Intra-articular osteoid osteoma of the femoral neck poses significant diagnostic challenges due to its atypical presentation and radiologic overlap with conditions such as avascular necrosis. This case underscores the limitations of MRI as a standalone modality in early detection, particularly in anatomically complex regions. Clinicians should maintain a high index of suspicion in young adults with persistent, unexplained hip pain and utilize sequential imaging strategies – especially CT – to identify the nidus. Timely diagnosis enables effective minimally invasive management with radiofrequency ablation, thereby reducing morbidity and improving clinical outcomes.
Dr. Sahil Chowdhary, Department of Orthopaedics, Dr. D.Y. Patil Medical College Hospital and Research Institute, Pune, Maharashtra, India. E-mail: 22020366@dpu.edu.in
Introduction: Osteoid osteoma is a benign bone tumor, accounting for 10–12% of benign bone lesions, most commonly affecting young adults aged 10–35 years. While typically presenting with night pain relieved by non-steroidal anti-inflammatory drugs, atypical locations like the femoral neck can mimic other conditions, such as avascular necrosis (AVN), complicating diagnosis. This case highlights the diagnostic challenge posed by overlapping symptoms and underscores the importance of advanced imaging for accurate diagnosis and timely management.
Case Report: We present a case of a 21-year-old male who initially presented with persistent right hip pain. Initial magnetic resonance imaging revealed marrow edema in the right femoral neck with associated joint effusion, leading to a preliminary diagnosis of stress fracture and subsequent misdiagnosis of AVN. The patient’s symptoms persisted despite conservative management. After 6 months of continued symptoms, computed tomography (CT) imaging revealed a characteristic lucent lesion in the inferior cortex of the right femoral neck, confirming the diagnosis of osteoid osteoma. The patient underwent successful radiofrequency ablation (RFA) performed in three cycles.
Conclusion: This case emphasizes the potential for osteoid osteoma to masquerade as AVN, particularly in young adults with hip pain. It demonstrates the superiority of CT imaging in detecting the characteristic nidus of osteoid osteoma and highlights the effectiveness of RFA as a definitive treatment modality.
Keywords: Osteoma, osteoid/diagnosis, femoral neck, osteonecrosis/diagnosis, magnetic resonance imaging.
Osteoid osteoma, a benign bone-forming tumor first described by Jaffe in 1935, accounts for approximately 10–12% of benign bone tumors and typically affects young adults between 10 and 35 years of age [1]. While these lesions can occur in any bone, they show a predilection for the lower extremities, with 50% of cases occurring in the femur and tibia [2]. The classic clinical presentation includes night pain that responds dramatically to non-steroidal anti-inflammatory drugs, particularly salicylates [3]. However, when these tumors occur in unusual locations such as the femoral neck, their presentation can mimic other pathologies, leading to diagnostic challenges and potential delays in appropriate treatment [4]. Avascular necrosis (AVN) of the femoral head is another significant cause of hip pain in young adults, often associated with various risk factors including corticosteroid use, alcohol abuse, trauma, and certain medical conditions [5]. The similar age group affected and overlapping symptomatology can create diagnostic confusion, particularly when classical imaging findings are subtle or atypical [6]. This case report presents a diagnostically challenging scenario of a young adult initially misdiagnosed with AVN, whose persistent symptoms and careful radiological review led to the correct diagnosis of osteoid osteoma. It emphasizes the importance of maintaining a broad differential diagnosis in young patients with hip pain and highlights the role of advanced imaging techniques in achieving diagnostic accuracy [7].
