By sharing the novel approach of thumb carpometacarpal joint stabilisation with flexor carpi radialis tendon with further suture anchoring and its successful application, this case report aims to enhance clinical practice and improve patient outcomes in the management of thumb CMC joint instability.
Dr. Aditya A Agarwal, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: dradiagr@gmail.com
Introduction: Chronic instability of the carpometacarpal (CMC) joint of the thumb can significantly impair hand function and cause persistent pain. Stabilising this joint is crucial for restoring function and alleviating discomfort. Utilising the flexor carpi radialis (FCR) tendon for stabilisation has shown promise due to its anatomical suitability and biomechanical properties.
Case Report: A 20-year-old female patient presented with a complaint of non-traumatic popping of the metacarpophalangeal joint for the past 3 years. Conservative treatments, including splinting and physical therapy, were unsuccessful. Surgical stabilisation of the CMC joint with the FCR tendon was performed. The surgery was successful without intraoperative complications. Postoperative care involved immobilisation followed by a structured rehabilitation program. At 6 months and 1 year post-surgery, the patient experienced significant pain relief and improved thumb stability, with no recurrence of instability. Functional assessments indicated restored grip and pinch strength, assisting the patient to return to daily activities and work without limitations.
Conclusion: There was improvement in visual analogue scale score, disabilities of the arm, shoulder, and hand, and Kapandji score denoting better functional and pain outcome scores postoperatively. Using the FCR tendon with a suture anchor for CMC joint stabilisation in the thumb is an effective treatment for chronic instability, offering significant pain relief, enhanced stability, and restored hand function. This case supports the potential benefits of this surgical approach, though further research with larger cohorts is necessary to validate these findings.
Keywords: Carpometacarpal joint, chronic instability, stabilization, flexor carpi radialis, suture anchor.
The carpometacarpal (CMC) joint is essential for thumb function, allowing a wide range of motion (ROM) at the cost of stability. It experiences higher forces compared to other finger joints, making it prone to instability from ligament laxity, trauma, overexertion, or conditions like trapezium dysplasia [1]. This instability can lead to pain, functional limitations, subluxation, and strength loss, particularly during pinch grips. Ligament laxity at the thumb’s basal joint often results in dorso-radial translation and can contribute to osteoarthritis (OA). Eaton and Littler (1973) proposed a technique using flexor carpi radialis (FCR) tendon slip for ligament reconstruction [2]. In cases with OA, arthrodesis may be more beneficial, as shown by Pillukat et al. who reported high patient satisfaction with this approach [3]. CMC dislocation is rare due to strong capsuloligamentous structures, primarily stabilized by the anterior oblique and dorso-radial ligaments. Treatment options for acute dislocation include closed reduction, closed reduction with pinning, or open reduction with capsular repair and ligament reconstruction [4]. Persistent instability often requires surgical intervention. Accurate diagnosis relies on history and clinical tests. In our patient, stability was achieved using a Modified Eaton-Littler technique with a suture anchor, reinforcing both the anterior oblique and dorso-radial ligaments with joint capsule for global stability.
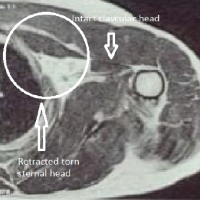
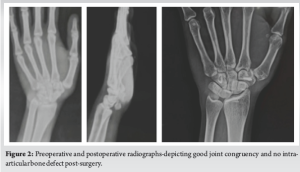
A 20-year-old female patient presented with non-traumatic popping of the metacarpophalangeal (MCP) joint for the past 3 years. She reported being unable to perform strenuous activities due to this condition. There was no history of trauma, negative family history, no signs of ligament laxity; on the other hand, it was normal. Clinically, the patient’s MCP joint demonstrated popping without any external force (Fig. 1). On examination, there were no visible deformities, swelling, or signs of ligament laxity. The ROM was normal in both hands except for the affected MCP joints. Standard radiographs of the hand and MCP joint were taken, which did not reveal any fractures or dislocations (Fig. 2).

Given the chronic nature of her symptoms and lack of trauma history, a conservative approach was initially recommended. Despite conservative management, she continued to experience symptoms, though there was no progression in severity. Future interventions, including possible surgical options, were discussed, and CMC joint stabilisation of the thumb with FCR tendon with suture anchoring was planned.
Surgical technique
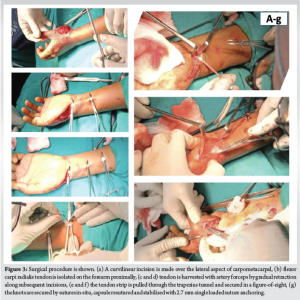
The approach used an anterior curvilinear incision along the CMC joint’s lateral margin from the distal wrist crease up to the FCR tendon. Radial nerve branches, the cutaneous palmar branch of the median nerve, and superficial branches of the radial artery were protected. CMC joint exposure was done by reflecting the thenar muscles extra-periosteally, and the articular surface cartilage was visualized for damage and was found to be healthy and intact. Equidistant mini-incisions were made in the forearm proximally, and the FCR tendon was harvested with artery forceps by gradual retraction along subsequent incisions. FCR tendon hooked along the trapezius and routed through extra-articular bone tunnel along dorsum of the thumb metacarpal parallel to articular surface and along direction of anterior oblique ligament for the purported action FCR tendon sutured covering dorsoradial and volar beak ligament under adequate tensile force (Fig. 3). For additional stability and robust support a single loaded 2.7 mm suture anchor used for capsule stabilization and resuturing, wound closed in layers with protective thumb splint given over 6 weeks, followed by gradual physiotherapy of hand and regular follow-ups at 3 month intervals (Fig. 4).

