To assess the effectiveness of closed reduction and percutaneous K-wire fixation in managing displaced supracondylar humeral fracture in children.
Dr. Sheik Mohideen, Department of Orthopaedics and Traumatology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India. E-mail: sheik.145@gmail.com
Introduction: Supracondylar humerus fractures are the most common elbow injuries in children, accounting for approximately 60% of all pediatric elbow fractures, primarily occurring in the first decade of life. These fractures are often associated with complications such as compartment syndrome, neurovascular injury, Volkmanns ischemic contracture, and malunion. The most common complication is cubitus varus deformity. The preferred pinning techniques include either a crossed pin construct or two lateral pins. Among various treatment approaches, closed reduction with percutaneous K-wire fixation has been found to be the most effective, with minimal complications. This study aims to assess the functional and radiological outcomes of pediatric displaced supracondylar humerus fractures managed with closed reduction and percutaneous K-wire fixation.
Materials and Methods: 35 consecutive patients meeting the studys inclusion and exclusion criteria were enrolled. Data are collected and analyzed using Microsoft Excel for statistical calculations.
Results: In this study, 25 children (62%) sustained the fracture within the first decade of life. Males showed a higher incidence than females. The Mayo elbow scores recorded at 6 months was 96.01 ± 2.80. Pin tract infections were observed in 10 patients, while 3 cases presented with cubitus rectus. Clinical outcomes, evaluated using Flynns criteria, showed fair outcome in 1 case, good outcomes in 3 cases, and excellent outcomes in 31 cases.
Conclusion: Percutaneous pinning after closed reduction, whether using a crossed configuration or lateral pinning remains the preferred treatment for supracondylar fracture of the humerus in pediatric patients. When performed with the proper technique, both configurations yield successful outcomes. This approach is a safe, economical, and least invasive option with low morbidity.
Keywords: Supracondylar humerus fracture, pediatric population, Baumanns angle, Mayo elbow score.
Supracondylar humeral fracture accounts for 50–70% of all elbow fractures in children between 1 and 10 [1]. Gartland classification is the most commonly used classification used to guide treatment for fractures. Managing these injuries is difficult due to immediate and long-term complications, such as: (1) compartment syndrome, (2) neurovascular damage, and (3) Volkmanns ischemic contracture and malunion [2,3]. These fractures are either (1) flexion type or (2) extension type (most common) [4]. Extension type is further classified into three types – types – 1 – undisplaced, type – 2 – partially displaced with an intact posterior hinge, and type – 3 – completely displaced. Type 1 and 2 fractures, treatment involves closed reduction followed by cast application, Dunlop traction, or olecranon traction. Type – 2 and 3 generally require closed reduction and pinning. Closed reduction and plaster of Paris (POP) slab or cast application, Dunlop skin traction, and olecranon traction are associated with high complication rates. Conservative treatment can lead to compartment syndrome, malunion, and loss of reduction [5]. Closed reduction with pinning involves either cross-medial and lateral pins or two lateral pins. This method has shown high success rates according to multiple studies. It has the lowest complication rates.
Objectives
This study aims to assess the effectiveness of closed reduction and percutaneous K-wire fixation in managing displaced supracondylar humeral fracture in children.
This prospective observational study was conducted at Chettinad Hospital and Research Institute, Kanchipuram from February 2022 to January 2024. Consecutive patients with displaced supracondylar humerus fractures presenting to the orthopedics outpatient department were included. A detailed history was obtained, followed by a comprehensive general, local, and systemic examination to assess for deformities, neurovascular injuries, and compartment syndrome. The clinical diagnosis was confirmed using a plain X-ray of the elbow joint in anteroposterior and lateral views. The patient would undergo surgical procedures after obtaining informed written consent from the parent or legal guardian.
Surgical procedure
After pre-operative evaluation, all surgeries were performed under general anesthesia. Closed reduction was achieved using traction and counter – traction along the longitudinal axis with the elbow in extension and supination. The reduction was maintained by forearm pronation and confirmed under an image intensifier in two views – anteroposterior (Jones) and lateral. Once proper alignment was ensured, percutaneous K-wire fixation was used to stabilize the reduction. K-wire ranging from 1.2 mm to 2.0 mm in diameter was utilized. The number of K-wires was determined based on intraoperative stability – either two cross K-wide fixations or, in cases of instability, an additional lateral K-wire was placed for enhanced fixation. Reduction and fixation were verified under an image intensifier, and a posterior above elbow POP slab was applied in the forearm in 90° flexion.
