Significant short- and long-term repercussions can result from pelvic injuries. PROMs are useful for evaluating the long-term consequences of such injuries. It is crucial to use these outcome metrics wisely in order to understand the complete picture
Dr. Lav Mehta, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India. E-mail: mehta.lav@gmail.com
Introduction: Pelvic ring injuries lead to significant patient morbidity and mortality. We evaluated long-term (>1 year) functional outcome of these patients using patient-reported outcome measures) using both generic health-specific and disease-specific outcome instruments.
Materials and Methods: Pelvic ring injury patients seen between 2015 and 2020 were called for a follow-up visit. Patient’s demographic profile, mode and pattern of injury, associated injuries, management, and complications were recorded. Functional outcome assessment was made using two generic health-specific scores (SF-36 and short musculoskeletal functional assessment [SMFA]) and three disease-specific scores (Majeed pelvic score [MPS], Iowa pelvic score [IPS], and pelvic discomfort index [PDI]). Statistical analysis was performed to find the correlation between the two types of scoring systems. SF-36 scores of the study population were compared with normative data from the general population.
Results: Of 56 patients (37 males, 19 females, mean age 32 years), there were 40 Tile B type and 16 Tile C type. 27 patients had other orthopaedic injuries, while 24 had nonorthopaedic injuries (14 – urological). 42 patients were operated and 14 were conservatively managed. The mean follow-up duration was 26.8 months. Mean (standard deviation [SD]) SF-36 physical component summary score was 64.01 (22.89) and mental component summary score was 63.79 (23.31). SMFA dysfunction index and SMFA bother index mean (SD) were 22.41 ± 11.75 and 25.97 ± 14.12, respectively. Mean (SD) MPS came as 85.93 (12.89) with 37 patients graded as ”excellent.” The mean (SD) of IPS and PDI scores were 78.61 (9.40) and 21.70 (16.59), respectively. There was no statistical difference between the two types of scores when assessed using Spearman correlation tests. However, on comparison of study population mean SF-36 subset scores with general population norms, no domain of SF-36 could reach norm values. MPS cutoff of >85 (“excellent” outcome) could not include in itself a sufficient percentage of population with at-par SF-36 scores. Long-term sequelae of trauma were significantly associated with poor quality of life scores.
Conclusion: Long-term physical functioning and quality of life in patients with pelvic ring injuries seem to be fair, although they are significantly lower than that of their peers in the general population.
Keywords: Pelvic fracture, disease-specific scores, generic health-specific scores, SF-36, Majeed pelvic score.
Among all fractures and bone injuries, pelvic fractures are among the most serious. It accounts for 1.5–3% of all bone injuries [1]. The incidence of pelvic fractures in polytrauma patients is about 25% [2]. The spectrum of pelvic fractures and their long-term prognosis is not well covered in the literature, particularly when it comes to the Indian population. In a polytraumatized patient, pelvic ring injuries are typically seen as a single element of multiple system injuries; as a result, measuring the functional outcome using only disease-specific outcome scores is not entirely appropriate because other injuries besides those to the pelvis will also have an impact on the functional outcome. Conventionally, the most commonly used outcome measure in these patients is the disease-specific Majeed pelvic score (MPS). Other disease-specific outcome scores used are the Iowa pelvic score (IPS) and the Pelvic discomfort index (PDI). We believe that using generic health-related outcome scores, like the SF-36 and short musculoskeletal functional assessment (SMFA), for all outcome studies is the best strategy to assess patients with pelvic injuries. Yet, an orthopaedic surgeon is constantly drawn to the bone aspect of polytrauma, and as a result, the disease-specific pelvic outcome ratings are more frequently used. In our clinical practice, pelvic trauma patients who had a “good” or “excellent” disease-specific outcome score and an acceptable post-operative radiographic decrease were frequently encountered on follow-up. However, after interacting with these patients, we frequently notice that they have not recovered to their pre-injury level of physical and/or mental functioning. We designed this study to address this frequently occurring clinical scenario, in which we would assess both disease-specific scores (Majeed score, IPS, PDA) and generic health-specific outcome instruments (SF-36, SMFA) on a comparatively larger patient group. This study’s objectives were to assess the long-term patient reported functional outcome (follow-up – minimum 1 year) following pelvic ring fractures and to compare the disease-specific scores (Majeed score, IPS, PDA) to generic health-specific instruments (SF-36, SMFA), in order to determine which of the three disease-specific scores – Majeed score, IPS, and PDA – would be the most accurate in correlating with these generic instruments. Since earlier research has historically not employed generic health-specific instruments, this has enormous academic relevance. We would also compare the generic health-specific scores of our study population with Indian general population norms [3].