A 21-year-old male presented with persistent right hip pain that significantly impacted his daily activities. The patient’s initial symptoms began in May 2024, prompting medical evaluation including magnetic resonance imaging (MRI) of the hip. The initial MRI revealed marrow edema in the right femoral neck with associated hip joint effusion and periarticular soft tissue changes. While no definitive signs of AVN were observed, the presence of a stress fracture in the right femoral neck led to the administration of zoledronic acid. Concurrent lumbar spine imaging revealed multiple levels of degenerative changes, including a mild foraminal disc bulge at L3-L4, significant changes at L4-L5 with bilateral nerve compression, and disc protrusion at L5-S1. These findings complicated the clinical picture, potentially contributing to the diagnostic challenge. The patient’s condition progressed, and by July 2024, he experienced worsening hip pain with reduced range of motion. Based on the clinical presentation and previous imaging findings, he was diagnosed with AVN and a femoral stress fracture, leading to a conservative treatment approach with analgesics for 10 days. In October 2024, the presence of a vascular valley was noted, and the patient was advised on lifestyle modifications and dietary changes. Due to persistent symptoms, a repeat MRI was performed in November 2024, which showed mild-to-moderate right hip joint effusion with synovial thickening and subtle marrow edema in the right femoral head, neck, and acetabular roof. Notably, this study did not demonstrate definitive AVN changes, prompting further diagnostic investigation. By December 2024, the patient reported progressive pain radiating from the hip to the right thigh. A computed tomography (CT) scan revealed a critical finding: A characteristic lucent lesion in the inferior cortex of the right femoral neck, consistent with an osteoid osteoma. This discovery led to a definitive change in diagnosis and treatment approach. The patient underwent radiofrequency ablation (RFA) of the osteoid osteoma, performed in three cycles. This case highlights the diagnostic challenges in differentiating between osteoid osteoma and AVN, particularly in young patients presenting with hip pain. The evolution of imaging findings and the importance of maintaining a broad differential diagnosis were crucial in reaching the correct diagnosis. The case also demonstrates the value of advanced imaging techniques, particularly CT scanning, in identifying subtle bone lesions that may be missed on initial MRI studies (Fig. 1-3).

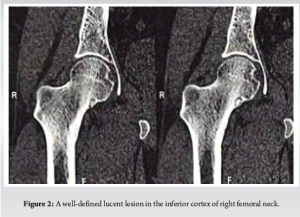
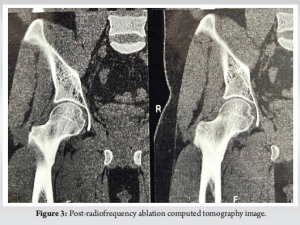
The presented case illustrates the diagnostic complexity of osteoid osteoma in the femoral neck, particularly when initial imaging and symptoms mimic AVN. Our patient’s presentation aligns with typical demographic characteristics of osteoid osteoma, which predominantly affects young adults in their second and third decades of life, with a male predilection reported in various studies [8]. The diagnostic challenge in our case stemmed from several factors that parallel findings in the existing literature. Chai et al. reported that intra-articular osteoid osteomas, particularly those in the hip joint, often present with atypical clinical features that can mask the classical presentation [7]. Similar to our case, Szendroi et al. documented that intra-articular lesions frequently present with synovitis and joint effusion, which can lead to misdiagnosis as inflammatory or degenerative conditions [4]. The initial misdiagnosis as AVN in our case is not unprecedented. Scalici et al. described similar cases where the presence of bone marrow edema on MRI led to incorrect initial diagnoses [9]. This underscores the limitations of MRI as a sole diagnostic tool for osteoid osteoma, despite its superior soft tissue resolution. Our experience reinforces the findings of Allen and Saifuddin, who emphasized that CT remains the gold standard for detecting the characteristic nidus of osteoid osteoma, particularly in complex anatomical locations [10]. The concurrent presence of lumbar spine pathology in our patient added another layer of diagnostic complexity. This finding correlates with studies by Lesher et al., who noted that referred pain patterns and coexisting pathologies can confound the clinical picture in hip disorders [11]. The radiation of pain to the thigh in our patient is consistent with the findings of Raux et al., who reported that up to 40% of patients with femoral neck osteoid osteomas experience referred pain patterns [12]. Our treatment approach using RFA aligns with the current best practices. Numerous studies have demonstrated the efficacy of RFA for osteoid osteoma, with success rates exceeding 90% [13]. The three-cycle approach used in our case is supported by research from Rosenthal et al., who demonstrated improved outcomes with multiple ablation cycles for lesions in weight-bearing locations [14]. The delay in diagnosis in our case, from initial presentation to definitive treatment, mirrors the findings of a multicenter study by Wenger et al., who reported an average delay of 15 months in cases of intra-articular osteoid osteoma [15]. This highlights the importance of maintaining a high index of suspicion for osteoid osteoma in young patients with persistent hip pain, even when initial imaging suggests alternative diagnoses. The case also emphasizes the value of sequential imaging in challenging cases. The progression from initial MRI to diagnostic CT aligns with the imaging algorithm proposed by Iyer et al., who advocate for multi-modality imaging in cases where clinical suspicion remains high despite initial negative findings [16].
