Complications due to microinstability, such as facet cyst formation, should be considered following Endoscopic Unilateral Laminotomy for Bilateral Decompression (Endo-ULBD).
Si Young Park, Department of Orthopedic Surgery, Yonsei University College of Medicine, 50-1, Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea. E-mail: drspine90@yuhs.ac; Drspine90@gmail.com
Introduction: Endoscopic unilateral laminectomy for bilateral decompression (Endo-ULBD) is a minimally invasive, motion-preserving surgical technique designed to decompress neural elements while preserving the posterior spinal structures. Because it maintains spinal integrity, the risk of postoperative instability is generally lower than that of conventional decompression techniques. However, microinstability-related complications, such as facet cyst formation, can still occur and may lead to recurrent symptoms.
Case Report: A 63-year-old male underwent ULBD for L4–5 lumbar stenosis and showed notable symptom improvement, which enabled his discharge without complications. However, on postoperative day 5, he developed low back pain and right-sided radiating leg pain. At the 3-month follow-up, these symptoms persisted, prompting an MRI, which revealed a right-sided facet cyst formation. Conservative management, including analgesics, was initiated. By the 4-month follow-up, the patient reported significant symptom improvement.
Conclusion: This case highlights that despite the minimally invasive nature of Endo-ULBD and its intent to reduce instability, complications related to microinstability, such as facet cyst formation, can still occur. Awareness of such potential complications is crucial for early diagnosis and management.
Keywords: Endoscopic ULBD complications, microinstability, postoperative facet cyst, postoperative complication.
Endoscopic unilateral laminectomy for bilateral decompression (Endo-ULBD) has gained widespread acceptance as a minimally invasive option for lumbar spinal stenosis (LSS). This technique preserves key posterior elements – including the facet joints – aiming to maintain the native motion and overall stability of the lumbar spine while effectively decompressing neural structures [1,2]. Due to these advantages, Endo-ULBD is associated with less muscle disruption, reduced postoperative pain, and shorter hospital stays compared to conventional bilateral laminectomy [3]. However, even with the motion-preserving intent of Endo-ULBD, recent studies have shown that limited bony resection can alter the biomechanics of the operated segment [4]. Kim et al. reported that dynamic radiographic evaluations revealed increased segmental motion in a subset of patients following percutaneous endoscopic cervical decompression, suggesting that the preservation of gross anatomy does not entirely prevent local stability changes [5]. Although no reports have definitively documented obvious instability following endoscopic lumbar decompression, it is important to consider that even minimal resection of the lamina and ligamentum flavum (LF) may disturb the delicate balance of forces in the lumbar spine. Facet joint cysts are thought to develop as a consequence of such microinstability. Increased mechanical stress on the facet joint – resulting from subtle postoperative hypermobility – can induce synovial hyperplasia and degeneration of the joint capsule, eventually leading to cyst formation [6,7]. In this report, we present a rare case of a contralateral facet cyst that developed shortly after Endo-ULBD for LSS, underscoring the need for meticulous surgical planning and careful postoperative monitoring even when employing minimally invasive, motion-preserving techniques.
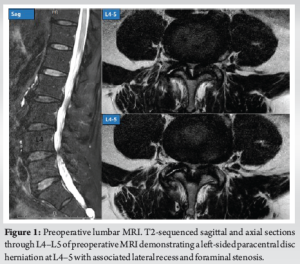
A 63-year-old male with a 1-year history of left-sided radiculopathy presented with bilateral neurogenic claudication and localized pain in the upper buttocks, radiating to the posterolateral thighs. His symptoms significantly limited his walking tolerance to 20 min. Prior conservative treatments, including lumbar epidural steroid injections, facet joint ablations, oral NSAIDs, and physical therapy, provided only temporary relief. On physical examination, the patient exhibited full motor strength (Grade 5 in all muscle groups), normal muscle tone, and preserved deep tendon reflexes. Sensory function was intact bilaterally, and the straight leg raise test was negative. Plain and dynamic radiographs showed no evidence of instability or other significant abnormalities. However, MRI revealed a left-sided paracentral disc herniation at L4–5 with associated lateral recess and foraminal stenosis (Fig. 1).
The patient underwent endoscopic unilateral laminotomy for bilateral decompression (ULBD) at L4–5 with minimal facet joint disruption. Our standard surgical approach involves removing the LF up to the tip of the superior articular process, ensuring adequate decompression of both traversing nerve roots. The procedure was uneventful, with no intraoperative complications, including nerve root injury. Postoperatively, the patient’s symptoms initially resolved. However, on postoperative day 5, the patient developed new-onset contralateral radiculopathy. As symptoms persisted, a follow-up MRI at 3 months postoperatively revealed a synovial cyst at the right L4/5 facet joint (Fig. 2). After discussing treatment options with the patient, pain management with NSAIDs and gabapentin was initiated. By the 6-month follow-up, the patient reported significant symptom improvement. As the symptoms had resolved, no further imaging studies, such as MRI, were performed.
