It is recommended to acquire the maximum amount of positive support reduction during fixation for unstable pertrochanteric fractures because it improves mechanical stability.
Dr. Makesh Ram Sriraghavan, Department Of orthopedics, Periyar Government Hospital , Madras Medical College, Chennai, Tamilnadu, India. Email: ram23ortho@yahoo.com
Introduction: Pertrochanteric fractures are among the most common hip fractures in the elderly population, typically resulting from low-energy trauma such as a simple fall. This demographic is particularly susceptible due to factors like decreased bone density, frailty, and impaired balance. It can occur in the younger patient due to high-velocity trauma – road traffic accidents. Medial cortical support (MCS) reduction is a key element, as it allows limited sliding of head–neck fragments and it provides good fracture healing and MCS acts as non-anatomic buttress reduction providing secondary stability.
Materials and Methods: This is a prospective single study center cohort which includes 40 patients undergoing treatment for an unstable pertrochanteric fracture using Proximal Femoral Nail A2 (PFN A2) admitted in the Department of Orthopedics, Government Thoothukudi Medical College Hospital, Tamil Nadu from June 2019 to September 2024, for a follow-up period for a maximum of 18–24 months.
Results: In our study, outcome analysis was assessed by Harris hip scoring system 56% which showed excellent results, 24% good, 12% shows fair, and other 8% bad outcome. In this series, 21 cases were fixed in positive cortical support, 15 cases in neutral support, and 4 cases in negative cortical support. We noticed varus malunion in 2 cases and 1 case of delayed union and 1 case of screw pullout in the negative cortical support group.
Conclusion: Positive and neutral medial cortical support was noticed to produce a stronger buttress effect in both the anteroposterior and lateral views. It is recommended to acquire the maximum amount of positive support reduction during a procedure for unstable pertrochanteric fractures because it improves mechanical stability.
Keywords: Medial cortical support, trochanteric fracture, proximal femoral nail A2.
Elderly people are most likely to suffer from pertrochanteric fractures. There are various forms of internal fixation implants for trochanteric fractures, of them the most commonly used implant is the Dynamic Hip Screw (DHS) [1-4]. This is a collapsible fixation implant, which permits the proximal fragment to collapse or settle on the fixation implant [5]. Nowadays, the most commonly used implant for the management of trochanteric fracture is the proximal femoral nail (PFN), which is a collapsible device and with added rotational stability [6]. This implant is a centro medullary device and biomechanically sounder with other added advantages like small incision, minimal blood loss, and good stability. The key factor for stability in pertrochanteric fracture is the Medial Cortical Support (MCS) of the femoral neck [7]. MCS allows limited, controlled impaction (sliding) of the proximal fragment along the implant axis, facilitating stable fracture healing. They were classified into three groups according to the grade of medial cortical support in fracture reduction (positive, neutral, negative). The positive cortex support was defined that the medial cortex of the head-neck fragment displaced and located a little bit superomedial to the medial cortex of the shaft. If the neck cortex is located laterally to the shaft, it is negative with no cortical buttress, and if the two cortices contact smoothly, it is in a neutral position [8]. The demographic baseline, postoperative radiographic femoral neck-shaft angle and neck length, rehabilitation progress [9], and functional recovery scores of each group were recorded and compared.
This is a prospective study conducted in Orthopaedics Department, Thoothukudi Medical College Hospital, Tamil Nadu from June 2019 to September 2024. We included 40 patients of both sexes with isolated trochanteric fractures in the age group of 20–65 years of Boyd and Griffin type 2,3,4. Cases of those not willing to study, polytrauma and head injury patients, preexisting arthritis of the hip joint, pathological trochanteric fractures, non-union trochanteric fractures, and those whose lost follow-up were excluded from this study. All standard protocols and norms were followed. A thorough clinical history and clinical examination were done, patient subjected to routine blood investigations and radiological evaluation (AP and Lateral). All patients were primarily immobilized with skin traction.
