Careful surgery with clear margins is imperative to restore function and eliminate disability in desmoid fibrosis cases especially when occurring in very young children. Complete and thorough eradication via excision may suffice, however, close monitoring and meticulous follow-up is are indicated given the benign though locally aggressive nature of this lesion.
Dr. Shenbaghavalli Thanikaimalai, Department of Orthopaedics, Bai Jerbai Wadia hospital for children, Mumbai, Maharashtra, India. E-mail: shenscorp@gmail.com
Introduction: Desmoid fibromatosis (DF) is a rare, fibrous neoplasm arising from the musculoaponeurotic structures. It is also named aggressive fibromatosis owing to its rapid progression in spite the nature. In this case report we want to highlight the unusual site of presentation, the age group, the surgical challenges, behavior of the tumor, and the various treatment methods. Owing to the rarity of diagnosis and unusual sites in our cases, they can be missed which eventually causes significant morbidity.
Case Report: We present two cases of gradually progressing soft tissue tumors posing significant deformity with functional restrictions, at unusual sites where diagnosis was delayed causing difficulty and loss of function. A 7-year-old female child presented with a history of swelling over the right arm and restriction of movements at the right elbow and shoulder joint approximately for the past 2 years or more. She had a previous history of incision and drainage at junction, and middle third arm around 3 years ago, following which a swelling and restriction of movements steadily increased. On presentation to us, higher Imaging revealed a large soft tissue mass involving the triceps, but not infiltrating the bone. Case 2, an 8-month-old child presented with a slow-growing tumor of the right neck causing a severe torticollis deformity. Parents were advised physiotherapy and also had a steroid injection intramuscularly elsewhere, which showed no improvement. On examination, a large, firm swelling along the entire length of the sternocleiodomastoid muscle was causing severe restriction of movements of the neck. An open biopsy done proved both to be a DF which can be locally aggressive if not treated in time. Surgical resection was done for functional improvement. This is the youngest age group reported ever in literature .
Conclusion: A simple, safe, and clear surgical resection alone can bring about restoration of functional limitations and can have a disease-free survival in not very aggressive DF tumors provided close monitoring is guaranteed for check of recurrence.
Keywords: Desmoid tumor, desmoid type fibromatosis, musculoaponeurotic fibrous neoplasm, benign locally aggressive tumor.
According to the World Health Organization, desmoid tumor (DT) is a “clonal fibroblastic proliferation that arises in the deep soft tissues and is characterized by infiltrated growth and a tendency toward local recurrence but inability to metastasize,” even though it may be multifocal in the same limb or body part. Commonly, fibromatosis occurs in the anterior abdominal region in adults, and in extreme cases, it invaded the shoulder, trunk, and hip as well. In this report, we outline two such pediatric cases with accurate diagnosis despite unusual sites, their management, supportive investigations, and current recommendations of the treatment plans available for fibromatosis.
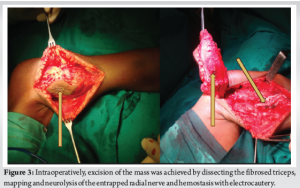
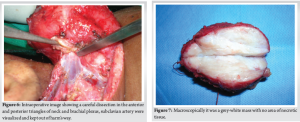
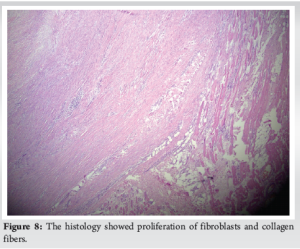
Case 1, A 7-year-old female child presented elsewhere with a history of a gradually growing swelling in her right arm for the past 2 years and an inability to flex the elbow. A small intervention was performed at the same site elsewhere 3 years ago but there were no records of details. She had no similar swellings elsewhere in her body, constitutional symptoms, or positive family history. On examination, a diffuse swelling was present over the Postero-lateral aspect of the right arm. It was approximately 7 × 6 cm in size, not fixed to the bone, non-fluctuant, firm in consistency, and the skin overlying the mass was pinchable with no distended veins. The elbow was completely stiff and only an abduction of 90° at the shoulder (Fig. 1). Radiographs of the arm and shoulder region showed no bony abnormality and only a thought-provoking soft tissue shadow in the middle third – proximal third junction of the humerus. Blood investigations ruled out infection. Magnetic resonance imaging (MRI) showed a large, soft tissue heterogeneous (T1 and T2) signal intensity mass, involving the triceps, extending up to the humerus but not infiltrating it (Fig. 2). An open biopsy of the mass done confirmed the diagnosis of desmoid fibromatosis (DF) by exhibiting proliferation of fibroblasts and collagen fibers characteristic of this condition. She underwent wide excision of the mass with the help of the onco-surgery team through posterior approach to humerus with a 15 cm long incision, enclosing biopsy scar. Intraoperatively, excision of the mass was achieved by dissecting the fibrosed triceps, mapping, and neurolysis of the entrapped radial nerve and hemostasis with electrocautery (Fig. 3). No intraoperative neuromonitoring or tourniquet was needed. The mass was retrieved in toto, margins were well circumscribed, hence no chemotherapy or radiotherapy was given. The child was immobilized with a POP cast in elbow flexion of 90° for 3 weeks. Gradual, active, and passive physiotherapy was done. Extension was achieved by gravity since more than 2/3 of the triceps mass was lost. At 2 years after index surgery, the child had gained near normal elbow range of movements and full abduction of the shoulder (Fig. 4) and was able to do activities of daily living, independently. Case 2, 8-month-old child presented with a slow-growing tumor of the right neck causing a severe torticollis deformity (Fig. 5a and b). Parents were advised physiotherapy and also had a steroid injection intramuscularly elsewhere, which showed no improvement. On examination, a large, firm swelling along the entire length of the sternocleido mastoid muscle was causing severe restriction of movements of the neck. Bony abnormalities were ruled out with X-ray; MRI done revealed DF, juxta internal jugular vein. The tumor was excised with musculoskeletal oncology and head–neck faciomaxillary surgical team and a cervical to chest pop was given for 6 weeks followed by a distraction collar for 3 months. No nerve damage occurred intraoperatively as careful dissection was done in the anterior and posterior triangles of neck and brachial plexus, subclavian artery was visualized and kept out of harm’s way (Fig. 6). Macroscopically it was a grey-white mass with no area of necrotic tissue (Fig. 7) and the histology showed proliferation of fibroblasts and collagen fibers (Fig. 8) characteristic of this condition. The child received no chemotherapy and as the tumor was excised in toto. The child was followed till 18 months postoperatively on a collar, hada mild residual tilt but the parents were satisfied with the clinical outcome.