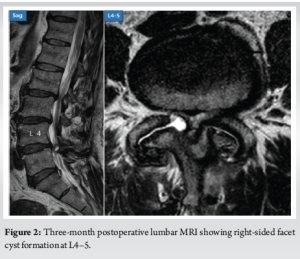
The present case involves a 63-year-old male who initially experienced significant symptom relief following endoscopic unilateral laminotomy for bilateral decompression (ULBD) at L4–5, only to develop new-onset contralateral radiculopathy on postoperative day 5. Subsequent imaging at 3 months revealed a synovial facet cyst at the right L4–5 facet joint. This case is noteworthy because it highlights that even minimally invasive, motion-preserving decompression techniques – designed to limit facet joint disruption – may still be associated with complications such as facet cyst formation, underscoring the need for vigilance during postoperative follow-up. Spinal synovial cysts have been associated with various etiologies, including inflammatory processes, congenital anomalies, myxoid degeneration of collagen, incomplete synovial tissue development, mesenchymal cell metaplasia, and fibroblast proliferation with excessive hyaluronic acid production [6-9]. Among these, degeneration and segmental instability are considered key factors, particularly given that synovial cysts most commonly develop at the L4–5 level, the most mobile segment of the lumbar spine [10,11]. Postoperative intraspinal facet cysts are relatively rare, with an incidence of approximately 5% [12]. These cysts have been associated not only with pre-existing segmental instability but also with postoperative progressive spondylolisthesis and accelerated disc degeneration [13]. During decompression, LF resection weakens the medial facet joint, potentially facilitating the protrusion of the joint capsule into the spinal canal. Moreover, since the LF plays a crucial role in maintaining intrinsic spinal stability and regulating intervertebral motion, its removal can contribute to postoperative biomechanical alterations [14]. Many studies argue that endoscopic decompression induces less instability compared to open decompression [15-17]; however, the fundamental decompression process of both procedures is similar. As a result, decompression itself, regardless of whether performed through an open or endoscopic approach, can influence facet cyst formation, including facet capsule protrusion, due to its impact on spinal biomechanics. In the present case, the minimal resection of the facet joint during ULBD may have predisposed the contralateral facet to abnormal loading, ultimately resulting in synovial cyst formation. This mechanism underscores that even motion-preserving techniques are not entirely immune to the adverse effects of altered postoperative biomechanics. To the best of our knowledge, this study is the only reported case demonstrating that microinstability can occur in the short term following endoscopic decompression surgery. Endoscopic spine surgery requires a relatively long learning period [18]. However, in this case, a postoperative facet cyst, which suggests instability, developed even though the surgery was performed by a highly experienced surgeon. This highlights the importance of being cautious about postoperative microinstability, even when using endoscopic decompression techniques. From a clinical management standpoint, this case emphasizes the importance of careful surgical planning. Various instruments for decompression, including a shaver, arthroscopic burr, or Kerrison punch, can be used to remove the LF attached to the lamina and facet joint. Surgeons should be thoroughly skilled in operating each instrument to perform the procedure without causing damage to the facet joint, particularly the superior articular process [19]. In this case, the patient’s symptoms were managed conservatively, with significant improvement observed at the 6-month follow-up. However, early recognition of microinstability-related complications remains critical for achieving optimal outcomes. Generally, idiopathic facet cysts are often treated with cyst excision, with or without adjunctive stabilization, depending on the degree of instability [20]. Surgeons should always be familiar with these management options to ensure appropriate intervention when necessary [21]. Future research should focus on identifying patient-specific risk factors and refining surgical techniques to further mitigate the risk of such complications. In the meantime, spine surgeons must remain aware that even minimally invasive procedures can lead to unforeseen biomechanical alterations, emphasizing the need for a balanced approach between adequate decompression and the preservation of spinal stability.
This case report demonstrates that even minimally invasive, motion-preserving techniques such as endoscopic unilateral laminotomy for bilateral decompression (ULBD) are not entirely exempt from postoperative biomechanical alterations. Despite the intent to preserve spinal stability, subtle microinstability may develop and contribute to rare complications like facet cyst formation. Early detection through vigilant postoperative monitoring is critical, as timely conservative management can lead to favorable outcomes.
While Endo-ULBD is a minimally invasive technique designed to preserve spinal stability, this case highlights that postoperative microinstability can still occur, leading to complications such as contralateral facet cyst formation. To minimize this risk, a comprehensive preoperative evaluation of the facet joint, including its morphology, degenerative changes, and potential instability, is crucial for optimizing surgical planning. Intraoperatively, meticulous bone work should be performed with minimal facet joint disruption to preserve stability and reduce the likelihood of postoperative microinstability. Surgeons should remain vigilant for delayed-onset symptoms and consider postoperative instability as a potential cause, emphasizing the need for careful surgical planning and thorough follow-up.