Over 6 months, the VAS score improved from 6 to 0, the disabilities of the arm, shoulder, and hand score from 77% to 28% postoperatively, and Kapandji score from 4 to 10 [5]. The patient regained power up to grade 4 in CMC joint movements over 3 months with very mild residual pain, followed by complete recovery of energy and painless ROM pre-injury levels at 6 months (Fig. 5). Post-operative recovery was uneventful, with no complications, a complete range of joint mobility of the thumb with no residual instability, and no radiographic evidence of subluxation or arthritic changes.

Post-operative protocol
The post-operative protocol included several stages to ensure optimal recovery. In the immediate postoperative period (0–2 weeks), regular monitoring for signs of infection, pain management, hand elevation, and gentle finger movements to prevent stiffness. The patient was gradually transitioned to a removable CMC orthosis after 2 weeks, thumb opposition exercises started simultaneously, and strengthening exercises were initiated at 3 months. The patient was allowed to return to work 6 months after surgery and was able to oppose her thumb to the base of the small finger (Kapandji score 10) and on radiographic evaluation of thumb – -there was CMC joint alignment with no arthritic changes or intra articular defects.
Patient consent and ethical considerations
Informed consent was obtained from the patient for the publication of this case report and any accompanying images. The patient’s autonomy and right to withdraw consent at any time were respected throughout the process. To ensure confidentiality, all identifying information has been omitted or anonymized for patient privacy and data protection.
The CMC joint of the thumb is a complex saddle joint whose stability is governed by five principal ligaments: the anterior oblique ligament, dorsoradial ligament, first intermetacarpal ligament, posterior oblique ligament, and the ulnar collateral ligament. This case presented a unique challenge due to the chronic instability of the CMC joint without any history of trauma, which is uncommon and often underreported [1,6]. In this particular case, the patient experienced chronic instability of the CMC joint for 3 years without any traumatic event. Eaton and Littler emphasized the importance of the anterior oblique ligament in preventing radio-dorsal subluxation during pinch activities. The absence of a traumatic event in this patient suggests a different etiology, potentially involving a congenital laxity or a degenerative weakening of the ligament [2,7,8]. Using Medline through PubMed a comprehensive literature review was conducted. Several studies highlight different aspects of CMC joint instability and treatment options. Pellegrini et al. (1991) provided evidence that pathological instability, leading to dorsal translation of the metacarpal, significantly contributes to osteoarthritic changes in the CMC joint [2]. Strauch et al. (1994) conducted a cadaveric study that suggested the dorsoradial ligament complex as the primary restraint to dorsal dislocation, which contrasts with the findings in this case where the anterior oblique ligament was the primary concern [4]. This reinforces that injury mechanisms and resultant instability varies with position and nature of force applied to the thumb. Diagnosing CMC joint instability can be complex, particularly when radiographs show a congruent joint, as was seen in this case. Clinical tests, such as the “Torque test” by Eaton and Littler and the two-step provocative test by Takwale et al., are essential for detecting subtler forms of instability that may not be apparent on standard imaging. Advanced imaging modalities, including high-resolution ultrasound and magnetic resonance imaging, have shown promise in providing detailed evaluations of ligament integrity, but their clinical application remains limited and underreported [9-15]. Traditional treatments for traumatic CMC dislocation, including closed reduction and pinning, have shown variable success. The conventional Eaton and Littler Technique is a well-established method with a long history of use and provides stable fixation and good alignment. Modified Eaton and Littler Technique have improved stability compared to the original technique with better outcomes in terms of pain relief and function [2,3]. Compared to open techniques, Mini Tight Rope Technique is minimally invasive and preserves more natural joint motion. It is not suitable for all types of dislocations or severe cases, limited long term durability and outcome data. Arthrodesis is considered in cases of severe instability or arthritis providing more stability and strength, ligament reconstruction with tendon interposition provides better functional outcomes and preserves thumb motion [10,11]. FCR tendon transfer by Eaton and Littler Technique with Suture Anchor Capsule Repair combines stability of traditional methods with modern suture anchor and gives a more robust repair by preserving more of the natural anatomy and joint function. Though this method is a relatively more technically demanding procedure with additional expense due to the use of a single loaded suture anchor [12,13]. While both FCR and APL tendons can be used effectively for chronic CMC joint dislocation, the FCR tendon offers stronger biomechanical stability. FCR reconstructions generally result in better grip strength and stability, whereas APL may have an edge in preserving overall wrist function. In our case, even with FCR harvesting, wrist flexion movements regained normal strength and function by the end of 6 months [14]. This case underscores the complexity of managing chronic CMC joint instability, particularly in the absence of trauma. It highlights the necessity of a thorough clinical evaluation, the use of advanced imaging techniques, and the potential for innovative surgical interventions such as the FCR tendon transfer. The successful outcome in this case supports the use of this technique for similar presentations, providing a valuable addition to the arsenal of treatments available for CMC joint instability. Future research should focus on long-term outcomes and refine diagnostic modalities to identify better and treat this challenging condition.
