Surgical treatment of proximal humeral fractures with PHILOS plating results in better functional outcomes.
Dr. Vijayashankar Murugesan, Department of Orthopaedics, Chettinad Hospital and Research Institute, Chettinad Academy of Research and Education, Kelambakkam, Tamil Nadu, India. E-mail: vijayashankar.m@gmail.com
Introduction: Fractures of the proximal humerus are the second most common upper extremity fracture and the third most common fracture, after hip and distal radial fractures. The fractures can occur at any age, but the incidence rapidly increases with age. Common complications following non-operative management of proximal humeral are pain, stiffness, and loss of function. The following study was conducted to evaluate the functional and radiological outcome of displaced proximal humeral fractures treated with the proximal humerus internal locking osteosynthesis system (PHILOS).
Materials and Methods: The study was conducted in patients treated for displaced proximal humerus fracture (Neer’s 2-part, 3-part, 4-part, and associated with dislocation) between the period of April 2022–April 2024. Twenty proximal humerus fracture patients were taken into the study; all were fixed with PHILOS plate. Patients’ ages ranged from 18 to 75 years, with a mean of 53.6 years.
Results: In our study, the sample size of twenty patients of proximal humeral fractures. 10 were males and 10 were females. The patients’ ages ranged from 18 to 75 years, with a mean age of 53.6 years. The causes of fractures were self-fall in 12 patients and road traffic accident in 8 patients. Fourteen fractures involved the right side and 6 involved the left. Patients were followed up from 4 weeks, 12 weeks, and 6 months. Functional outcome was rated as per Constant-Murley Shoulder score, we got excellent results in 07 patients, good in 10 patients, moderate in 02 patients, and poor in 01 patient. The mean Constant-Murley score of this study at the end of the final follow-up period was 81.26.
Conclusion: The majority of proximal humerus fractures in elderly people results from fall on outstretched hand in an osteoporotic bone. As PHILOS plate has options for more number of screws for humeral head than conventional locking plate, it will lead to more stable fixation of fracture fragments and early mobilization of the patients. The functional outcome of Neer’s 2- and 3-part fractures is better than Neer’s 4-part fractures. The radiological outcome, assessed through quality of reduction and bony union, is better in Neer’s 2- and 3-part fractures as compared to Neer’s 4-part fractures. We concluded that proximal humeral fractures, when treated surgically, especially using the PHILOS plate, provided stability, early mobilization, and good range of motion.
Keywords: Proximal humerus fracture, PHILOS plate, constant murley score.
Proximal humerus fractures are fractures occurring at or near the surgical neck of the humerus. This is the most frequently encountered fracture in the shoulder girdle among adults, ranking third after hip and distal radius fractures, which are the first and second most common, respectively [1]. Neer’s classification is clinically applied for classifying these fractures of the proximal humerus, based upon the angulation of the fragments more than 45 and or displacement >10 mm of fragments with respect to one another. It has implications in management and outcome of these fractures [2]. These fractures are a significant source of complications in older adults and should be considered when planning healthcare strategies. Approximately 80% of these fractures are documented to be non-displaced and treated conservatively with plaster of Paris or a cuff and collar sling. The treatment of displaced fractures remains a topic of debate and posing a challenge for orthopedic surgeons. The non-surgical management may be appropriate in 2-, 3-, and 4-part proximal humeral fractures in elderly patients; however, reports indicate that a high percentage of these patients experience pain, stiffness, and decreased function following this approach [3]. CT scans can be beneficial in challenging situations where it is hard to assess the rotation of fragments or the extent of displacements using X-rays [4]. Various fixation methods exist for proximal humerus fractures, including K-wires, screw fixation, buttress plates, conventional plates, locking plates, and prosthetic replacements. Each fixation method comes with its own set of benefits and drawbacks. As a result, there has been recent development of angular stable plates designed to preserve anatomic alignment with secure anchorage, particularly in bones affected by osteoporosis. These are 3-dimensional anatomically designed Proximal Humerus Internal Locking Osteosynthesis System (PHILOS) plate, offering a multidirectional locking mechanism in the humeral head. These implants are capable of supporting physiological forces even in osteoporotic bones, thereby improving the functional recovery [5]. We analyzed the functional and radiological outcomes in patients treated with plate osteosynthesis of proximal humeral fractures and evaluated using the Constant Murley scoring system.