Study design
It was a cross-sectional observational study conducted on a patient population that presented to a tertiary level trauma centre, regardless of the type of pelvic injury and treatment given, and with a minimum of 1 year of follow-up.
Setting
We identified all patients with pelvic ring fractures who were admitted to a single level 3 trauma centre between 2015 and 2020. All patients who were above 18 years. and with follow-up duration of more than 1 year were included. Eligible patients were called for a single follow-up visit. Each patient’s personal and clinical data, including gender, age, comorbidities, treatment received, type of surgery (isolated posterior or combined anterior–posterior fixation), concurrent injuries and surgeries, surgical complications, length of hospital stay, injury to weight bearing duration, and follow-up period, were gathered.
Participants
Patients with pathological/stress fractures of the pelvis were excluded from the study. A total of 110 patients responded out of the available data of 168 patients. 10 patients did not fulfil our inclusion criteria and 56 patients who were eligible, came for a follow-up visit and were included in this study.
Outcome scores
Both disease-specific and general health-specific scoring methods were used to record functional outcomes. MPS, IPS, and PDI were the disease-specific outcome measures used. SF-36 and SMFA were the generic health-specific scores used. The PDI comprises six questions regarding issues with pain, walking, hip motion, leg sensation, scar tissue from the pelvic region, and sexual problems. A six-level scale, ranging from no discomfort to extremely uncomfortable, is used to score each question. On completion, an index is created that ranges from 0% (best) to 100% (worst) in terms of pelvic discomfort. The SF-36 is a well validated and reliable general health assessment survey consisting of 36 questions divided into eight subscales: Physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health. The physical component summary (PCS) for physical health can be created by combining the first four subscales, and the mental component summary (MCS) for mental health can be created by combining the last four subscales. The SMFA is a brief functional status assessment tool created for use in community-based outcome studies and in the treatment of individual patients with musculoskeletal disorders. It consists of 34 functional items comprising the dysfunction index and the twelve items comprising the bother index.
Statistical methods
All the data was tabulated in Microsoft Excel spreadsheet program. Statistical Packages for the Social Sciences v23 (IBM Corp.) was used for data analysis. Descriptive statistics of the study were elaborated in the form of means/standard deviations and medians/IQRs for continuous variables, and frequencies and percentages for categorical variables. When comparing two groups of continuously distributed data, independent sample “t” test was used. Non-normally distributed data was analysed using appropriate non-parametric tests in the form of the Wilcoxon Test were used. Chi-squared test was used for group comparisons for categorical data. When the expected frequency in the contingency tables was found to be <5 for >25% of the cells, Fisher’s Exact test was used instead. Nonparametric tests (Spearman Correlation) were used to compare the two types of scoring systems used, i.e., generic health-specific outcome scores (SF-36, SMFA) and disease-specific outcome scores (MPS, IPS, and PDI score). Statistical significance was kept at P < 0.05.
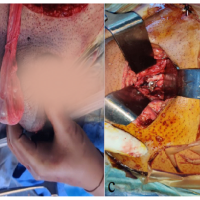
Participants Fig. 1

Descriptive data
There were 37 male and 19 female patients with an average age of 32 (range, 18–61) years. RTA was the most common mode (40 patients), followed by fall from height [4] followed by fall of heavy object [5]. 24 patients had other significant non- orthopaedic injuries, of which, urological injuries were the most common [6]. There were 40 patients with type-B pelvic fractures and 16 patients with type-C pelvic fractures according to Tile’s classification. As per the young and burgess classification, there were 31 lateral compression LC1–16 LC2–10, LC3–5, 14 anteroposterior compression, APC1–3, APC2–5 APC3–6, 8 vertical shear, and 3 combined mechanisms. The attending surgeon’s preference determined the initial course of treatment. Out of the 56 patients, 14 had conservative care, and 42 underwent surgery. On their single follow-up appointment, patients completed all of the aforementioned outcome measuring questionnaires. The average number of follow-up months was 26.8 (with a range of 12–50).