This case report presents a unique instance of chronic CMC joint instability in the thumb without any history of trauma, managed successfully through the innovative use of the FCR tendon transfer along with 2.7 mm suture anchor for further global capsular stability and support. FCR tendon generally offers stronger biomechanical stability and grip strength as compared to anterior cruciate ligament tendon transfer and the relative wrist flexor weakness is gradually regained post physiotherapy and rehabilitation. It provides a new perspective on addressing chronic joint issues, potentially influencing future clinical practices and research in orthopedics and related fields.
This case report highlights a novel and effective surgical technique for managing chronic CMC joint instability of the thumb using FCR tendon transfer with suture anchor. FCR tendon provides robust stabilisation, restoring function and alleviating pain in patients with insufficient traditional methods offering a new solution for a challenging condition and expanding the repertoire of surgical techniques available for CMC joint stabilisation.
References
- 1.D’Agostino P, Wilson C. Anatomy and biomechanics of the first carpometacarpal joint. J Hand Surg Am 2016;41:108-12. [Google Scholar | PubMed]
- 2.Tomaino, M M; Pellegrini, V D Jr; Burton, R I. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition.. The Journal of Bone & Joint Surgery 77(3):p 346-355, Mar 1995. [Google Scholar | PubMed]
- 3.Pillukat T, Mühldorfer-Fodor M, Fuhrmann R, Windolf J, Van Schoonhoven J. Die arthrodese des daumensattelgelenks. Operative Orthopädie und Traumatologie 2017;29:395-408. [Google Scholar | PubMed]
- 4.Strauch RJ, Behrman MJ, Rosenwasser MP. Acute dislocation of the carpometacarpal joint of the thumb: An anatomic and cadaver study. J Hand Surg Am 1994;19:93-8. [Google Scholar | PubMed]
- 5.Kapandji AI. Clinical evaluation of the thumb’s opposition. J Hand Ther 1992;5:102-6. [Google Scholar | PubMed]
- 6.Simonian PT, Trumble TE. Traumatic dislocation of the thumb carpometacarpal joint: Early ligamentous reconstruction versus closed reduction and pinning. J Hand Surg Am 1996;21:802-6. [Google Scholar | PubMed]
- 7.Burton RI, Pellegrini VD Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am 1986;11:324-32. [Google Scholar | PubMed]
- 8.Sokolowsky T, Freeland AE. Surgical options for the treatment of trapeziometacarpal arthritis. Tech Hand Up Extrem Surg 2009;13:9-14. [Google Scholar | PubMed]
- 9.Kamakura T, Ito H, Goto K, Minami A. Surgical stabilization for thumb carpometacarpal joint arthritis. J Hand Surg Eur Vol 2013;38:57-64. [Google Scholar | PubMed]
- 10.Becker SJ, Briet JP, Hageman MG, Ring D. Death, taxes, and trapeziometacarpal arthrosis. Clin Orthop Relat Res 2014;471:3637-44. [Google Scholar | PubMed]
- 11.Vermeulen GM, Brink SM, Sluiter J, Elias SG, Hovius SE, Moojen TM. Ligament reconstruction arthroplasty for primary thumb carpometacarpal osteoarthritis (Weilby technique): Prospective cohort study. J Hand Surg Am 2009;34:1393-401. [Google Scholar | PubMed]
- 12.Garavaglia G, Dayer R, Haugstvedt JR, Wyrsch P, Giesen T. Arthroscopic hemitrapeziectomy with suture-button suspensionplasty for thumb CMC joint arthritis: A prospective study of 20 cases. J Hand Surg Eur 2010;35:730-5. [Google Scholar | PubMed]
- 13.Kessler I, Hecht O. Carpometacarpal arthroplasty with ligament reconstruction and tendon interposition: Long-term results. J Hand Surg Am 1996;21:216-21. [Google Scholar | PubMed]
- 14.Court T, Hussain K, Kim JS, Patel I, Higginbotham DO, Tsai AG. Systematic review of ligament reconstruction of traumatic isolated thumb carpometacarpal joint dislocation. J Am Acad Orthop Surg Glob Res Rev 2022;6:e22.00103. [Google Scholar | PubMed]
- 15.Takwale VJ, Stanley JK, Shahane SA. Post-traumatic instability of the trapeziometacarpal joint of the thumb. Diagnosis and the results of reconstruction of the beak ligament. The Journal of bone and joint surgery British volume [Internet]. 2004 May;86(4):541–5. [Google Scholar | PubMed]