Determination of nail diameter
To find the appropriate nail diameter, an AP and lateral X-ray was used to measure the femur diameter at the isthmus level [9,10].
Determination of neck shaft angle
A goniometer was used on the patient unaffected side by the AP X-ray to assess the neck shaft angle [11].
Surgical procedure
Under strict aseptic precaution, under anesthesia, the patient in the supine position, fracture limb in the traction table, opposite limb in the lithotomy position, and parts are painted and draped. Under C arm guidance fracture reduced, if found unreduced, fracture reduced with percutaneous/open reduction and temporarily fixed with K wires (which will not interrupt the nail insertion and helical blade insertion). Skin incision made, facia and muscle cut, entry made guide wire insert, reaming done. PFNA2 nail inserted and helical blade inserted and then distal locking done. The wound closed; dressing is done.
Post op protocol
Following surgery, vital signs such as breathing rate, temperature, blood pressure, and pulse were closely monitored and antibiotic treatment continued. As needed, patients were prescribed analgesics. Depending on the need, blood transfusions were administered. Twelve days after surgery, sutures were removed. Patients were advised to sit in bed for at least the first 24 h after surgery. During the first postoperative day, patients learned how to mobilize their knees as pain tolerated and set their quadriceps. Nonweight-bearing walking with a walker was allowed from 2nd postoperative day. Along with hip and knee mobilization, the patient was discharged 5–7 days after surgery based on associated medical comorbidities. Partial weight bearing is allowed 3–6 weeks after surgery based on medial cortical support. We started delayed weight bearing in fractures which showed negative cortical support. Strictly full weight bearing started only after radiological and clinical evidence of union.
Follow-up
Every patient was periodically evaluated every 4 weeks until the fracture healed, and then every three months until a year late, and then subsequently every 6 months up to a maximum of 2 years. In every visit, we included a clinical evaluation of their hip and knee mobility, gait, fracture healing, deformity, and shortening. We evaluated the patient by using a modified version of the Harris hip scoring system. For the purpose of evaluating fracture union and implant-bone contact, an X-ray of the affected hip with femur was performed on every follow-up.
Demography data
In our series, the age distribution was from 20 to 65 years and the most common age group was between 61 and 65 years. The mean age group is 59 years. Males were common in our study (25 cases) compared to females (15 cases). Left-sided injury was more common (24 cases).
Mode of injury
In our study, self-fall was more common (Table 1), mode of injury than RTA.

Boyd and Griffin classification
In our study, Boyd and Griffin type 3, cases were most commonly reported (56%) and type 4 was least commonly reported (Table 2).
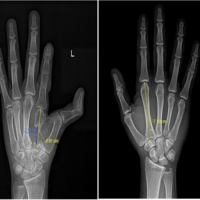
Anteromedial cortical support reduction- Radiological evaluation
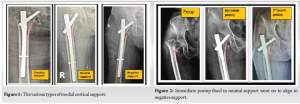
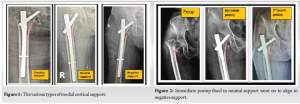
In the immediate post-operative period, radiological evaluation was done based on anteromedial cortical support (AMCS). We noticed that the majority of cases (21 cases) had positive support. We also observed neutral support in 15 cases and negative support in 4 cases (Table 3 and Fig. 1).

Relationship between Boyd and Griffin trochanteric fracture type and Anteromedial cortical support
We analyzed the AMCS with the type of fracture sustained, it was noticed that positive support was most common in type 2 (Table 4).

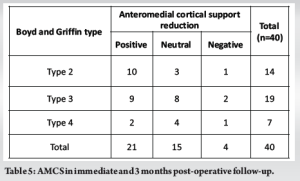
Radiological analysis at immediate and post-operative for anteromedial cortical support
In our study, out of 21 cases of positive cortical support – 6 cases went to neutral support, those were 3 cases from Boyd and Griffin type 2, two cases from type 3 and 1 case from type 4, and other each 1cases from type 2 and type 3 went to negative cortical support from neutral cortical support and 3 cases from type 4 went to negative cortical support from neutral reduction. Finally, all the fractures united well between 3 and 5 months (Table 5 and Fig. 2 and 3).

