incisions.
- It is very important to be diligent about minute post-operative signs of nerve injuries as in this case, for early diagnosis and prompt treatment of such complications.
References
- 1.Yasuda K, Majima T, Tsuchida T, Kaneda K. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res 1992;282:186-95. [Google Scholar | PubMed]
- 2.Amendola A. Unicompartmental osteoarthritis in the active patient: The role of high tibial osteotomy. Arthroscopy 2003;19:109-16. [Google Scholar | PubMed]
- 3.Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br 1961;43-B:746-51. [Google Scholar | PubMed]
- 4.Poignard A, Flouzat Lachaniette CH, Amzallag J, Hernigou P. Revisiting high tibial osteotomy: Fifty years of experience with the opening-wedge technique. J Bone Joint Surg Am 2010;92:187-95. [Google Scholar | PubMed]
- 5.Lee OS, Ahn S, Lee YS. Effect and safety of early weight-bearing on the outcome after open-wedge high tibial osteotomy: A systematic review and meta-analysis. Arch Orthop Trauma Surg 2017;137:903-11. [Google Scholar | PubMed]
- 6.Raja Izaham RM, Abdul Kadir MR, Abdul Rashid AH, Hossain MG, Kamarul T. Finite element analysis of Puddu and Tomofix plate fixation for open wedge high tibial osteotomy. Injury 2012;43:898-902. [Google Scholar | PubMed]
- 7.Shenoy PM, Oh HK, Choi JY, Yoo SH, Han SB, Yoon JR, et al. Pseudoaneurysm of the popliteal artery complicating medial opening wedge high tibial osteotomy. Orthopedics 2009;32:442. [Google Scholar | PubMed]
- 8.Attinger MC, Behrend H, Jost B. Complete rupture of the popliteal artery complicating high tibial osteotomy. J Orthop 2014;11:192-6. [Google Scholar | PubMed]
- 9.Jeong JH, Chang MC, Lee SA. Deep peroneal nerve palsy after opening wedge high tibial osteotomy: A case report. Medicine (Baltimore) 2019;98:e16253. [Google Scholar | PubMed]
- 10.Shin YS, Sim HB, Yoon JR. Tibial nerve neuropathy following medial opening-wedge high tibial osteotomy-case report of a rare technical complication. Eur J Orthop Surg Traumatol 2017;27:563-7. [Google Scholar | PubMed]
- 11.Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg 2004;124:649-53. [Google Scholar | PubMed]
- 12.De Mello Junior WA, Arruda LR, Coluccini AM, da Silva Nunes RP, Pedro MA, de Souza MR, et al. Complications following medial opening wedge osteotomy of the knee: Retrospective study. Rev Bras Ortop 2015;46:64-8. [Google Scholar | PubMed]
- 13.Yazdi HR, Torkaman A, Ebrahimzadeh Babaki A, Soleimani M, Eslami A. Fixation method can affect posterior tibial slope in opening-wedge high tibial osteotomy: A retrospective study. J Orthop Surg Res 2023;18:780. [Google Scholar | PubMed]
- 14.Bianchi S, Martinoli C, Demondion X. Ultrasound of the nerves of the knee region: Technique of examination and normal US appearance. J Ultrasound 2007;10:68-75. [Google Scholar | PubMed]
- 15.Itoh M, Itou J, Kuwashima U, Fujieda H, Okazaki K. Deep peroneal nerve injury during plate fixation for medial open-wedge high tibial osteotomy: A case report and cadaveric study. Clin Case Rep 2019;7:2225-30. [Google Scholar | PubMed]
- 16.Lowe JA, Rister J, Eastman J, Freind J. Injury to neurovascular structures with insertion of traction pins around the knee. J Orthop 2015;12:S79-82. [Google Scholar | PubMed]
- 17.Beelmann K, Vogel H, Nahrstedt U. A pseudoaneurysm of the popliteal artery following a valgus osteotomy of the tibial head. Rofo 1994;161:468-70. [Google Scholar | PubMed]
- 18.Pape D, Dueck K, Haag M, Lorbach O, Seil R, Madry H. Wedge volume and osteotomy surface depend on surgical technique for high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:127-33. [Google Scholar | PubMed]
- 19.Kim K, Isu T, Morimoto D, Iwamoto N, Kokubo R, Matsumoto J, et al. Common diseases mimicking lumbar disc herniation and their treatment. Mini Invasive Surg 2017;1:43-51. [Google Scholar | PubMed]
- 20.Alvites R, Rita Caseiro A, Santos Pedrosa S, Vieira Branquinho M, Ronchi G, Geuna S, et al. Peripheral nerve injury and axonotmesis: State of the art and recent advances. Cogent Med 2018;5:1466404. [Google Scholar | PubMed]
- 21.Kowalska J, Grabowski R, Pigonska J, Domzalski M. Management of an iatrogenic injury to the tibial nerve in a 24-year-old hurdle runner. J Int Med Res 2018;46:3394-403. [Google Scholar | PubMed]
- 22.Celik M, Kose A, Kose D, Karakus E, Akpinar E, Calik M, et al. The double-edged sword: Effects of pregabalin on experimentally induced sciatic nerve transection and crush injury in rats. Int J Neurosci 2014;125:845-54. [Google Scholar | PubMed]
- 23.Antoniadis G, Kretschmer T, Pedro MT, König RW, Heinen CP, Richter HP. Iatrogenic nerve injuries: Prevalence, diagnosis and treatment. Dtsch Arztebl Int 2014;111:273-9. [Google Scholar | PubMed]
- 24.Schraut NB, Walton S, Bou Monsef J, Shott S, Serici A, Soulii L, et al. What protects certain nerves from stretch injury? Anat Rec (Hoboken) 2016;299:111-7. [Google Scholar | PubMed]
- 25.Retrouvey H, Silvanathan J, Bleakney RR, Anastakis DJ. A case of posterior tibial nerve injury after arthroscopic calcaneoplasty. J Foot Ankle Surg 2018;57:587-92. [Google Scholar | PubMed]