The intra-articular antibiotic (IAA) irrigation system represents a novel approach to chronic PJI management by enabling high local antibiotic delivery and a shortened interstage interval, with potential benefits in infection clearance, functional recovery, and reduced systemic exposure, while underscoring the importance of patient selection, provider expertise, and ongoing research.
Dr. Nicolas Piuzzi, Cleveland Clinic, Orthopedic and Rheumatology Institute, 9500 Euclid Ave, A41, Cleveland, OH 44195. E-mail: piuzzin@ccf.org
Introduction: The current standard for treating chronic periprosthetic joint infection (PJI) in North America, a two-stage exchange arthroplasty, has success rates of 65–90% but involves prolonged interstage periods, increased morbidity, and a high 5-years mortality rate of up to 25%. These limitations have driven research into alternative approaches, such as intra-articular antibiotic (IAA) irrigation, which uses a specialized titanium spacer for localized antibiotic delivery over a 7-day period.
Case Report: A 53-year-old male with chronic PJI of the left knee underwent a novel rapid two-stage exchange arthroplasty using an IAA irrigation system. The first stage involved implant removal and placement of a specialized antibiotic delivery IAA device. During the 7-day interstage period, high-concentration local antibiotics (tobramycin and vancomycin) were administered. The second stage, performed 1 week later, included reimplantation with a total stabilized revision knee system. At 1-year post-surgery, the patient demonstrated excellent functional recovery, pain-free mobility, and no signs of recurrent infection.
Conclusion: This case illustrates the potential of IAA in managing chronic PJI, offering rapid reimplantation and effective infection control. While promising, larger studies are needed to establish long-term efficacy and cost-effectiveness of this innovative approach.
Keywords: Chronic, periprosthetic joint infection, intra-articular antibiotic, two stage, revision, knee.
Periprosthetic joint infection (PJI) remains one of the most challenging and devastating complications following total knee arthroplasty (TKA) [1]. Despite advances in preoperative optimization, surgical techniques and antimicrobial therapies, PJI continues to be a leading cause of failure and revision in TKA, with an incidence of 0.5–1% following primary procedures [2-9]. The current gold standard for treating chronic PJI in North America is a two-stage exchange arthroplasty [10,11]. While this method has demonstrated success rates of 65–90% in eradicating infection, it is associated with substantial drawbacks [12,13]. Patients often endure a prolonged period between stages with limited mobility and function. The interstage interval, which typically lasts 6–12 weeks or longer, places patients at risk for spacer-related complications and general deconditioning [14]. Furthermore, recent studies have highlighted concerning mortality rates associated with two-stage exchange, with reports of up to 25% mortality at 5 years – a rate 4 times higher than matched patients undergoing aseptic revision arthroplasty [15]. The limitations of current treatment strategies have spurred research and development into novel approaches for managing PJI [16]. One such innovative technique is the use of intra-articular antibiotic (IAA) irrigation as part of a modified abbreviated two-stage exchange protocol. This method aims to deliver high local concentrations of antibiotics directly to the infected joint space and surrounding tissues while minimizing systemic exposure and toxicity [17]. The IAA system consists of a specially designed titanium spacer with internal channels and surface pores that allow for controlled antibiotic delivery and evacuation. Daily cycles of vancomycin and tobramycin irrigation are administered through the spacer device over a 7-day period, theoretically achieving local antibiotic concentrations well above the minimum biofilm eradication concentration required to effectively treat established bacterial biofilms [18-20]. Preliminary results using this IAA device and protocol have been published, demonstrating promising outcomes in terms of infection eradication and patient safety. A recent prospective, randomized Phase II study comparing IAA to standard two-stage exchange showed no significant difference in adverse events between groups, with minimal systemic antibiotic exposure in the IAA cohort [17]. However, detailed accounts of the surgical technique, perioperative management, and patient-specific outcomes using this novel approach are limited in the literature. This case report aims to provide an in-depth description of a patient with chronic knee PJI treated using this novel IAA system, focusing on the nuances of the surgical procedure, postoperative care, and clinical course.
