Understanding the biomechanical implications of meniscal root tears is essential for guiding timely and effective management.
Dr. Brajesh Dadarya, Department of Orthopaedics, NSCB, Jabalpur, Madhya Pradesh, India. E-mail: dr.bdadarya@gmail.com
Introduction: Meniscal root tears (MRTs) disrupt knee biomechanics, leading to meniscal extrusion, joint instability, and osteoarthritis progression. They are classified as degenerative or traumatic, with varying etiologies and clinical implications.
Objectives: The objectives were to evaluate the etiology, biomechanics, management strategies, and outcomes of MRTs, focusing on the effectiveness of surgical repair in preserving knee function and delaying osteoarthritis.
Materials and Method: A review of recent literature was conducted, analyzing key aspects of MRTs, including pathogenesis, biomechanical consequences, management approaches, and patient outcomes. Studies assessing surgical techniques, non-operative treatment, and partial meniscectomy were included in the study.
Result: Degenerative MRTs were common in older, obese individuals with varus alignment, whereas traumatic MRTs occurred in younger patients with concomitant injuries. Surgical repair demonstrated favorable short-term outcomes, including reduced extrusion and improved clinical scores, but challenges such as persistent extrusion and long-term cartilage damage persisted. Non-operative treatment and partial meniscectomy offered limited benefits, with higher risks of osteoarthritis progression.
Conclusion: MRTs significantly impact knee joint health, requiring timely diagnosis and individualized management. Surgical repair remains the gold standard, restoring knee kinematics and delaying osteoarthritis, although long-term outcomes need further optimization. Personalized treatment strategies based on patient-specific factors are essential for improved care.
Keywords: Meniscal root tears, surgical repair, osteoarthritis.
Medial meniscus posterior root tears (MMPRTs) are severe injuries that compromise knee biomechanical stability, resulting in a loss of hoop tension and accelerated joint degeneration, comparable to total meniscectomy. These injuries are increasingly recognized as significant contributors to early osteoarthritis and joint dysfunction. Arthroscopic repair, particularly utilizing transtibial pullout techniques, has emerged as the standard treatment to restore meniscal function and mitigate long-term complications, with studies demonstrating superior clinical and radiological outcomes compared to non-operative approaches or partial meniscectomy [1,2]. Posterior medial meniscus root tears are now widely acknowledged for their potential to induce progressive arthritis if left untreated [3]. Damage proximal to the root attachment significantly alters tibiofemoral contact mechanics, leading to the rapid progression of osteoarthritis [4]. By impairing hoop tension, MMPRTs compromise the meniscus’s capacity to transmit loads, simulating the biomechanical effects of a total meniscectomy [5]. Recent studies emphasize the efficacy of arthroscopic repair in maintaining meniscal integrity and reducing extrusion, which is crucial for proper load distribution in the joint [6]. Advancements such as suture anchor techniques offer enhanced fixation strength and less invasive procedures [7]. However, outcomes remain variable, underscoring the necessity for further research to compare techniques and identify factors influencing successful repairs [8]. The prevalence of posterior medial meniscus root tears has been reported to range from 10.1% to 21.4% in patients undergoing meniscal repair or meniscectomy and 3.6% of all meniscal tears [9]. This review examines the biomechanical basis, surgical methods, and outcomes of arthroscopic MMPRT repair, providing recommendations to enhance patient care and promote knee health.
Objectives
The objective of the study is to evaluate the outcomes of arthroscopic fixation in patients with MMPRT.
The study was conducted in a tertiary care setting, where patients presenting with symptomatic MMPRT were selected for surgical intervention. The diagnosis of MMPRT was confirmed through clinical suspicion followed by magnetic resonance imaging (MRI) [10]. Only patients with confirmed MMPRT on MRI and those who failed non-operative management were included in the study.
Patient selection
Patients aged 18–65 years with symptomatic MMPRTs confirmed by MRI were included. Inclusion criteria consisted of patients with minimal osteoarthritis (Outerbridge grade 0–2), no significant concomitant knee injuries, and failure of conservative treatment for at least 3 months. Exclusion criteria were patients with severe osteoarthritis (Outerbridge grade 3 or 4), prior knee surgeries, or contraindications to surgery [10].