Follow-up
Patient who underwent surgery received pin tract dressing weekly or biweekly. K-wires were removed 4–6 weeks after surgery once an X-ray confirmed with adequate callus formation. Simultaneously, the POP splint was removed, and the patients were encouraged for elbow range of movement. Follow-ups were at 6 weeks, 3 months, and 6 months after surgery. The patients were assessed with Mayo elbow score and Baumanns angle (Table 1).
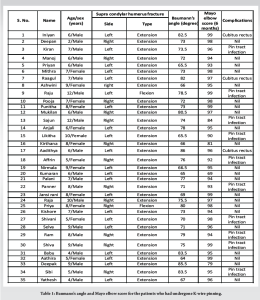
A total of 35 pediatric patients, aged between 2 and 12 years (mean age: 7.15 years), underwent supracondylar pinning for the supracondylar humerus fractures. Of these, 22 were male and 13 were female. In the study, 21 cases involved the left side, while 14 cases affected the right side. Extension-type fractures were observed in 93% of patients, while 7% had flexion-type fractures. All patients were followed up for a minimum of 6 months. Superficial pin tract infections developed in 10 patients, all of whom recovered after pin removal and oral antibiotics treatment. No cases of severe infection or septic arthritis were reported. Cubitus rectus seen in 3 patients (8%) who showed positive functional outcomes during the follow-up. No instances of neurovascular injury, compartment syndrome, and migration of the pin were observed in this study. At the 6-month follow-up, the mean Mayo Elbow score was 96.01 ± 2.80. Based on this assessment, 31 patients achieved excellent outcomes, while 3 had good outcomes and 1 had fair outcome. No poor outcomes were recorded. The mean Baumanns angle was 75.90 ± 10.01 (Fig. 1-4].

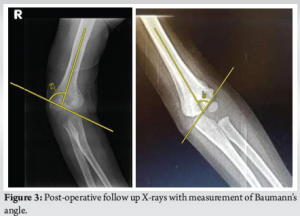

Supracondylar humerus fractures are one of the most common fractures that affect children. It constitutes for more than 50% of elbow fractures. The fractures typically occur within the first 10 years of life and affect the distal humerus, near the metaphysis. It is of two types – flexion and extension type [6]. The standard treatment involves closed reduction followed by percutaneous pin fixation. Several treatment methods have been used in the management of supracondylar humerus fractures. Non-surgical treatment is generally considered only for fractures that are not displaced or displaced minimally. They are managed with reduction and stabilized with a POP cast. However, in cases of displaced or open fractures, surgical intervention is necessary to prevent complications, such as malunion, cubitus varus, restricted elbow movement, and persistent pain. Open reduction with fixation is recommended in specific scenarios, such as open fractures requiring vascular exploration or fractures that cannot be reduced by closed methods. In this study, the average age of the children was 7.15 years, ranging from 2 to 12 years. A study conducted in Saudi Arabia by Khan et al. reported a similar mean age of 8.1 years [7]. The majority of our study population was between 5 and 10 years (62%), which is consistent with the findings by Fowels et al. According to Reising et al., supracondylar humerus fractures were common for the ages above 4 years and below 9 years [8]. This study also found that boys were more frequently affected than girls (62.8% vs. 37.2%), a trend that aligns with findings by Devkota et al., who reported male–to-female ratio of 58:44. This difference is due to boys higher level of sports and physical exertion, making them more susceptible to falls and injuries [9]. Among 35 cases, 21 involved the left arm while 14 affected the right side. These findings correspond with those of Devkota et al., who reported a left-to-right arm ratio of 54:48. This pattern is often attributed to the protective function of the non-dominant limb during falls [9]. The clinical outcomes in this study were assessed using the Mayo Elbow score. At the 6 month follow-up, the mean score was 96.01 ± 2.80, which aligns with findings by Sinikumpu et al., who reported a mean score of 96.4 in patients with modified Gartlands type 3 fractures [10]. Similarly, Ulmar et al. documented excellent outcomes, reinforcing the effectiveness of the treatment approach used in this study [11]. On an anteroposterior radiograph, Baumanns angle is defined as the angle formed between the physeal line of the lateral condyle and the distal humeral metaphysis in relation to the long axis of the humerus. At 6 months, three patients showed cubitus rectus. The standard Baumanns angle ranges from 64° to 81°. In this study, the mean Baumanns angle at 6 months was 75.90 ± 10.01, which is within the acceptable range. Similar results were observed in a study by Lee et al., which found no significant changes [12]. In addition, Kitta et al. had used humeral capitellar angle to assess how the fracture fragments were reduced, and specifying the importance of maintaining the carrying angle. The mean humeral capitellar angle was 72.3 [13]. Basaran et al. conducted a similar study, reporting an insignificant difference between closed reduction with or without a medial incision [14].