References
- 1.Spetzger U, Bertalanffy H, Reinges MH, Gilsbach JM. Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis. Part II: Clinical experiences. Acta Neurochir (Wien) 1997;139:397-403. [Google Scholar | PubMed]
- 2.Kim HS, Choi SH, Shim DM, Lee IS, Oh YK, Woo YH. Advantages of new endoscopic unilateral laminectomy for bilateral decompression (ULBD) over conventional microscopic ULBD. Clin Orthop Surg 2020;12:330-6. [Google Scholar | PubMed]
- 3.Park SM, Kim GU, Kim HJ, Choi JH, Chang BS, Lee CK, et al. Is the use of a unilateral biportal endoscopic approach associated with rapid recovery after lumbar decompressive laminectomy? A preliminary analysis of a prospective randomized controlled trial. World Neurosurg 2019;128:e709-18. [Google Scholar | PubMed]
- 4.Ju CI, Lee SM. Complications and management of endoscopic spinal surgery. Neurospine 2023;20:56-77. [Google Scholar | PubMed]
- 5.Quillo-Olvera J, Lin GX, Kim JS. Percutaneous endoscopic cervical discectomy: A technical review. Ann Transl Med 2018;6:100. [Google Scholar | PubMed]
- 6.Arantes M, Silva RS, Romão H, Resende M, Moniz P, Honavar M, et al. Spontaneous hemorrhage in a lumbar ganglion cyst. Spine (Phila Pa 1976) 2008;33:E521-4. [Google Scholar | PubMed]
- 7.Banning CS, Thorell WE, Leibrock LG. Patient outcome after resection of lumbar juxtafacet cysts. Spine (Phila Pa 1976) 2001;26:969-72. [Google Scholar | PubMed]
- 8.Chimento GF, Ricciardi JE, Whitecloud TS 3rd. Intraspinal extradural ganglion cyst. J Spinal Disord 1995;8:82-5. [Google Scholar | PubMed]
- 9.Eck JC, Triantafyllou SJ. Hemorrhagic lumbar synovial facet cyst secondary to anticoagulation therapy. Spine J 2005;5:451-3. [Google Scholar | PubMed]
- 10.Zhao J, Li C, Qin T, Jin Y, He R, Sun Y, et al. Mechanical overloading-induced miR-325-3p reduction promoted chondrocyte senescence and exacerbated facet joint degeneration. Arthritis Res Ther 2023;25:54. [Google Scholar | PubMed]
- 11.Rong X, Liu Z, Wang B, Pan X, Liu H. Relationship between facet tropism and facet joint degeneration in the sub-axial cervical spine. BMC Musculoskelet Disord 2017;18:86. [Google Scholar | PubMed]
- 12.Morishita Y, Taniguchi R, Kawano O, Maeda T. Synovial facet joint cysts after lumbar posterior decompression surgery. J Neurosurg Spine 2021;35:704-9. [Google Scholar | PubMed]
- 13.Ikuta K, Tono O, Oga M. Prevalence and clinical features of intraspinal facet cysts after decompression surgery for lumbar spinal stenosis. J Neurosurg Spine 2009;10:617-22. [Google Scholar | PubMed]
- 14.Safak AA, Is M, Sevinc O, Barut C, Eryoruk N, Erdogmus B, et al. The thickness of the ligamentum flavum in relation to age and gender. Clin Anat 2010;23:79-83. [Google Scholar | PubMed]
- 15.Choi SS, Ahn G, Jang IT, Kim HS. Clinical and radiological outcomes of full-endoscopic decompression for lumbar spinal stenosis with grade i degenerative spondylolisthesis: A retrospective study with a minimum 1-year follow-up. Neurosurg Pract 2024;5:e00078. [Google Scholar | PubMed]
- 16.Persaud-Sharma D, Gunaratne C, Talati J, Philips W, Sohel A, Blake A, et al. Efficacy of endoscopic decompression surgery for treatment of lumbar spinal stenosis. Interv Pain Med 2024;3:100391. [Google Scholar | PubMed]
- 17.Yagi K, Kishima K, Tezuka F, Morimoto M, Yamashita K, Takata Y, et al. Advantages of revision transforaminal full-endoscopic spine surgery in patients who have previously undergone posterior spine surgery. J Neurol Surg A Cent Eur Neurosurg 2023;84:528-35. [Google Scholar | PubMed]
- 18.Maayan O, Mai E, Kim AY, Iyer S. Overview of endoscopic spine surgery and learning curve. Semin Spine Surg 2024;36:101079. [Google Scholar | PubMed]
- 19.Min WK, Kim JE, Choi DJ, Park EJ, Heo J. Clinical and radiological outcomes between biportal endoscopic decompression and microscopic decompression in lumbar spinal stenosis. J Orthop Sci 2020;25:371-8. [Google Scholar | PubMed]
- 20.Métellus P, Fuentes S, Adetchessi T, Levrier O, Flores-Parra I, Talianu D, et al. Retrospective study of 77 patients harbouring lumbar synovial cysts: Functional and neurological outcome. Acta Neurochir (Wien) 2006;148:47-54. [Google Scholar | PubMed]
- 21.Piscoya AS, Clark DM, Wagner SC. Management of postoperative facet cysts: A report of 3 cases. JBJS Case Connect 2020 Jul-Sep;10(3):e20.00134. [Google Scholar | PubMed]