Post-genicular artery embolization, total knee arthroplasty can be effectively performed with careful vascular evaluation and thorough patient counseling on risks related to wound healing and bone health.
Jai Thilak, Department of Orthopaedics, Amrita Institute of Medical Sciences and Research Centre, Kochi, Kerala, India. E-mail: jaithilak@aims.amrita.edu
Introduction: The literature on total knee arthroplasty following genicular artery embolization (GAE) is still in its early stages. This case highlights the challenges and essential considerations in performing total knee arthroplasty for advanced osteoarthritis (OA) in patients who experience inadequate pain relief following GAE.
Case Report: A patient with advanced OA underwent GAE for knee pain. He had swelling and skin discoloration around the knee, which required readmission. The patient sought further treatment options due to persistent knee pain. After a thorough pre-operative vascular assessment, he underwent total knee arthroplasty. At 1-year follow-up, he reported significant pain relief, improved knee range of motion, and returned back to daily routine activities.
Conclusion: This case illustrates that after GAE for OA, with no pain relief, a successful total knee arthroplasty can be performed after comprehensive pre-operative workup with counselling on GAE issues.
Keywords: Genicular artery embolization, total knee arthroplasty, osteoarthritis.
Osteoarthritis (OA), particularly of the knee, is a major cause of disability in the elderly. This condition is characterized by progressive degeneration of articular cartilage, which leads to increased joint pain and functional limitations [1,2]. Recently, minimally invasive techniques have emerged as alternatives to traditional non-surgical treatments for knee OA. Among these image-guided interventions, genicular artery embolization (GAE) has shown considerable promise for mitigating arthritic pain and functional impairments associated with knee OA [3,4]. GAE is an emerging treatment option for knee OA. GAE targets abnormal neovasculature arising from the genicular arteries that supply the inflamed synovium within the knee joint, aiming to reduce pain and inflammation by selectively blocking these vessels [5]. The GAE technique is based on the idea that neo-angiogenesis and low-grade inflammation are key factors in the pain associated with knee OA [6]. The procedure will be performed under moderate sedation in an interventional radiology suite, with focal pain areas marked. Arterial access will be obtained through the femoral artery, and using a microcatheter, the specific genicular arteries will be catheterized and embolized with Embozene particles until hypervascularity resolves, while preserving normal arterial flow [7]. As with any emerging procedure, ensuring patient safety in GAE trials is crucial, necessitating the careful monitoring of potential adverse effects [8]. These effects can be categorized into two groups: general complications of arterial embolization, such as puncture site hematoma and post-embolization syndrome, and those specific to GAE, including skin discoloration and ulceration, plantar paresthesia, and asymptomatic bone infarction [8,9].
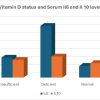
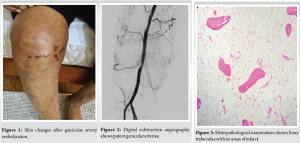
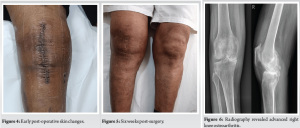
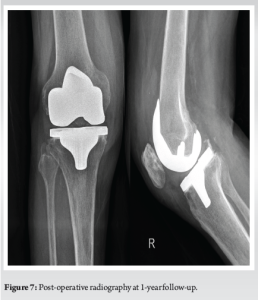
A 77-year-old male with right knee pain was diagnosed with advanced OA. In pursuit of relief, the patient underwent GAE at another hospital. Following the procedure, the patient developed swelling, increased pain, and skin discoloration, necessitating readmission to the same hospital for vascular observation and pain control. Redness, swelling, and pain subsided over a period of 7 days, and the patient was discharged from the hospital (Fig. 1). After a 6-month recovery period, owing to persistent osteoarthritic knee pain, the patient sought further treatment options at our hospital. Upon consultation with our radiologists, an arteriogram was performed 1 year after embolization, and it was ascertained that the genicular arteries remained patent (Fig. 2). Consequently, a decision was made to proceed with total knee arthroplasty to manage OA. During arthroplasty, bone samples of bone cuts from the weight-bearing distal femur and proximal tibia were sent for histopathological examination, and the results were negative for osteonecrosis (Fig. 3). The post-operative period involved meticulous monitoring of complications such as wound dehiscence, tissue necrosis, and infection. Fortunately, aside from the mild erythema observed around the knee a week after the procedure, which did not require any treatment, the wound healed well without any complications, with standard rehabilitation of same-day walking, and ROM exercise could be initiated (Fig. 4 and 5). After 1 year of follow-up, the patient experienced relief of knee pain and achieved a knee range of motion of up to 0°–120° and back to his day-to-day activities, indicating a successful outcome following total knee arthroplasty (Fig. 6 and 7).