Complication
There was screw pullout (Fig. 4) in one case fixed with neutral cortical support, and subsequently treated with revision PFN A2 with bone grafting (Table 6). We noticed varus malunion in 2 cases (Fig. 5) and 1 case of delayed union (united in 16 weeks). These observed complications were reported in the negative cortical support group. We also noticed a superficial infection in 2 cases which settled with antibiotics.



Functional outcome of intertrochanteric fractures
Results from our research of 40 patients using the Modified Harris Hip Scoring System ranged from excellent (56%), good (24%), fair (12%), to poor (8%). All positive and neutral reduction cases showed excellent and good results (Table 7).

Before the advised placement of various implants, the anatomic reduction is always performed during the procedure of unstable pertrochanteric fractures. Posteromedial cortical alignment is critical for effective reduction in any type of implant used. It should be ensured that the femoral head–neck and shaft fragments are in anteromedial contact and that the Garden alignments are met for these fractures [12]. Fracture alignment in the valgus position does not always indicate favorable medial cortical support when fragments are displaced. Bone healing is aided by compressing the bone fragments [13]. One way to fix unstable pertrochanteric fractures is to compress the fracture site during surgery. Postoperative bone impaction using a helical blade or lag screw that is controlled along its axis is another best available option. During surgery, the surgeon applies pressure to the fracture site to stabilize the main fracture. A combination of the patient’s weight bearing, muscle contraction, and a fixation device that can slide is required to attain secondary fracture stability [14]. When the head-neck fragment is controlled and impacted via constrained sliding onto the femur shaft, it provides secondary axial and torsional stability [15], due to controlled collapse which occurs in with subsequent dynamic processes, including remodeling along the fracture line and cyclic loading. For displaced sub-capital femoral neck fractures, Gotfried initially suggested reducing the non-anatomic positive cortical buttress. Thanks to a 180° fracture alignment in the lateral view, the displaced sub-capital femoral fragment may be seen medially to the lower-medial border of the proximal fracture fragment in the Anterior-Posterior (AP) imaging [16]. At this stage, the distal component might stop the femoral head from sliding too far through the buttress that joins the cortex to the remainder of the bone. A new definition of positive medial cortical support is proposed for unstable pertrochanteric fractures. It deviates from Gotfried’s standard in the AP view by moving the distal femoral shaft fragment somewhat laterally to the lower-medial border of the proximal fracture fragment, and it also necessitates a 180° fracture alignment in the lateral view. After surgery for a pertrochanteric fracture, the piece of the head and neck often shifts laterally as sliding starts. Unlike in unstable femoral neck fractures, where the proximal fragment typically moves in a displacement pattern, this one hits the comminuted and low-intensity trochanteric zone, leading to collapse [16]. There may be three possible sub-conditions for some of the so-called “anatomic reduction” features observed in intraoperative fluoroscopy: a small positive position, a small negative position, and the same anatomic cortex-to-cortex position as others. Those sub-conditions were difficult to detect, however, due to the low picture resolution. Therefore, we substituted “neutral” for “anatomic reduction.” The medial cortex of the femoral shaft may stop the femoral head-neck fragment from sliding any farther laterally, and the two major portions touch each other’s cortex in the same way as the positive medial cortical support position. A further source of secondary stability is the contact between the anterior cortex and the head during head-neck sliding. Positive medial cortical support, on the other hand, maybe more successful than anterior cortical contact, considering the essential of lateral sliding direction. The optimal method for reducing