Main results
The average of MPS in our study population was 85.93 (range 49–100). 37 patients were graded “excellent” as per MPS outcome grading, and 11 patients had “good” outcome (Table 1). On analysis of response to MPS question regarding present day work, we found that only 14 patients, which constitutes 25% of the study population, could return back to same job with same performance and 20 patients (35.7%) were able to return to same job but with somewhat reduced performance.
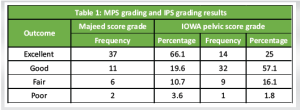
The average IPS of our study population came out to be 78.61, which when graded as per Nepola et al. [5] represents overall “good” outcome. 32 patients came under IPS “Good” outcome grade, whereas 14 were graded as “excellent” outcome (Table 1).
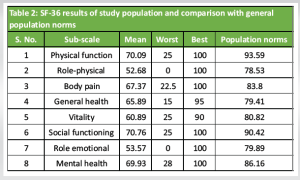
The average value of the PDI score in our study population was calculated to be 21.7, signifying overall “moderate” residual pelvic discomfort in our study cohort. SMFA score average of our study population was 48.38 with an average discomfort index score of 22.41 and average bother index score of 25.97. The average PCS of the SF-36 was 64.01 (range- 15.62–95) points and the average MCS of the SF-36 was 63.79 (range- 20.75–95.25) points. On Comparison with average population norms of the Indian population, we found that mean scores of our study population could not achieve the population norms in any of the 8 sub-scales of the SF-36 score (Table 2). 9% of our study population was able to reach population norm of the physical function subscale (least), whereas 37.5% of the study population had role emotional subscale score at par with Indian population norm.
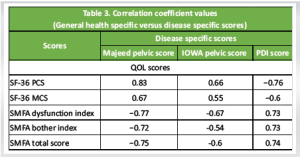
Correlation between the disease-specific and generic health-specific scores
As inferred from the Spearman correlation coefficients given in Table 3 below and the P-values, there was a significant correlation (P < 0.001) between generic health-specific and disease-specific outcome scores when used in our study population. MPS had the best correlation coefficient to all generic health-specific scores compared to IPS and PDI score.
Using statistical techniques, we attempted to estimate the proportion of the study population whose SF-36 subscale score was within the range of the general population norm after grouping them according to their total MPS. The results are shown in Table 5.
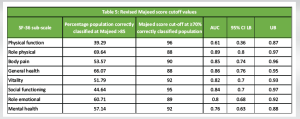
Table 5 depicts that the MPS grading system, with more than 85 score being graded as excellent, clearly does not corroborate with generic health-specific scores such as SF-36. Only in a single sub-scale of role physical, Majeed’s score cut off of 85 could include in itself, 70% of the study population with SF-36 score at par with that of the general population. This analysis shows that in spite of being no statistical difference, the two types of outcomes scoring systems should not be used independently to avoid misuse of the term such as an “excellent” outcome.
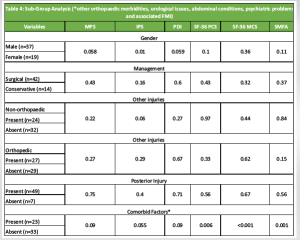
Pelvic ring fractures can be a significant cause of patient morbidity and mortality [7]. Pelvic fractures can range in energy from low-energy pubic ramus fractures to high-energy unstable patterns that can result in substantial bleeding and mortality. It wouldn’t be erroneous to argue that the main goal of treatment for unstable pelvic ring fractures has historically been the patients’ survival. The present report, however, is concentrated on researching the long-term results when morbidity following pelvic fracture is a concern. Contrary to other fracture patterns, the degree of patient satisfaction following pelvic ring fractures depends not only on the success of anatomical fracture reduction and the restoration of mechanical function but also on a number of biosocial and psychological effects connected to the impairment of non-biomechanical function, including urinary, bowel, sexual, neurological dysfunction, activities of daily living, pain, and return to work. To establish the patients’ subjective and objective health status, it is crucial to apply health measurement scoring systems. However, we could find no study that has used more than three outcome measurement scores along with a combination of both generic and disease specific scores. Mean MPS of our study population was 85.93 ± 12.89 (range: 49.00–100), which is comparable to values seen in other long-term outcome studies (Petryla et al. [8], Moon et al. [9], Soni et al. [10]). Similarly, the mean IPS of the population in our study was 78.61 ± 9.40. This is in agreement with other studies (Suzuki et al. [11], Nepola et al. [5]) in which IPS has been used. The mean SMFA score in our study population was 48.38 ± 25.26. Our results are comparable to the results of the other studies, such as Sagi et al. [12] (SMFA mean total score = 45) and