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
Patient information
A 53-year-old male, presented with a 1-year history of mild left knee pain. He had undergone bilateral TKAs in June and July 2020, with the left TKA complicated by persistent drainage after surgery. In July 2021, he developed increased pain and swelling in the left knee. On examination, the patient had a body mass index of 28.37 kg/m². His left knee showed an effusion with range of motion from 0° to 120°. Radiographs demonstrated well-aligned and fixed implants without evidence of loosening or osteolysis. Laboratory tests revealed elevated inflammatory markers (C-reactive protein 1.1 mg/dL and erythrocyte sedimentation rate 24 mm/h) and synovial fluid analysis showed a total nucleated cell count of 53,052 with 94% polymorphonuclear cells, meeting the musculoskeletal infection society criteria for PJI [21]. All cultures were negative. At this point, surgical treatment was advised.
Surgical technique
Stage 1: Implant removal and antibiotic spacer placement
The procedure began with the patient in a supine position under general anesthesia. A tourniquet was applied to the left upper thigh. The surgical site was prepped and draped in the usual sterile fashion. The knee was approached through the previous midline incision, which was extended proximally and distally for better exposure. Upon entering the joint through a median parapatellar arthrotomy, purulent fluid was immediately encountered, confirming the clinical suspicion of infection. Samples of this fluid were sent for culture and cell count analysis. Multiple tissue samples were taken from areas adjacent to all implants and sent for frozen section analysis and culture, which subsequently were all negative. Attention was then turned to the femoral component. Despite being well-fixed, it was carefully removed using a combination of flexible osteotomes and oscillating saw to loosen interphase between the implant and the femur. After removal, areas of abscess erosion were discovered behind the anterior flange and between the condyles. These areas were radically debrided down to healthy-appearing bone. The tibial component was also well-fixed, requiring high-speed burs, a sagittal saw, and multiple osteotomes to break up the cement-implant interfaces. After implant removal, central metaphyseal bone deficiency was noted in the proximal tibia. Following implant removal, the intramedullary canals of both the femur and tibia were debrided and reamed with flexible reamers and irrigated with 5 liters of pulsatile sterile saline each (Fig. 1). The entire knee space was then soaked with.

antimicrobial solution (combining 250 mL of 3% hydrogen peroxide, 15 mL of 10% povidone-iodine, and 235 mL of normal saline [NS], totaling 500 mL) after component removal, half of this solution (250 mL) was used to soak the wound for 3 min, followed by irrigation with 3.0 L of NS using pulsatile lavage. For reconstruction, a VT-X7 antibiotic delivery device (Osteal Therapeutics Inc., Dallas, Texas) was chosen (Fig. 2). Conical hand reamming was done in both the femur and the tibia, with a size 7 stem was placed in the tibia, and a size 12 stem was used in the femur (Figs. 3 and 4). These were connected with a 25 mm connector to achieve appropriate leg length and stability, effectively creating a temporary fusion construct to span the joint and maintain limb length (Fig. 5). Once the antibiotic delivery spacer was inserted, the joint was irrigated again with antimicrobial solutions with the remaining 250 mL soaking the wound for 3 min, concluded by another 3.0 L NS pulsatile lavage.



Then the site was prepared for the IAA irrigation system. Black sponges were placed in the medial and lateral gutters, with another placed in a 5 cm gap left proximally. The capsule was partially closed using #1 PDS running suture. An integrated wound management system (3M™ V.A.C.® Ulta Therapy System, Saint Paul, MN) was applied to facilitate the postoperative antibiotic delivery.
The procedure concluded with the application of a sterile compression dressing, stocking, and knee immobilizer. The total operative time was 2 h and 56 min, with a tourniquet time of 90 min, and an estimated blood loss of 400 cc.