This prospective study was approved by the Institutional Human Ethics Committee, Chettinad Hospital and Research Institute. Twenty-two patients were included in our study. All patients were followed up to a minimum of 6 months and a maximum of 18 months. All patients aged above 18 years with proximal humerus fractures, duration of injury <4 weeks, and treated with PHILOS plate were included in the study. Patients with open proximal humerus fractures, infection, head injury/vascular injury, pathological fracture, and malignancy were excluded. All patients were classified and operated by a senior Orthopedic Surgeon.
Surgical approach
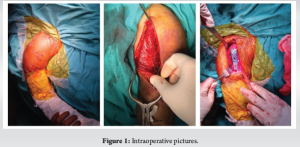
All patients were operated with the standard deltopectoral approach. All patients were positioned supine on the operating table with a sandbag placed between the spine and the medial border of the scapula, pushing the affected side forward, thereby opening the front of the joint. The head end of the table was raised to an angle of 30–45° to minimize bleeding and facilitate blood drainage away from the surgical area. Across the deltopectoral approach, fragments were reduced and temporarily fixed with k wires. After appropriate reduction, the plate was placed at least 8 mm inferior to the greater tuberosity. Then the plate was aligned and fixed with multiple locking or cortical screws. The humeral head is fixed with only cancellous locking screw and infer medial screw calcar screws is important and mandatory for preventing the secondary loss of reduction [Fig. 1]. The final position is checked with the use of an image intensifier in multiple planes. The shoulder is then checked for range of movements and the stability of fixation. None of our patients were required for bone grafting [6]. Intraoperative complications include Fracture of the shaft due to forceful manipulation, displacement of any undisplaced fractures, damage to the deltoid due to retraction, and damage of the axillary artery or nerve.
Post-operative protocol
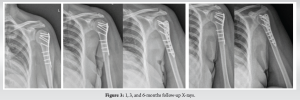
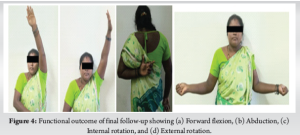
Post-operatively, the arm was immobilized using a shoulder immobilizer for all 20 patients. The time for commencement of shoulder physiotherapy was based on the stability of fixation, quality of bone, and compliance of the patient. Passive range of movement exercises, such as pendulums, passive forward elevation, and external rotation, were generally started on the 1st post-operative day, provided that a stable reduction was achieved. Active range of movements of the elbow, wrist, and hand was also started on the 1st post-operative day. Early passive assisted exercises, active exercises were started at approximately 6 weeks post-operatively and strengthening or resistance exercises started at 10–12 weeks post-operatively. Post-operative X-rays were taken after 24 h of surgery to check the fracture alignment, reduction, and fixation [Fig. 2]. Routine follow-up radiographs were taken after 4 weeks, 3 months, 6 months and 12 months post-operatively to evaluate the features of union, such as disappearance of fracture line, inner column continuity, trabecular continuity, calcar screw status, maintenance of neck shaft angle, and plate related complications, such as screw penetration, screw cut out, avascular necrosis, and implant loosening [Fig. 3,4]. Common post-operative complications are restricted movements associated with pain, operative site infection, fixation failure, avascular necrosis of the head, and sometimes late rupture of the cuff muscles [7].

The study consisted of 10 female and 10 male patients. Four were in the age group of 25–35 (20%), two in the age group of 36–45 (10%), three in the age group of 46–55 (15%), seven in the age group of 56–65 (35%), and four in the age group of 66–75 (20%). Twelve patients (60%) presenting to the hospital had self-fall from standing height as the reason for their proximal humerus fractures. The remaining 8 patients (40%) developed fractures due to road traffic accidents (RTA) (Table 1).
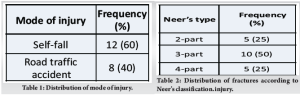
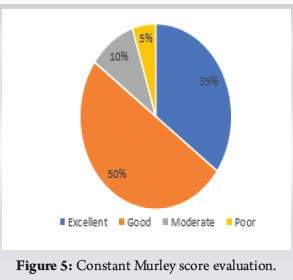
All patients had closed proximal humerus fractures and were classified into Neer’s 2-part, 3-part, and 4-part fractures. The common type of fracture observed in our series was 2-part fracture, accounting for five of twenty patients (25%), along with 3-part fracture, accounting for ten of twenty patients (50%).4-part fracture accounted for five of twenty patients (25%) (Table 2). All patients were evaluated using Constant Murley score and radiographs taken for the proximal part of the humerus. Out of 20 patients, 7 patients had excellent Constant Murley scores, 10 had good scores, 2 had moderate scores, and 1 had a poor outcome score. Mean Constant Murley score is 81.26 (range 60–94 points). Mean constant score for Neer’s 2-part fracture was 85.2 (range 80–94), 3-part fracture was 77.8 (range 62–92), and 4-part fracture was 80.8 (range 60–92). The mean constant score for middle age group (18–40) was 86.4, for old age group (41–60) was 80, and for very old age group (>60) was 78.44 [Fig. 5].