Surgical technique
The procedure was performed under general or spinal anesthesia with the patient in a supine position. Standard arthroscopic portals were created to provide adequate visualization and access to the knee joint. Diagnostic arthroscopy was initially performed to assess the tear pattern and address any other knee pathologies, such as cartilage damage or associated ligament injuries. The MMPRT was confirmed through probing (Fig. 1), with the tear identified at the meniscus root attachment. Two relay sutures were passed using a suture-passing device (Fig. 2) to facilitate the repair of the root tear. A tunnel was drilled at the anatomical footprint of the posterior meniscus root, which was carefully identified during the arthroscopic procedure (Fig. 3) [11]. For fixation, the tunnel was made at the anatomical footprint, and the meniscus root was reattached using the fiber wire. Other concomitant meniscal tears were also addressed and fixed using appropriate fixation techniques. The final fixation was confirmed by probing (Fig. 4) to ensure that the root was securely attached to its anatomic footprint. The stability of the fixation was further validated through repeated probing (Fig. 5-7), confirming that the repair was stable and well-positioned [12].


Postoperative care and rehabilitation
Postoperative care involved a structured rehabilitation protocol. The patient was initially kept non-weight-bearing for the first 4 weeks. Partial weight-bearing was allowed after 4 weeks, and full weight-bearing was permitted after 8 weeks, depending on clinical and radiological evaluation. Range-of-motion exercises, strengthening, and proprioceptive training began at 4 weeks post-surgery.
Outcome measures
The primary outcomes included meniscal extrusion, which was measured using 3D MRI preoperatively and at 3 months post-surgery, and functional outcomes assessed through the knee injury and osteoarthritis outcome score (KOOS) and Visual Analog Scale (VAS) for pain. Secondary outcomes included complications such as infection, re-tear, and hardware failure, along with the ability to return to pre-injury activity levels.
Statistical analysis
Data were analyzed using Statistical Packages for the Social Sciences version 25. Descriptive statistics were applied, and paired t-tests or Wilcoxon signed-rank tests were used to compare preoperative and postoperative outcomes. A P < 0.05 was considered statistically significant.
Fifty patients with MMPRTs confirmed by MRI and clinical examination underwent arthroscopic fixation. The mean age was 46 ± 8 years, with 64% being male. All patients reported significant pre-operative knee pain, instability, and functional limitations. The average follow-up duration was 12 months.
Radiological findings
MRI findings revealed a mean pre-operative meniscal extrusion of 3.5 ± 0.8 mm, which significantly decreased to 1.2 ± 0.6 mm at 3 months postoperatively (P < 0.001). Postoperative imaging confirmed successful reattachment of the root at the anatomical footprint (Table 1).
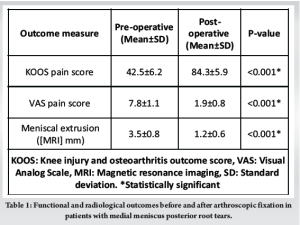
Functional outcomes
KOOS improved significantly in all subdomains, particularly for pain and daily activities. The mean KOOS pain score increased from 42.5 ± 6.2 preoperatively to 84.3 ± 5.9 at the final follow-up (P < 0.001). Pain, measured by the VAS, decreased from 7.8 ± 1.1 to 1.9 ± 0.8 postoperatively (P < 0.001) (Table 1).
Stability and return to activity
Intraoperative probing confirmed stable fixation in all cases. At 6 months, 90% of patients returned to their pre-injury activity levels, whereas 10% required extended rehabilitation. No cases of re-tears were observed during the follow-up period.
Complications
Minor complications occurred in 8% of patients, including transient knee effusion and superficial portal site infections in 4%, both of which were treated conservatively. There were no deep infections, hardware failures, or neurovascular injuries.