Interstage period
Following Stage 1 surgery, the patient began the IAA irrigation protocol. This consisted of daily cycles of tobramycin (80 mg in 50 mL NS) with a 2-h soak time, followed by hourly cycles of vancomycin (125 mg in 50 mL NS) with 30-min soak times. The V.A.C. Ulta™ system was programmed to deliver the antibiotics and provide intermittent negative pressure. Serum antibiotic levels were monitored daily after local irrigation with all values recorded being Vancomycin <4 ug/mL and Tobramycin <0.4 ug/mL. The patient remained hospitalized during this 7-day period, maintaining strict non-weight bearing status and keeping the extremity elevated when in bed (Fig. 6). Systemic IV antibiotics (daptomycin 700 mg/24 h and piperacillin/tazobactam 3.375 g/6 h) were administered as directed by the infectious disease service.

Stage 2: Reimplantation
One week after stage 1 surgery, the patient returned to the operating room for the second stage of his exchange arthroplasty. The procedure began similarly to the first stage, with the patient positioned supine and the left lower extremity prepped and draped in the usual sterile fashion (Fig. 7).

The temporary antibiotic delivery device was carefully removed. The surgeon then performed a thorough assessment of the remaining bone stock and soft tissue quality. Recontruction was performed with short stemmed Triathlon Total Stabilized Revision Knee System (Stryker, Mahwah, NJ) with varus valgus contrained. All components were cemented into place using four doses of antibiotic-loaded (tobramycin) cement (Simplex™ P with Tobramycin, Stryker, Mahwah, NJ). Stability was excellent throughout the arc of motion, with the total stabilized insert providing additional constraint. The patella tracked well centrally without the need for a lateral release. The wound was copiously irrigated, and meticulous hemostasis was achieved. The arthrotomy and subcutaneous tissues were closed in layers using absorbable sutures. The skin was closed with nylon sutures, and an incisional VAC dressing was applied.
Postoperative course
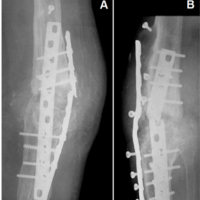
Immediately following the Stage 2 procedure, the patient was started on intravenous (IV) antibiotics. He received IV daptomycin 700 mg/24 h and piperacillin/tazobactam 3.375 g/6 h for a total duration of 5 weeks post-reimplantation. Following the completion of the IV antibiotic course, the patient was transitioned to oral doxycycline 100 mg twice daily. This oral antibiotic regimen was planned to continue for 3 months, extending the total duration of antibiotic treatment to approximately 4.5 months post-reimplantation. 1 month after the stage 2 procedure, the surgical incision was noted to be dry and well-healed. X-rays taken at this time showed that the implants were well-aligned and well-fixed, with no evidence of loosening or osteolysis. The patella was also well-positioned. The range of motion was noted to be from 0° of extension to 110° of flexion. He reported no pain at this visit. 1 year after the stage 2 procedure, repeat X-rays were obtained. These images again demonstrated that the implants remained well-aligned and well-fixed. There was no evidence of loosening, osteolysis, or any other signs of failure or recurrent infection (Fig. 8).

The inflammatory markers normalized, and he demonstrated excellent functional recovery. He reported no pain in the left knee and denied any limitations in his daily activities. He had returned to activities such as skiing and cycling without complications, indicating successful eradication of the infection and a well-functioning knee replacement.