Informed consent from the patient was obtained for study participation.
GAE is an emerging, minimally invasive treatment for mild-to-moderate OA, with short- to mid-term results [10]. The primary objective of GAE is to reduce hypervascularity while preserving arterial perfusion, a goal that distinctly sets it apart from many other embolization techniques that aim to achieve complete stasis. It is important to recognize the potential risk of non-target embolization and its associated complications. Follow-up care is essential to evaluate the patient’s response to treatment and monitor the recovery of the femoral artery puncture site. The initial follow-up is usually scheduled one week after the procedure, with additional evaluations potentially occurring at 1, 3, 6, and 12 months to track patient progress and assess the long-term efficacy and safety of GAE. If symptoms do not improve at the 3-month follow-up, alternative treatment strategies may need to be explored [6,11]. The adverse events observed in the GAE trials can be classified into two categories [8]. The first category includes complications common to all arterial embolization procedures, such as hematoma at the puncture site and post-embolization syndrome [9]. Among the adverse effects unique to GAE, transient skin changes are most frequently observed following the procedure. These alterations arise from embolization of minor cutaneous branches originating from the genicular arteries [8]. However, a recent study [7] identified seven cases of self-limiting ulceration associated with the use of 100-micron permanent particles during GAE. Current literature shows that skin changes are generally self-limiting, affecting 10–65% and typically resolving within 3–12 weeks [12,13]. A less frequent side effect of GAE is post-procedural plantar paresthesia. A study by Bagla et al. [13], using 75-micron permanent particles, this effect was observed in 10% of the patients (two out of 20). Thus far, all cases of plantar paresthesia have been self-limiting and resolved within 2 weeks of treatment with gabapentin. The final adverse effect to consider is non-target embolization (NTE), which leads to bone infarction. At present, bone infarcts are infrequent, asymptomatic, and relatively rare. Padia et al. identified these infarcts in two of 40 patients who underwent MRI surveillance 3 months after GAE [7]. The infarcts were located in non-weight-bearing regions of the joint and measured < 2 cm. At 1-year follow-up, no adverse events related to these infarcts were observed. The clinical significance of these findings and their long-term repercussions are unclear because of the limited number of cases studied and the absence of weight-bearing bone infarcts. Consequently, surveillance MRIs at 1-year and subsequent intervals in a larger cohort are essential to determine the relevance of these infarcts and assess the impact of embolization on the knee joint [8]. The potential compromise of osseous blood flow due to particle embolization may lead to osteonecrosis, which could not only diminish the efficacy of GAE but also impact subsequent interventions, such as joint replacement surgery. GAE does not address the wear and degradation of the joint cartilage; therefore, there is an increased risk of joint dysfunction in the long term. Consequently, a significant proportion of patients who undergo GAE may eventually require joint replacement surgery. However, existing literature on complications associated with TKA after GAE is limited. Reportedly, 10 cases of GAE have been documented in which patients later underwent TKA, and follow-up data on these cases are lacking [9]. In a study by Cusumano et al. [14]. on patients undergoing total knee arthroplasty after GAE, 4 complications (8%) were observed, including 2 (4%) related to wound healing, such as wound dehiscence requiring drainage, a small eschar treated with a staple, a stitch abscess, and fluid discharge at the surgical site in two other patients. In a study by Padia et al. [7], two successful TKAs were performed in patients who had previously undergone GAE. Our case adds to the growing body of literature on TKA after GAE. This report describes a 77-year-old patient with end-stage OA who underwent GAE at another institution, experiencing initial issues of GAE, such as skin discoloration, pain, and swelling. Despite these initial symptoms of GAE subsiding, the patient continued to experience osteoarthritic knee pain, ultimately requiring TKA after a thorough pre-operative evaluation, such as vascular assessment. No obvious bone necrosis was noted in the weight-bearing areas of the knee upon histopathological examination. The patient experienced significant pain relief and improved knee range of motion at the 1-year follow-up. Although the case outcome was favorable, this underscores the need for more extensive studies and follow-up data on TKA after GAE. The literature on this specific sequence of interventions is sparse, with only a few documented cases of patients who underwent TKA after GAE. Therefore, the findings of our case report support the need for larger cohort studies to determine the safety, efficacy, and optimal timing of TKA after GAE.