MMPRTs represent a significant pathology with profound biomechanical, clinical, and functional implications. Recent studies have extensively evaluated the anatomy, biomechanics, etiology, diagnosis, treatment, and rehabilitation associated with MMPRTs, yielding important insights into its management and outcomes. MMPRTs result in loss of hoop stress, creating a meniscal-deficient knee state that contributes to joint instability and accelerated cartilage degeneration. Moon et al. emphasized the detrimental biomechanical effects of untreated MMPRTs, particularly their association with increased meniscal extrusion and osteoarthritis progression [13]. Similarly, Takase et al. highlighted that while transtibial pullout repair reduces extrusion in flexion positions, it fails to sustain long-term extrusion reduction in extension positions, correlating with ongoing cartilage damage [14]. The etiology of MMPRTs varies significantly compared to lateral meniscus root tears (LMRTs). Karpinski et al. demonstrated that MMPRTs are predominantly degenerative, often linked with varus alignment, older age, and higher body mass index (BMI), whereas LMRTs are more commonly traumatic and associated with anterior cruciate ligament injuries [15]. Kodama et al. supported these findings, identifying dynamic medial meniscus extrusion during flexion as a key factor in cartilage degeneration among older patients with MMPRTs [16]. In contrast, Mundal et al. described a unique subgroup of traumatic MMPRTs in younger patients, often characterized by concomitant injuries, highlighting the heterogeneity in pathogenesis [17]. Management of meniscal root tears (MRTs) depends on injury severity, timing, and cartilage status. Non-operative treatment suits advanced cartilage damage or unfit patients, focusing on symptom relief. Surgical repair, the mainstay, restores knee kinematics but is contraindicated in severe osteoarthritis or malalignment. Partial meniscectomy offers short-term relief but risks long-term osteoarthritis progression [18]. Arthroscopic and transtibial pullout techniques are the primary surgical options for MMPRTs, aimed at restoring meniscal function and biomechanical integrity. Wu detailed an arthroscopic knotless suture anchor technique, emphasizing its ability to reduce extrusion and promote healing in patients without advanced arthritis [19]. However, Takase et al. observed that while surgical repair significantly improves clinical scores, such as KOOS and Lysholm, extrusion in weight-bearing and extension positions often persists, potentially compromising long-term outcomes [14]. Kodama et al. further demonstrated that transtibial fixation effectively suppresses posterior extrusion in flexion, preserving dynamic stability and minimizing cartilage degeneration [16]. Epidemiological studies have provided a broader understanding of MMPRTs. Kamatsuki et al. identified key demographic trends, with higher BMI correlating with younger onset of MMPRTs. They also noted that complete tears were more likely to result in painful symptoms, underscoring the importance of early and accurate diagnosis [20]. The clinical significance of MMPRTs lies in their potential to progress to severe knee osteoarthritis if left untreated. While surgical interventions show favorable short-term outcomes, long-term challenges persist, including incomplete restoration of extrusion and its correlation with cartilage degeneration [14]. Future research should focus on optimizing surgical techniques, standardizing rehabilitation protocols, and understanding long-term biomechanical changes to improve outcomes. MMPRTs present a complex clinical challenge with significant implications for knee joint health. Advances in surgical techniques and growing insights into the etiology and biomechanics have improved outcomes, but long-term efficacy remains an area of ongoing research. Personalized treatment strategies based on patient-specific factors, such as age, BMI, and tear characteristics, may further enhance outcomes in this diverse patient population.
MRTs pose significant challenges due to their impact on knee biomechanics and progression to osteoarthritis. Timely diagnosis and appropriate management, including surgical repair when feasible, are crucial to preserving meniscal function and delaying degenerative changes. Future research should focus on refining treatment strategies and addressing long-term outcomes to optimize patient care.
Early diagnosis and appropriate surgical intervention in MRTs can preserve knee function and delay osteoarthritis progression.