Percutaneous pinning after closed reduction, whether using a crossed configuration or lateral pinning remains an effective approach for treating a supracondylar fracture of the humerus in pediatric patients. This technique is an economical and least invasive option with low morbidity.
Closed reduction and percutaneous pinning is an effective treatment for supracondylar humerus fractures in the pediatric population.
References
- 1.MacEwen GD. Tachdjian s Pediatric Orthopaedics. 3rd ed., Vol. 1, 2, 3. Netherlands: Elsevier Health Sciences; 2002. p. 1104. [Google Scholar | PubMed]
- 2.Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Ser A 2007;89:706-12. [Google Scholar | PubMed]
- 3.Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, et al. Delaying treatment of supracondylar fractures in children: Has the pendulum swung too far? J Bone Joint Surg Br 2008;90:1228-33. [Google Scholar | PubMed]
- 4.Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. J Pediatr Orthop Part B 2001;10:63-7. [Google Scholar | PubMed]
- 5.Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop B 2007;27:181-6. [Google Scholar | PubMed]
- 6.Mulhall KJ, Abuzakuk T, Curtin W, OSullivan M. Displaced supracondylar fractures of the humerus in children. Int Orthop 2000;24:221-3. [Google Scholar | PubMed]
- 7.Khan AQ, Goel S, Abbas M, Sherwani MK. Percutaneous K-wiring for Gartland type III supracondylar humerus fractures in children. Saudi Med J 2007;28:603-6. [Google Scholar | PubMed]
- 8.Reising K, Schmal H, Kohr M, Kuminack K, Sudkamp NP, Strohm PC. Surgical treatment of supracondylar humerus fractures in children. Acta Chir Orthop Traumatol Cech 2011;78:519-23. [Google Scholar | PubMed]
- 9.Devkota P, Khan JA, Acharya BM, Pradhan NM, Mainali LP, Singh M, et al. Outcome of supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. J Nepal Med Assoc 2008;47:66-70. [Google Scholar | PubMed]
- 10.Sinikumpu JJ, Victorzon S, Pokka T, Lindholm EL, Peljo T, Serlo W. The long-term outcome of childhood supracondylar humeral fractures. Bone Joint J 2016;98-B:1410-7. [Google Scholar | PubMed]
- 11.Ulmar B, Brunner A, Kocak T, Schwarz J, Stöckle U, Mittlmeier T, et al. Behandlungsergebnisse operativ versorgter kindlicher suprakondylärer Humerusfrakturen. Zeitschrift Orthop Unfallchir 2012;150:488-94. [Google Scholar | PubMed]
- 12.Lee BJ, Lee SR, Kim ST, Park WS, Kim TH, Park KH. Radiographic outcomes after treatment of pediatric supracondylar humerus fractures using a treatment-based classification system. J Orthop Trauma 2011;25:18-25. [Google Scholar | PubMed]
- 13.Kitta MI, Ismiarto YD, Saleh MR, Sakti M, Abidin MA, Putra LT. Analysis of radiological alignment and functional outcomes of pediatric patients after surgery with displaced supracondylar humerus fracture: A cross-sectional study. Int J Surg Open 2020;24:136-42. [Google Scholar | PubMed]
- 14.Basaran SH, Ercin E, Bayrak A, Bilgili MG, Kizilkaya C, Dasar U, et al. The outcome and parents-based cosmetic satisfaction following fixation of paediatric supracondylar humerus fractures treated by closed method with or without small medial incision. SpringerPlus 2016;5:174. [Google Scholar | PubMed]











