A osteonecrotic lesion can mimic a malignant lesion on PET CT in vertebral body.
Dr. Arvind G Kulkarni, Mumbai Spine Scoliosis and Disc Replacement Centre, Bombay Hospital and Medical Research Centre, Marine Lines, Mumbai, India. E-mail: drarvindspines@gmail.com
Introduction: Occurrence of a focal lytic lesion which is “hot” on positron emission tomography (PET) scan is presumed to be neoplastic until proven otherwise. Focal osteonecrosis of vertebral body (VB) without collapse is a rare entity with sparse literature available.
Case Report: A focal osteolytic lesion in a patient with a history of breast carcinoma, in remission, thought to be metastatic lesion on magnetic resonance imaging and PET-computed tomography (CT), with an inconclusive CT-guided biopsy, was found to be osteonecrosis on histopathology of aggregates of tissue obtained from the T9 VB during open surgery.
Conclusion: Osteonecrosis without a VB collapse is a rare diagnosis, but should be considered a differential when examining suspected metastatic lesions in VB.
Keywords: osteonecrosis, vertebrae, PET CT, metastasis
Bone tissue necrosis or osteonecrosis is an abnormality that can occur whenever a disease process causes major cell stress. This entity involves massive necrosis of the bone and bone marrow [1]. Although multiple theories have been proposed concerning this condition’s etiology, none have been confidently established. However, it is believed to be multifactorial [2]. The most common sites for avascular necrosis are the femoral head, knee, talus, and humeral head [3]. In the context of vertebral body (VB) osteonecrosis, literature is sparse and the actual incidence remains unknown [4]. In the VB, post-traumatic vascular disruption is considered one of the most common mechanisms for osteonecrosis [1]. Therefore, osteonecrosis in the VB is usually described in the setting of a clearly demonstrable moderate/severe fracture with progressive kyphosis, also called Kummell’s disease [5]. However, to the authors knowledge, only four cases have been reported in literature on osteonecrosis of VB without any collapse or demonstrable fracture on imaging [6,7]. In case of a necrotic lesion found in the VB, the diagnosis purely with imaging can become challenging as it is not been able to adequately distinguish it from other entities. Some describe gaseous collection on radiographs in the VB as pathognomonic for VB necrosis [8], while others report that this collection is also seen in infection and malignancy [9]. Histopathology remains the gold standard for diagnosis [10]. We present a case of idiopathic, focal, VB osteonecrosis in non-collapsed T9 vertebrae of a 51-year-old breast cancer surviving female, mimicking a metastatic malignancy on imaging.
Statement of informed consent
The patient was informed that her data would be collected and sent for publication, the patient had assented to this, and signed informed consent was obtained.
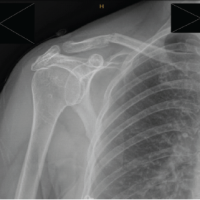
We present the case of a 51-year-old female with acute-onset severe upper back pain for 3 months before presentation. She was a known case of adenocarcinoma of the breast, for which she underwent a surgery in 2014 and has been reportedly cancer free since then. She was on chemotherapy of tamoxifen till June 2022. Pain was localized to the upper back, which worsened in the morning. Pain was without any radiation or mechanical symptoms. She felt partial relief on medication and after walking a few steps. There was no history of trauma and no previous history of such episodes. Current medications included only a daily oral dose of thyroxine supplementation. The patient had tenderness to deep palpation over the dorsolumbar region. There was no significant neurology or bowel/bladder involvement. Laboratory assessment revealed no significant findings including a negative M band. Magnetic resonance imaging (MRI) of the lesion was performed (Fig. 1 and 2).
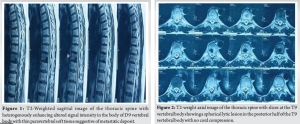
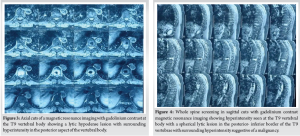
Additional gadolinium contrast (Fig. 3 and 4) was then done, which showed a focal lytic lesion in the T9 VB. This lesion was hypointense on T1- and T2-weighted images and showed heterogeneous enhancement on gadolinium contrast images. A metastatic deposit was suspected. A positron emission tomography–computed tomography (PET-CT) was then performed (Fig. 5 and 6), which reported focal 15F-FDG uptake in the body of T9 vertebrae. Differential of this nodule was inflammatory, infective, or metastatic.

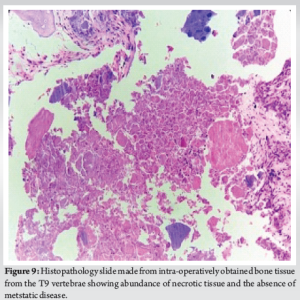
A CT-guided biopsy yielded no organism growth, and histopathology sample was reported as necrotic bone with normal marrow elements, with immunohistochemistry negative for tumor markers. At the end of this thorough investigation protocol, the primary surgeon was unconvinced with the CT-guided biopsy report suspecting inadequate sampling. The patient underwent an open debridement and screw-rod fixation at D8 and D10 with graft placement at hollow debridement site (Fig. 7). Sample of size 2 cm3 collected during the surgery was sent for histopathology (Fig. 8 and 9) which reported it to be necrotic bone with regenerating woven bone intervened by fibroblastic reaction and there seemed to be no evidence of tuberculosis or metastasis.