References
- 1.Lee DW, Ha JK, Kim JG. Medial meniscus posterior root tear: A comprehensive review. Knee Surg Relat Res 2014;26:125-34. [Google Scholar | PubMed]
- 2.Feucht MJ, Kühle J, Bode G, Mehl J, Schmal H. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy 2015;31:1808-16. [Google Scholar | PubMed]
- 3.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: Radiographic and clinical results with a 2-year follow-up. Arthroscopy 2009;25:951-8. [Google Scholar | PubMed]
- 4.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. J Bone Joint Surg Am 2008;90:1922-31. [Google Scholar | PubMed]
- 5.Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J Bone Joint Surg Am. 2009 Oct 1;91 Suppl 2:257-70. doi: 10.2106/JBJS.I.00500. [Google Scholar | PubMed | CrossRef]
- 6.Chung KS, Ha JK, Ra HJ, Kim JG. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy 2016;32:1613-21. [Google Scholar | PubMed]
- 7.Perry AK, Lavoie-Gagne O, Knapik DM, Maheshwer B, Hodakowski A, Gursoy S, et al. Examining the efficacy of medial meniscus posterior root repair: A meta-analysis and systematic review of biomechanical and clinical outcomes. Am J Sports Med 2023;51:17-26. [Google Scholar | PubMed]
- 8.Chang PS, Radtke L, Ward P, Brophy RH. Midterm outcomes of posterior medial meniscus root tear repair: A systematic review. Am J Sports Med 2022;50:342-9. [Google Scholar | PubMed]
- 9.Bernard CD, Kennedy NI, Tagliero AJ, Tagliero AJ, Camp CL, Saris DB, et al. Medial meniscus posterior root tear treatment: A matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med 2020;48:392-9. [Google Scholar | PubMed]
- 10.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Meniscal root tears: Current concepts review. Arch Bone Jt Surg 2018;6:250-9. [Google Scholar | PubMed]
- 11.LaPrade RF, LaPrade CM, James EW. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg 2021;29:281-9. [Google Scholar | PubMed]
- 12.Xue H, Furumatsu T, Hiranaka T, Kintaka K, Higashihara N, Tamura M, et al. Concomitant posterior anchoring further reduces posterior meniscal extrusion during pullout repair of medial meniscus posterior root tears: A retrospective study. Int Orthop 2023;47:2391-400. [Google Scholar | PubMed]
- 13.Moon HS, Choi CH, Jung M, Chung K, Jung SH, Kim YH, et al. Medial meniscus posterior root tear: How far have we come and what remains? Medicina (Kaunas) 2023;59:1181. [Google Scholar | PubMed]
- 14.Takase R, Ohsawa T, Hashimoto S, Kurihara S, Yanagisawa S, Hagiwara K, et al. Insufficient restoration of meniscal extrusion by transtibial pullout repair for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc 2023;31:4895-902. [Google Scholar | PubMed]
- 15.Karpinski K, Forkel P, Häner M, Bierke S, Petersen W. Etiology of posterior meniscus root tears: Medial vs. lateral. Arch Orthop Trauma Surg 2023;143:429-37. [Google Scholar | PubMed]
- 16.Kodama Y, Furumatsu T, Masuda S, Okazaki Y, Kamatsuki Y, Okazaki Y, et al. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 2020;28:3416-25. [Google Scholar | PubMed]
- 17.Mundal K, Geeslin AG, Solheim E, Inderhaug E. Differences Between Traumatic and Degenerative Medial Meniscus Posterior Root Tears: A Systematic Review. Am J Sports Med. 2025 Jan;53(1):228-233. doi: 10.1177/03635465241237254. [Google Scholar | PubMed | CrossRef]
- 18.Hantouly AT, Aminake G, Khan AS, Ayyan M, Olory B, Zikria B, et al. Meniscus root tears: State of the art. Int Orthop 2024;48:955-64. [Google Scholar | PubMed]
- 19.Wu TY. Arthroscopic medial meniscus posterior root repair with centralization using knotless suture anchors. Arthrosc Tech 2022;11:e661-8. [Google Scholar | PubMed]
- 20.Kamatsuki Y, Furumatsu T, Hiranaka T, Okazaki Y, Kintaka K, Kodama Y, et al. Epidemiological features of acute [Google Scholar | PubMed]