The management of chronic PJI remains a major challenge in orthopedic surgery. While two-stage exchange arthroplasty is considered the gold standard treatment in North America, it is associated with substantial patient morbidity and mortality [2-9]. Alternative treatments have been explored, including one-stage exchange, debridement with implant retention, and long-term suppressive antibiotic therapy in certain cases [10,11]. However, each of these approaches has limitations, particularly in the context of chronic infections with resistant organisms or significant bone loss. The case presented here demonstrates the potential of a novel approach using IAA as part of a modified two-stage exchange protocol. The IAA technique, as illustrated in this case, offers several potential advantages over traditional two-stage exchange. Perhaps the most noteworthy benefit is the shortened interval between stages, which in this case was reduced to just 1 week. This rapid reimplantation minimizes the period of functional limitation for the patient and may reduce the risk of interim complications such as muscle atrophy, joint stiffness, and spacer-related issues. In addition, the high local concentrations of antibiotics achieved through the IAA system may be more effective in eradicating biofilm-associated bacteria than systemic therapy alone or cement eluting antibiotics potentially improving infection clearance rates. The use of a specialized titanium spacer with internal channels also allows for more controlled and consistent antibiotic delivery compared to traditional antibiotic-loaded cement spacers, which typically have inconsistent and short lasting elution characteristics. Despite these advantages, the IAA technique is not without potential drawbacks. The system requires specialized equipment and training, especially in the interim which may limit its widespread adoption and may require attention to the surgical technique and postoperative management. Furthermore, the implementation of this technique involves logistical considerations. It requires personnel training for the interstage phase, including nursing staff to manage the antibiotic delivery system and patient monitoring. The pharmacy department must be equipped to prepare and manage the specific antibiotic formulations required for the irrigation protocol. Additionally as with any new technology long-term cost-effectiveness remains to be determined. The safety and successful outcome in this case aligns with the promising results reported in the recent prospective, randomized Phase II study by Springer et al. [17]. Their study demonstrated that the IAA technique had a safety profile comparable to standard two-stage exchange, with no significant difference in adverse events between groups. Importantly, they found that the IAA group had minimal systemic antibiotic exposure, with serum antibiotic levels well below toxicity thresholds. However, as with our case report, longer-term follow-up and larger patient cohorts will be necessary to fully establish the efficacy and durability of this technique. Future research should focus on optimizing patient selection criteria, refining the antibiotic delivery protocol, and evaluating long-term outcomes. In addition, comprehensive cost-effectiveness analyses will be crucial in determining the role of IAA in the broader context of PJI management, given the major economic burden associated with PJI.
This case report demonstrates the successful application of a novel IAA system in the treatment of chronic PJI of the knee. The technique, which combines a specialized antibiotic delivery device with a shortened interstage interval, resulted in successful eradication of infection and excellent functional outcomes at 1-year post-reimplantation.
This case highlights the potential of a novel IAA irrigation system as part of a modified two-stage exchange protocol for managing chronic PJI of the knee. By delivering high local antibiotic concentrations and enabling a shortened interstage interval, this approach offers promising outcomes in infection eradication and functional recovery while minimizing systemic antibiotic exposure.
References
- 1.Siddiqi A, Warren JA, Manrique-Succar J, Molloy RM, Barsoum WK, Piuzzi NS. Temporal trends in revision total hip and knee arthroplasty from 2008 to 2018: Gaps and opportunities. J Bone Joint Surg Am 2021;103:1335-54. [Google Scholar | PubMed]