pertrochanteric fragments also involves getting an anterior cortical buttress in addition to a medial buttress (anteromedial reduction). we looked at, of 21 cases of positive cortical support – 6 cases went to neutral support, those were 3 cases from Boyd and Griffin type 2, 2 cases from type 3 and 1 case from type 4 and other each 1cases from type 2 and type 3 went to negative cortical support from neutral cortical support and 3 cases from type 4 went to negative cortical support from neutral reduction. All three groups were similar in terms of age, sex ratio, number of medical comorbidities, fracture reduction quality, osteoporosis Singh index [18], and placement of the helical blade in the femoral head except for walking ability. During follow-up, patients in the group that received positive medial cortical support for reduction were able to walk on the ground much sooner than those in the group that received negative support, and which had a significant decrease in the loss of neck shaft angle and neck length. Minor misalignment may progress to complete misalignment after bone resorption along the fracture plane. Two patients in our case series who initially had neutral cortical reduction eventually became negative, and their results were poor. All four of these patients likewise showed no evidence of anterior cortical support on the lateral radiographs. Later on, the nine patients who initially showed positive cortical reduction went into neutral reduction. According to our research, reducing medial cortical support using a cephalomedullary nail appears to be a simple process. The fact that tension on the leg may easily separate the two primary pieces might be because pertrochanteric fractures are a kind of extracapsular fractures. When the nail is introduced from the medial edge of the greater trochanter, a wedge may form between the femoral head-neck fragment and the lateral wall. It is possible to move the shaft laterally by pushing the lateral wall with the nail. This means the shaft piece is now lateral to the lower medial border of the proximal head-neck piece. In theory, the wedge-open effect and a favorable decrease in medial cortical support can lead to an increase in femoral offset, which is beneficial for abductor strength. When there is too much distraction and/or too many open cortices, the impaction area among fragments decreases, union is delayed, or non-union occurs. In our study of 40 patients, according to Harris Hip Scoring System 56% shows excellent results, 24% good results, 12% shows fair results and other 8% bad results such as infection, varus collapse, pain, and screw pullout. In our study, we observe early union and early weight bearing occurred in trochanteric fracture fixed with positive cortical support, the average union duration in type 2 trochanteric fracture average union is 8 weeks and type 3 and 4 show late union compare to others types. The mean hospital stay is 10 days and mean full weight bearing 9 weeks and there is no limb length discrepancy noted. Three had varus collapse, one underwent screw pullout and was subsequently treated with revision PFN A2 with bone grafting. Two patients were treated with intravenous antibiotics for superficial infections. [19,20]
Positive and neutral medial cortical support was observed to produce a stronger buttress effect in both the anteroposterior and lateral views. It is recommended to acquire the maximum amount of positive support reduction during a procedure for unstable pertrochanteric fractures because it improves mechanical stability. Fixation failure was common with the negative support reduction pattern; thus, surgeons should steer clear of it, if possible, preoperatively. When reducing a fracture, non-anatomic positive medial cortical support may help create an optimal mechanical setting for the healing process. Once the head–neck fragment reaches the femur shaft, secondary stability is achieved because this support prevents its sliding.
Irrespective of any age group, all intertrochanteric fractures requires acceptable optimal fixation and stable reduction. PFN A2 is the ideal implant in unstable trochanteric fractures. The helical blade design provides better rotational stability and anchorage with improved clinical outcomes.