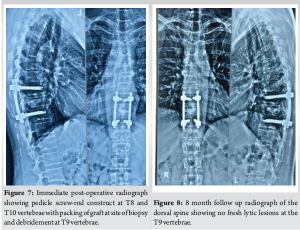
At 8 months post-surgery, (Fig. 8) X-ray was performed which showed no further collapse and although no repeat MRI scan has been performed, there has been no evidence of recurrence on plain radiographs and patient has not suffered any recurrent pain episodes.
The standard approach in cases suspicious of malignancy was followed, with an MRI, CT and a PET-CT Scan being performed. The likely DD’s were a primary neoplastic focus or a metastatic disease presenting with a focal lytic lesion. Therefore, a biopsy was performed to confirm the diagnosis. In this case, suspicion of malignancy was high, especially based on history of the patient of breast cancer and the PET CT report which noted a hot-spot at the site of the lesion. In fact, the intra-vertebral vacuum cleft sign that is considered a hallmark for osteonecrosis in imaging, produces a cold defect on the bone scan [11], making it especially striking that this lesion presented as “hot” on PET-CT. We found only one other case in literature that had such a hot spot in the thoracic spine on PET in case of VB osteonecrosis [7]. In that case, the 24 year old patient presented with transient avidity on 18F-FDG PET initially interpreted as extra-nodal disease in a case of non-Hodgkins lymphoma. In our case, however, the transient nature of PET hyperintensity was not observed as PET was done 4–5 weeks after the onset of symptoms and the nodule was still “hot”. In the cases reported by Murakami et al. [6], none were in the thoracic spine. However, all cases had lesions which were hypointense on T1 and hyperintense on T2-weighted images with no enhancement on Gadolinium contrast infusion. Bone scan in those cases too did not show any uptake. These findings are significantly different from our case where there was T1 and T2 hypointensity with enhancement on contrast administration as well as a hot spot on PET-CT.
Little is known about the entity of VB osteonecrosis. It is evident that radiological findings can vary from patient to patient and can often mimic metastatic tissue and do therefore, do not provide a confident enough guidance with respect to the diagnosis. Our study shows a rare-er presentation of an already rare entity. This diagnosis on radiology can be devastating for the patient and challenging for the surgeons. The cause, preferred method of non-invasive diagnosis and optimal management of this condition is unknown.
Osteonecrosis of VB without collapse is a rare diagnosis, this necrotic segment being “hot” on PET CT is even rarer. An appropriate biopsy should be performed before undertaking final surgery and fixation one level above and below has shown to be a stable fixation in this case.
References
- 1.Lafforgue P. Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine 2006;73:500-7. [Google Scholar | PubMed]
- 2.Kenzora JE, Glimcher MJ. Accumulative cell stress: The multifactorial etiology of idiopathic osteonecrosis. Orthop Clin North Am 1985;16:669-79. [Google Scholar | PubMed]
- 3.Matthews AH, et al. Avascular necrosis. In: StatPearls. Treasure Island, FL: StatPearls; 2023. [Google Scholar | PubMed]
- 4.Formica M, Zanirato A, Cavagnaro L, Basso M, Divano S, Formica C, et al. What is the current evidence on vertebral body osteonecrosis? A systematic review of the literature. Asian Spine J 2018;12:586-99. [Google Scholar | PubMed]
- 5.Lim J, Choi SW, Youm JY, Kwon HJ, Kim SH, Koh HS. Posttraumatic delayed vertebral collapse: Kummell’s disease. J Korean Neurosurg Soc 2018;61:1-9. [Google Scholar | PubMed]
- 6.Murakami H, Kawahara N, Gabata T, Nambu K, Tomita K. Vertebral body osteonecrosis without vertebral collapse. Spine (Phila Pa 1976) 2003;28:E323-8. [Google Scholar | PubMed]
- 7.Chaudhary K, Ngai S. Vertebral body osteonecrosis mimicking malignant disease on 18F-FDG PET. Clin Nucl Med 2023;48:e115-7. [Google Scholar | PubMed]
- 8.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: A sign of ischemic vertebral collapse. Radiology 1978;129:23-9. [Google Scholar | PubMed]
- 9.Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol 2005;26:1634-40. [Google Scholar | PubMed]
- 10.Lin CL, Lin RM, Huang KY, Yan JJ, Yan YS. MRI fluid sign is reliable in correlation with osteonecrosis after vertebral fractures: A histopathologic study. Eur Spine J 2013;22:1617-23. [Google Scholar | PubMed]
- 11.Kim H, Jun S, Park SK, Kim GT, Park SH. Intravertebral vacuum cleft sign: A cause of vertebral cold defect on bone scan. Skeletal Radiol 2016;45:707-12. [Google Scholar | PubMed]