- 2.Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev 2014;27:302-45. [Google Scholar | PubMed]
- 3.Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 2017;32:2663-8. [Google Scholar | PubMed]
- 4.Piuzzi NS, Klika AK, Lu Q, Higuera-Rueda CA, Stappenbeck T, Visperas A. Periprosthetic joint infection and immunity: Current understanding of host-microbe interplay. J Orthop Res 2024;42:7-20. [Google Scholar | PubMed]
- 5.Ng MK, Kobryn A, Emara AK, Krebs VE, Mont MA, Piuzzi NS. Decreasing trend of inpatient mortality rates of aseptic versus septic revision total hip arthroplasty: An analysis of 681,034 cases. Hip Int 2023;33:1063-71. [Google Scholar | PubMed]
- 6.Rullán PJ, Orr MN, Emara AK, Klika AK, Molloy RM, Piuzzi NS. Understanding the 30-day mortality burden after revision total hip arthroplasty. Hip Int 2023;33:727-35. [Google Scholar | PubMed]
- 7.Sinclair ST, Orr MN, Rothfusz CA, Klika AK, McLaughlin JP, Piuzzi NS. Understanding the 30-day mortality burden after revision total knee arthroplasty. Arthroplast Today 2021;11:205-11. [Google Scholar | PubMed]
- 8.Puhto T, Puhto AP, Vielma M, Syrjälä H. Infection triples the cost of a primary joint arthroplasty. Infect Dis (Lond) 2019;51:348-55. [Google Scholar | PubMed]
- 9.Davidson DJ, Spratt D, Liddle AD. Implant materials and prosthetic joint infection: The battle with the biofilm. EFORT Open Rev 2019;4:633-9. [Google Scholar | PubMed]
- 10.Shichman I, Ward SA, Lu L, Garceau S, Piuzzi NS, Seyler TM, et al. Failed 2-stage revision knee arthroplasty for periprosthetic joint infection-patient characteristics and outcomes. J Arthroplasty 2023;38:2177-82. [Google Scholar | PubMed]
- 11.Miller R, Higuera CA, Wu J, Klika A, Babic M, Piuzzi NS. Periprosthetic joint infection: A review of antibiotic treatment. JBJS Rev 2020;8:e1900224. [Google Scholar | PubMed]
- 12.Gomez MM, Tan TL, Manrique J, Deirmengian GK, Parvizi J. The fate of spacers in the treatment of periprosthetic joint infection. J Bone Joint Surg Am 2015;97:1495-502. [Google Scholar | PubMed]
- 13.Kozaily E, Tan TL, Yacovelli S, Anis H, Higuera C, Piuzzi NS, et al. Interim spacer exchange for treatment of periprosthetic joint infection: Almost half the patients subsequently fail. J Arthroplasty 2022;37:150-5. [Google Scholar | PubMed]
- 14.Cancienne JM, Werner BC, Bolarinwa SA, Browne JA. Removal of an infected total hip arthroplasty: Risk factors for repeat debridement, long-term spacer retention, and mortality. J Arthroplasty 2017;32:2519-22. [Google Scholar | PubMed]
- 15.Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am 2013;95:2177-84. [Google Scholar | PubMed]
- 16.Tidd JL, Pasqualini I, McConaghy K, Higuera CA, Deren ME, Visperas A, et al. The use of oral antibiotics after total joint arthroplasty: A critical analysis review. JBJS Rev 2023;9;11(10). doi: 10.2106/JBJS.RVW.23.00083 [Google Scholar | PubMed | CrossRef]
- 17.Springer BD, Higuera-Rueda CA, De Beaubien BC, Warner KD, Glassman AH, Parvataneni HK, et al. Safety profile of seven-day intra-articular antibiotic irrigation for the treatment of chronic periprosthetic joint infection: A prospective randomized phase II comparative study. J Arthroplasty 2024;39:S229-35.e1. [Google Scholar | PubMed]
- 18.Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A. The Calgary biofilm device: New technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol 1999;37:1771-6. [Google Scholar | PubMed]
- 19.Visperas A, Santana D, Klika AK, Higuera-Rueda CA, Piuzzi NS. Current treatments for biofilm-associated periprosthetic joint infection and new potential strategies. J Orthop Res 2022;40:1477-91. [Google Scholar | PubMed]
- 20.Higuera-Rueda CA, Piuzzi NS, Milbrandt NB, Tsai YH, Klika AK, Samia AC, et al. The mark Coventry award: PhotothermAA gel combined with debridement, antibiotics, and implant retention significantly decreases implant biofilm burden and soft-tissue infection in a rabbit model of knee periprosthetic joint infection. J Arthroplasty 2024;39:S2-8. [Google Scholar | PubMed]
- 21.Warren J, Anis HK, Bowers K, Pannu T, Villa J, Klika AK, et al. Diagnostic utility of a novel point-of-care test of calprotectin for periprosthetic joint infection after total knee arthroplasty: A prospective cohort study. J Bone Joint Surg Am 2021;103:1009-15. [Google Scholar | PubMed]