References
- 1.Kristan A, Benulič C, Jaklič M. Reduction of trochanteric fractures in lateral view is significant predictor for radiological and functional result after six months. Injury 2021;52:3036-41. [Google Scholar | PubMed]
- 2.Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: Comparison of patient self-report with surgeon assessment. J Arthroplasty 2001;16:575-80. [Google Scholar | PubMed]
- 3.Xie W, Shi L, Zhang C, Cui X, Chen X, Xie T, et al. Anteromedial cortical support reduction of intertrochanteric fractures-a review. Injury 2024;55:111926. [Google Scholar | PubMed]
- 4.Jonnes C, Shishir SM, Najimudeen S. Type II intertrochanteric fractures: Proximal femoral nailing (PFN) versus dynamic hip screw (DHS). Arch Bone Jt Surg 2016;4:23-8. [Google Scholar | PubMed]
- 5.Bharadwaj S. Prospective Study of Management of Trochanteric Fractures Treated with Dynamic Hip Screw. [MS Thesis]. India: Rajiv Gandhi University of Health Sciences; 2014. [Google Scholar | PubMed]
- 6.Druva V. A Clinical Outcome of Surgical Management of Unstable Intertrochanteric Fractures by Proximal Femoral Nail Antirotation-II [Master’s Thesis]. India: Rajiv Gandhi University of Health Sciences; 2020. [Google Scholar | PubMed]
- 7.Mao W, Chang SM, Zhang YQ, Li Y, Du SC, Hu SJ, et al. Positive medial cortical support versus anatomical reduction for trochanteric hip fractures: Finite element analysis and biomechanical testing. Comput Methods Programs Biomed 2023;234:107502. [Google Scholar | PubMed]
- 8.Cho MR, Lee JH, Kwon JB, Do JS, Chae SB, Choi WK. The effect of positive medial cortical support in reduction of pertrochanteric fractures with posteromedial wall defect using a dynamic hip screw. Clin Orthop Surg 2018;10:292-8. [Google Scholar | PubMed]
- 9.Pajarinen J, Lindahl J, Savolainen V, Michelsson O, Hirvensalo E. Femoral shaft medialisation and neck-shaft angle in unstable pertrochanteric femoral fractures. Int Orthop 2004;28:347-53. [Google Scholar | PubMed]
- 10.Yang TC, Tzeng YH, Wang CS, Lin CC, Chang MC, Chiang CC. “Ratio of fracture site diameter to isthmus femoral canal diameter” as a predictor of complication following treatment of infra-isthmal femoral shaft fracture with antegrade intramedullary nailing. Injury 2021;52:961-6. [Google Scholar | PubMed]
- 11.Bizdikian AJ, Assi A, Bakouny Z, Saghbini E, Bakhos GE, Esber S, et al. Validity and reliability of different techniques of neck-shaft angle measurement. Clin Radiol 2018;73:984.e1-9. [Google Scholar | PubMed]
- 12.Hunter TB. Fracture fixation. Radiologic Guide to Orthopedic Devices. Cambridge: Cambridge University Press; 2017. p. 19. [Google Scholar | PubMed]
- 13.Thakur AJ. The Elements of Fracture Fixation-E-Book. Amsterdam: Elsevier Health Sciences; 2022. [Google Scholar | PubMed]
- 14.Taljanovic MS, Jones MD, Ruth JT, Benjamin JB, Sheppard JE, Hunter TB. Fracture fixation. Radiographics 2003;23:1569-90. [Google Scholar | PubMed]
- 15.Ajay SS. A Prospective Study of Surgical Management of Basicervical Fracture Neck of Femur Treated with Dynamic Hip Screw and Derotation Screw. [MS Thesis]. India: Rajiv Gandhi University of Health Sciences; 2020. [Google Scholar | PubMed]
- 16.Giannakou M. Rehabilitation Plan and Process in Patients after a Hip Fracture. Vol. 11. [Bachelor of Thesis]; 2016. p. 161. [Google Scholar | PubMed]
- 17.Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015;135:811-8. [Google Scholar | PubMed]
- 18.Koot VC, Kesselaer SM, Clevers GJ, De Hooge P, Weits T, Van der Werken C. Evaluation of the singh index for measuring osteoporosis. J Bone Joint Surg Br 1996;78:831-4. [Google Scholar | PubMed]
- 19.Li H, Chen H, She R, Li Y, Qin G, Gan F, et al. Clinical observation of Gofried positive buttress reduction in the treatment of trochanteric fracture: A systematic review and meta-analysis. Medicine (Baltimore) 2023;102:e36424. [Google Scholar | PubMed]
- 20.Zhang YQ, Chang SM. Mechanism of “Gotfried reduction” in femoral neck fracture. J Orthop Trauma 2013;27:e291. [Google Scholar | PubMed]