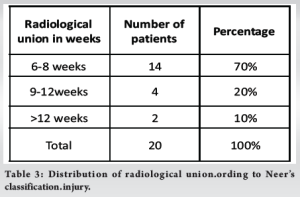
Nineteen out of our twenty patients had fracture union around 9 weeks of follow-up. The average time seen for radiological union of the fracture was 8.4 weeks (6–14 weeks) (Table 3).
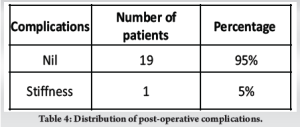
During follow-up, only one patient had post-operative stiffness (5%) (Table 4). There were no incidences of non-union, malunion, implant failure, screw cut-out, neurovascular injury, varus collapse or osteonecrosis of the proximal humeral head.
Approximately 4–5% of all fractures are found to be proximal humeral fracture occurring in two age groups: Younger individuals with high-energy trauma or older individuals with low-velocity injuries, such as falls from standing height. Most often these fractures require open reduction and internal fixation for better results. Functional outcome is always better in isolated fractures than in association with dislocations. K-Wires were the original fracture fixing technique for a very long period, with greater advancements in the development of implants, locking compression plates have now been introduced in the treating proximal humerus fractures. PHILOS plate is the implant of choice used for the fixation of these type of fractures, since it offers options for more numbers of multidirectional screws than conventional locking plate, aiding stability and early mobilization of the patients. The potential complications of using PHILOS plate is screw perforation into glenohumeral joint, screw cut-out, varus malreduction, avascular necrosis in 3-part and 4-part fractures, stiffness, sub-acromial impingement, difficult revision surgery. The 20 individuals included in the study had a mean age of 53.6 ± 14.56 years. The research study conducted by Saber et al. and Kaliraj et al. on a sample of 20 patients had a mean age of 57, 51–55.3 years, respectively [8,9]. Our analysis revealed that the side affected was right in 16 patients, while the side affected was left in 4 patients. Almost all the other studies by Deepak et al. and Ethiraj et al. showed right-handed dominance. In contrast to our study and other studies, Martinez et al. found that the majority of the injury was in the left-hand side, consisting of 28 out of 46 patients [10-12]. The cause of injury was commonly seen to be self-falls and Road Traffic accidents. The patients sustaining proximal humeral fractures by self-fall may be attributed to osteoporosis in the elderly. This makes such injuries difficult to manage. Fractures due to RTA are due to high velocity, and such injuries are most often comminuted with complex fracture patterns. The type of fracture sustained by the patients was described by Neer’s classification score with the following fracture pattern as observed in the present study and the other related studies [12-14]. These studies show that most of the fractures are either 3-part or 4-part as per Neer’s classification. As proximal humerus fractures are most often found in the elderly population, they are associated with comorbidities. In the present study, 15 % of patients had diabetes mellitus and 10% had associated systemic hypertension. Mootha et al. study patients were associated with diabetes mellitus in 10% and systemic hypertension in 20%, which was more likely same as that compared with our study [15]. The time to bony union in the studies conducted ranged from 8 to 13 weeks based upon the type of fracture. The functional outcome of the patients treated by PHILOS plate fixation was analyzed by using the Constant Murley score. The outcome results in the present and other related studies are as follows. It was observed from the various studies, including our study that the fractures fixed with a plate seem to have excellent to good results in at least 80% of the patients who underwent the procedure. The patients with fair and poor results are due to fracture in severely osteoporotic bones or due to complex fractures, such as Neer’s 4-part fracture. In the present study, conducted to evaluate the final outcome of plate osteosynthesis for proximal humeral fractures, complication after the surgery was stiffness with only one patient, with no other complications. Studies by Saber et al. and Ethiraj et al. also had only one case with shoulder stiffness, whereas Deepak et al’s. study had 20 cases with stiffness, which was very higher when compared with our present study [8,10,11].