Hermans et al. [13] (SMFA mean total = 48). The mean SMFA dysfunction index in our study population was 22.41 ± 11.75. It can be interpreted as “fair” quality of life, as per Badra et al. [4]. The mean SF-36 PCS score in our study was 64.01 ± 22.89 and the mean MCS score was 63.79 ± 23.31. The mean PCS score of the study population is comparable to the scores seen in other studies, such as Suzuki et al. [11] and Oliver et al. [14]. However, mean MCS score in our study population was lower than the scores seen in previous studies such as Ayvaj et al. [6] and Oliver et al. [14]. On comparing SF-36 scores with general population norms, there was a significant difference seen (P < 0.05). These findings are in agreement with the studies that have earlier compared the SF-36 scores of their study population consisting of pelvic ring fracture patients with their country’s general population norm scores. Few of these studies include Ayvaj et al. [6], Bosch et al. [15], Suzuki et al. [11] and Oliver et al. [14]. The ever-growing and unsolved debate of generic versus disease-specific outcome measurement scores in pelvic trauma patients has been analyzed by authors such as Lefaivre et al. [16], Lumsdaine et al. [17] and Banierink et al. [18]. All of these studies have taken the SF-36 score as the standard outcome measuring instrument and they have compared the disease-specific scores such as MPS, IPS, Orlando pelvic score etc. with the SF-36 score. Highlights of the drawbacks of disease-specific scores that these studies have found include: Failure to capture emotional and mental outcome as a consequence of the injury, ceiling effect and lack of proven validity, reliability, and responsiveness. According to Banierink et al. [18], disease-specific scores have been used in most of the studies (n = 38) as compared to generic patient reported outcome measures (n = 15) with MPS being the most commonly used score. The MPS had the best correlation coefficient among the disease-specific scores when compared to generic healthspecific outcome scores, according to statistical methodologies utilized in this study to determine the correlation between two types of scores (Table 3). However, on further probing of patients with excellent (n = 37) and good (n = 11) MPS outcomes, we found a high proportion of patients with dissatisfaction related to their overall outcome post injury (Table 4).
In an attempt to find a more appropriate cutoff value for “excellent” Majeed score, we plotted ROC curves for each SF- 36 sub scale score of the Indian population in comparison with MPS total score and the results are shown in Table 5. With a median MPS score value of 91 being able to corroborate well with SF-36 norm values in at least 70% of the study population, we feel the new “excellent” grading score should be set at a minimum total score of 91. The SF-36 helps obtain a patient’s assessment of general disability, discomfort, and emotional state, although it does not include specific observations that may be limited after a hip fracture. The present study’s findings are consistent with the idea that a more thorough evaluation of patient outcomes can be achieved by correlating health-related quality-of-life parameters that are both generic and injury specific.
Functional outcome after pelvic ring fractures was weakly associated with age, not associated with gender, fracture pattern, or mode of injury. In our study, we also did not discover any differences in outcome between individuals who underwent surgery and those who received conservative treatment. However, the presence of any persistent co-morbidity/health-related factor such as long-term residual effects of the trauma, significantly affected the functional outcome, especially the generic health-specific scores such as SF-36 and SMFA (Table 4). Despite the fact that there was a statistical association between the disease-specific and generic health-specific outcome scores, there was a disparity. We conclude terms “excellent” MPS should be read in conjunction with the quality-of-life scores to know the comprehensive functional outcome after pelvic ring fracture.
Pelvic ring injuries significantly impact long-term patient-reported functional outcomes, even when anatomical reduction and surgical management are deemed successful. Despite a high percentage of patients scoring “excellent” on disease-specific outcome measures (such as the MPS), their overall quality of life remains significantly lower than general population norms, as assessed by generic health-specific outcome tools (such as SF-36 and SMFA). This highlights the necessity of integrating both disease-specific and generic health-specific outcome measures to comprehensively evaluate recovery. The study suggests reconsidering the threshold for an “excellent” outcome in the MPS to better align with patient-reported quality of life.