This case highlights the diagnostic challenges of femoral neck osteoid osteoma, particularly when symptoms and initial imaging findings mimic AVN or other hip pathologies. The delay in diagnosis underscores the limitations of relying solely on MRI, emphasizing the critical role of CT in detecting the nidus. Persistent symptoms despite negative initial imaging warrant a high index of suspicion and sequential imaging. RFA remains an effective, minimally invasive treatment with excellent outcomes, reinforcing the importance of timely and accurate diagnosis for optimal patient care.
Osteoid osteoma in the femoral neck can mimic conditions like AVN, leading to diagnostic delays. Persistent hip pain in young adults warrants a thorough evaluation with sequential imaging, including CT, to identify the nidus. Early diagnosis and treatment with RFA offer excellent outcomes and prevent prolonged morbidity.
References
- 1.Jaffe HL. Osteoid-osteoma: A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935;31:709-28. [Google Scholar | PubMed]
- 2.Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H. Osteoid osteoma and osteoblastoma. J Am Acad Orthop Surg 2011;19:678-89. [Google Scholar | PubMed]
- 3.Mungo DV, Zhang X, O’Keefe RJ, Rosier RN, Puzas JE, Schwarz EM. COX-1 and COX-2 expression in osteoid osteomas. J Orthop Res 2002;20:159-62. [Google Scholar | PubMed]
- 4.Szendroi M, Köllo K, Antal I, Lakatos J, Szoke G. Intraarticular osteoid osteoma: Clinical features, imaging results, and comparison with extraarticular localization. J Rheumatol 2004;31:957-64. [Google Scholar | PubMed]
- 5.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1995;77:459-74. [Google Scholar | PubMed]
- 6.Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum 2002;32:94-124. [Google Scholar | PubMed]
- 7.Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA, et al. Radiologic diagnosis of osteoid osteoma: From simple to challenging findings. Radiographics 2010;30:737-49. [Google Scholar | PubMed]
- 8.Ghanem I. The management of osteoid osteoma: Updates and controversies. Curr Opin Pediatr 2006;18:36-41. [Google Scholar | PubMed]
- 9.Scalici J, Jacquel A, Mukish P, Trouilloud P, Baulot E. Intra-articular osteoid osteoma of the hip misdiagnosed by MRI: An unusual cause of unexplained hip pain. Orthop Traumatol Surg Res 2011;97:881-5. [Google Scholar | PubMed]
- 10.Allen SD, Saifuddin A. Imaging of intra-articular osteoid osteoma. Clin Radiol 2003;58:845-52. [Google Scholar | PubMed]
- 11.Lesher JM, Dreyfuss P, Hager N, Kaplan M, Furman M. Hip joint pain referral patterns: A descriptive study. Pain Med 2008;9:22-5. [Google Scholar | PubMed]
- 12.Raux S, Abelin-Genevois K, Canterino I, Chotel F, Kohler R. Osteoid osteoma of the proximal femur: Treatment by percutaneous bone resection and drilling (PBRD). A report of 44 cases. Orthop Traumatol Surg Res 2014;100:641-5. [Google Scholar | PubMed]
- 13.Vanderschueren GM, Taminiau AH, Obermann WR, Bloem JL. Osteoid osteoma: Clinical results with thermocoagulation. Radiology 2002;224:82-6. [Google Scholar | PubMed]
- 14.Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 1998;80:815-21. [Google Scholar | PubMed]
- 15.Wenger DE, Tibbo ME, Hadley ML, Sierra RJ, Welch TJ. Osteoid osteomas of the hip: A well-recognized entity with a proclivity for misdiagnosis. Eur Radiol 2023;33:8343-52. [Google Scholar | PubMed]
- 16.Iyer RS, Chapman T, Chew FS. Pediatric bone imaging: Diagnostic imaging of osteoid osteoma. Am J Roentgenol 2012;198:1039-52. [Google Scholar | PubMed]