Our study found that proximal humerus fractures have a bimodal age distribution, occurring in two age groups of younger individuals with high-energy trauma and older individuals with low-energy injuries, such as falls from standing height. Locking compression plates, such as PHILOS plate have option for multidirectional locking screws in the humeral head than other conventional locking plate and are the preferred treatment for fixation of proximal humeral fractures. Functional and radiological outcomes in Neer’s 2- and 3-part fractures are better than 4-part proximal humerus fractures treated with PHILOS plate. Plate osteosynthesis of the proximal humeral fractures with PHILOS plating provides good stability for early mobilization, good range of movements, and hence leads to less stiffness of the shoulder joint.
Surgical treatment of proximal humeral fractures using PHILOS plating offers improved stability, facilitates early mobilization, reduces shoulder joint stiffness, and enhances the range of motion.
References
- 1.Pencle F, Varacallo MA. Proximl humerus fracture. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: http://www.ncbi.nlm.nih.gov/books/nbk470346 [Last accessed on 2025 Apr 24]. [Google Scholar | PubMed]
- 2.Carofino BC, Leopold SS. Classifications in brief: The neer classification for proximal humerus fractures. Clin Orthop Relat Res 2013;471:39-43. [Google Scholar | PubMed]
- 3.Schumaier A, Grawe B. Proximal humerus fractures: Evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil 2018;9. [Google Scholar | PubMed]
- 4.ResearchGate. (PDF) Three-Dimensional Measurement of Proximal Humerus Fractures Displacement: A Computerized Analysis. Available from: https://www.researchgate.net/publication/371647097_three/dimensional_measurement_of_proximal_humerus_fractures_displacement_a_computerized_analysis [Last accessed on 2025 Apr 24]. [Google Scholar | PubMed]
- 5.Aliuddin AM, Idrees Z, Rahim Najjad MK, Ali Shah SA. Functional outcome of proximal humeral fractures treated with philos plate in adults. J Ayub Med Coll Abbottabad 2016;28:337-40. [Google Scholar | PubMed]
- 6.Robinson CM, Murray IR. The extended deltoid-splitting approach to the proximal humerus: Variations and extensions. J Bone Joint Surg Br 2011;93:387-92. [Google Scholar | PubMed]
- 7.Ziegler P, Kühle L, Stöckle U, Wintermeyer E, Stollhof LE, Ihle C, et al. Evaluation of the Constant score: Which is the method to assess the objective strength? BMC Musculoskelet Disord 2019;20:403. [Google Scholar | PubMed]
- 8.Saber AY, Said UN, Abdelmonem AH, Elsayed H, Taha M, Hussein W, et al. Surgical fixation of three- and four-part proximal humeral fractures using the proximal humeral interlocking system plate. Cureus 2022;14:e25348. [Google Scholar | PubMed]
- 9.Kaliraj G, Praveen Kumar D, Sathish M. Outcome analysis of proximal humerus internal locking osteosynthesis system (PHILOS) in management of proximal humerus fractures. IOSR J Dent Med Sci 2017;16:23-8. [Google Scholar | PubMed]
- 10.Deepak CD, Mahesh DV, Ravoof A, Baruah MJ. Functional outcome of displaced proximal humerus fractures managed by proximal humerus interlocking system plate. Int J Res Orthop 2017;3:583-8. [Google Scholar | PubMed]
- 11.Ethiraj P, Venkataraman S, Karthik SJ, Shanthappa AH, Agarawal S. Does proximal humerus inter locking system (PHILOS) plating provide a good functional outcome in proximal humerus fractures? Cureus 2022;14:e26474. [Google Scholar | PubMed]
- 12.Martinez AA, Cuenca J, Herrera A. Philos plate fixation for proximal humeral fractures. J Orthop Surg Hong Kong 2009;17:10-4. [Google Scholar | PubMed]
- 13.Functional Outcome of Proximal Humerus Fracture Management with Proximal Humerus Internal Locking System Plate. Available from: https://www.researchgate.net/publication/353602844_functional_outcome_of_proximal_humerus_fracture_management_with_proximal_humerus_internal_locking_system_plate [Last accessed on 2025 Apr 24]. [Google Scholar | PubMed]
- 14.Vijayvargiya M, Pathak A, Gaur S. Outcome analysis of locking plate fixation in proximal humerus fracture. J Clin Diagn Res 2016;10:RC01-5. [Google Scholar | PubMed]
- 15.Mootha AK, Ramana Kumar KV, Saisaran Kumar B, Lavanya B. A prospective study of outcome of fracture of proximal humerus treated with PHILOS plating. Int J Orthop Sci 2021;7:109-12. [Google Scholar | PubMed]