GAE in advanced OA may not be beneficial for patients with additional complications of local tissue reactions. Total knee arthroplasty after GAE can be successfully performed after proper evaluation of the vascular status with digital subtraction angiography around the knee and counseling of the patient in detail about the issues of wound healing and bone necrosis, which were not present in the weight-bearing bone of the knee in our case, following GAE.
Undergoing GAE before total knee replacement may lead to post-operative complications. However, with appropriate clinical evaluation, investigation, and counselling to the patient, TKR can be performed safely after GAE.
References
- 1.Murphy L, Helmick CG. The impact of osteoarthritis in the United States: A population-health perspective: A population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs 2012;31:85-91. [Google Scholar]
- 2.Martel-Pelletier J, Boileau C, Pelletier JP, Roughley PJ. Cartilage in normal and osteoarthritis conditions. Best Pract Res Clin Rheumatol 2008;22:351-84. [Google Scholar]
- 3.Okuno Y, Korchi AM, Shinjo T, Kato S. Transcatheter arterial embolization as a treatment for medial knee pain in patients with mild to moderate osteoarthritis. Cardiovasc Intervent Radiol 2015;38:336-43. [Google Scholar]
- 4.Epelboym Y, Mandell JC, Collins JE, Burch E, Shiang T, Killoran T, et al. Genicular artery embolization as a treatment for osteoarthritis related knee pain: A systematic review and meta-analysis. Cardiovasc Intervent Radiol 2023;46:760-9. [Google Scholar]
- 5.Liu S, Swilling D, Morris EM, Macaulay W, Golzarian J, Hickey R, et al. Genicular artery embolization: A review of essential anatomic considerations. J Vasc Interv Radiol 2024;35:487-96.e6. [Google Scholar]
- 6.Sterbis E, Casadaban L. Genicular artery embolization technique. Tech Vasc Interv Radiol 2023;26:100878. [Google Scholar]
- 7.Padia SA, Genshaft S, Blumstein G, Plotnik A, Kim GH, Gilbert SJ, et al. Genicular artery embolization for the treatment of symptomatic knee osteoarthritis. JB JS Open Access 2021;6:e21.00085. [Google Scholar]
- 8.O’Grady AM, Little MW. Genicular artery embolization data review. Tech Vasc Interv Radiol 2023;26:100880. [Google Scholar]
- 9.Casadaban LC, Mandell JC, Epelboym Y. Genicular artery embolization for osteoarthritis related knee pain: A systematic review and qualitative analysis of clinical outcomes. Cardiovasc Intervent Radiol 2021;44:1-9. [Google Scholar]
- 10.Okuno Y, Korchi AM, Shinjo T, Kato S, Kaneko T. Midterm clinical outcomes and MR imaging changes after transcatheter arterial embolization as a treatment for mild to moderate radiographic knee osteoarthritis resistant to conservative treatment. J Vasc Interv Radiol 2017;28:995-1002. [Google Scholar]
- 11.Poursalehian M, Bhia I, Ayati Firoozabadi M, Mortazavi SM. Genicular artery embolization for knee osteoarthritis: A comprehensive review. JBJS Rev 2023 Sep 8;11(9). doi: 10.2106/JBJS.RVW.23.00082. [Google Scholar]
- 12.Lee SH, Hwang JH, Kim DH, So YH, Park J, Cho SB, et al. Clinical outcomes of transcatheter arterial embolisation for chronic knee pain: Mild-to-moderate versus severe knee osteoarthritis. Cardiovasc Intervent Radiol 2019;42:1530-6. [Google Scholar]
- 13.Bagla S, Piechowiak R, Hartman T, Orlando J, Del Gaizo D, Isaacson A. Genicular artery embolization for the treatment of knee pain secondary to osteoarthritis. J Vasc Interv Radiol 2020;31:1096-102. [Google Scholar]
- 14.Cusumano L, Albrecht H, Masterson K, Genshaft S, Stewart J, Callese T, et al. Abstract No. 366 safety of total knee arthroplasty following genicular artery embolization for knee osteoarthritis. J Vasc Interv Radiol 2024;35:S163. [Google Scholar]