References
- 1.Hodgson S. AO principles of fracture management. Ann R Coll Surg Engl 2009;91:448-9. [Google Scholar | PubMed]
- 2.McMurtry R, Walton D, Dickinson D, Kellam J, Tile M. Pelvic disruption in the polytraumatized patient: A management protocol. Clin Orthop Relat Res 1980;151:22-30. [Google Scholar | PubMed]
- 3.Sinha R, Van Den Heuvel WJ, Arokiasamy P. Validity and reliability of MOS short form health survey (SF-36) for use in India. Indian J Community Med 2013;38:22-6. [Google Scholar | PubMed]
- 4.Badra MI, Anand A, Straight JJ, Sala DA, Ruchelsman DE, Feldman DS. Functional outcome in adult patients following Bernese periacetabular osteotomy. Orthopedics 2008;31:69. [Google Scholar | PubMed]
- 5.Nepola JV, Trenhaile SW, Miranda MA, Butterfield SL, Fredericks DC, Riemer BL. Vertical shear injuries: Is there a relationship between residual displacement and functional outcome? J Trauma 1999;46:1024-9; discussion 1029-30. [Google Scholar | PubMed]
- 6.Ayvaz M, Cağlar O, Yılmaz G, Güvendik GI, Acaroğlu RE. Long-term outcome and quality of life of patients with unstable pelvic fractures treated by closed reduction and percutaneous fixation. Ulus Travma Acil Cerrahi Derg 2011;17:261-6. [Google Scholar | PubMed]
- 7.Sathy AK, Starr AJ, Smith WR, Elliott A, Agudelo J, Reinert CM, et al. The effect of pelvic fracture on mortality after trauma: An analysis of 63,000 trauma patients. J Bone Joint Surg Am 2009;91:2803-10. [Google Scholar | PubMed]
- 8.Petryla G, Uvarovas V, Bobina R, Kurtinaitis J, Puronaitė R, Kvederas G, et al. Comparison of one-year functional outcomes and quality of life between posterior pelvic ring fixation and combined anterior-posterior pelvic ring fixation after lateral compression (B2 type) pelvic fracture. Medicina (Kaunas) 2021;57:204. [Google Scholar | PubMed]
- 9.Moon DH, Kim NK, Won JS, Choi JS, Kim DH. Outcome of surgical treatment of AO type C pelvic ring injury. Hip Pelvis 2014;26:269-74. [Google Scholar | PubMed]
- 10.Soni A, Gupta R, Kapoor L, Vashisht S. Functional outcome of ‘LC-1 pelvic ring injury with incomplete sacral fracture’ managed non-operatively. J Clin Orthop Trauma 2020;11:S1-3. [Google Scholar | PubMed]
- 11.Suzuki T, Shindo M, Soma K, Minehara H, Nakamura K, Uchino M, et al. Long-term functional outcome after unstable pelvic ring fracture. J Trauma 2007;63:884-8. [Google Scholar | PubMed]
- 12.Sagi HC, Militano U, Caron T, Lindvall E. A comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma 2009;23:313-9; discussion 319-321. [Google Scholar | PubMed]
- 13.Hermans E, Brouwers L, Van Gent T, Biert J, De Jongh MA, Lansink KW, et al. Quality of life after pelvic ring fractures: Long-term outcomes. A multicentre study. Injury 2019;50:1216-22. [Google Scholar | PubMed]
- 14.Oliver CW, Twaddle B, Agel J, Routt ML Jr. Outcome after pelvic ring fractures: Evaluation using the medical outcomes short form SF-36. Injury 1996;27:635-41. [Google Scholar | PubMed]
- 15.Van Den Bosch EW, Van Der Kleyn R, Hogervorst M, Van Vugt AB. Functional outcome of internal fixation for pelvic ring fractures. J Trauma 1999;47:365-71. [Google Scholar | PubMed]
- 16.Lefaivre KA, Slobogean GP, Valeriote J, O’Brien PJ, Macadam SA. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: A systematic review. J Bone Joint Surg Br 2012;94:549-55. [Google Scholar | PubMed]
- 17.Lumsdaine W, Weber DG, Balogh ZJ. Pelvic fracture-specific scales versus general patient reported scales for pelvic fracture outcomes: A systematic review. ANZ J Surg 2016;86:687-90. [Google Scholar | PubMed]
- 18.Banierink H, Ten Duis K, Wendt K, Heineman E, IJpma F, Reininga I. Patient-reported physical functioning and quality of life after pelvic ring injury: A systematic review of the literature. PLoS One 2020;15:e0233226. [Google Scholar | PubMed]