Fibromatosis, desmoid type (DTF), known for its aggressiveness is a rare tumor relatively, can affect both the children and the adults with an overall incidence of two to four new diagnoses per 1 million/year [1]. The peak incidence of the tumor is between 6 and 15 years of age and between puberty to 40 years of age with a higher incidence in females during adolescence. The exact cause of DTF remains unclear, but certain factors such as surgical scars, familial adenomatous polyposis, and elevated estrogen levels have been identified as potential risk factors. DTs have a high propensity for recurrence, as nuclear and cytoplasmic features are similar histologically to a malignant tumor [1]. They can produce potential complications such as invasion of adjacent muscle, and nerves, causing pain and limitation of joint movement or contractures, deformities, compression, or obstruction of nearby organs and blood vessels sometimes life-threatening. Some patients remain asymptomatic or have non-specific symptoms and this differs based on its location and severity [2]. Strategies for treatment are complex as they are locally aggressive tumors with high recurrence rates. As the tumor is unpredictable and considering the morbidity that is associated with surgery, a conservative, step-wise approach is currently preferred for managing DT [3]. A wait-and-see approach can be applied for newly diagnosed tumors as studies have showed a significant percentage of tumors are stable on long term without treatment [4,5]. In some cases, it may spontaneously regress as reported by Bonvalot et al. [6]. Our patients needed surgical intervention as it was restricting their range of movements causing functional disability. The primary goal of surgery is to obtain an optimal resection with negative margins for the best oncological outcome. However, no significant difference in the 5-year progression-free survival rate has been reported by some studies with positive versus negative surgical margins [7,8]. Radiation therapy has shown benefits in both roles as an adjuvant and in post-operative therapy, for tumors with positive surgical margins or local recurrences. But its efficacy is controversial, especially in children [9,10]. Although the French sarcoma group study demonstrated good outcomes for chemotherapy, [11] the role of chemotherapy is unclear and limited [12] as well as when hormonal replacement therapy is tumors secreting receptor B for older patients [13]. In a case report by Ali Kaygin et al., a DT arising from the popliteal fossa was surgically resected and no subsequent radiotherapy or chemotherapy was given. Eighteen months later, similar to our case 2, the subject was free from disease without local recurrences or distant metastasis [14]. No recurrent lesion was observed at the 6th month postoperative MRI follow-up examination as per Pallarés Martí et al. wherein postoperative radiotherapy was dismissed for a giant DT of the neck with involvement of skull and scapula [15]. Total excision may not be possible always because of the local invasive nature of the tumor, and sometimes vital structures may not give the opportunity for total excision. The overall recurrence rate in cases of infantile fibromatosis, a DT of the sternocleidomastoid, is reported to be 50%, and recurrence is more frequent, especially in head and neck location (60–70%) due to the inability to completely excise these tumors. Radiotherapy and chemotherapy are reserved for only unresectable tumors [16]. Our case 2 had a complete excision and hence no chemo/radiotherapy was given.[17].
On confirming the validity and good prognosis of our case scenario and consultation with an orthopedic onco-surgeon, the patient was counseled to report back on a 6 monthly follow-up. We therefore concluded the current treatment as surgical resection only, as the surgical margins were tumor-free when assessed by histopathological examination. We wish to bring to light that a simple, safe, and clear surgical resection alone can bring about restoration of functional limitations and can have a disease-free survival in not very aggressive DF tumors provided close monitoring is guaranteed for check of recurrence.
Despite various recommendations for chemotherapy or adjuvant hormonal/radiotherapy, our subjects underwent just surgical resection and received no adjuvant therapy and proceeded to do well clinically with a close observation for recurrence.
References
- 1.World Health Organization, WHO. In: Fletcher C, Bridge JA, Hogendoorn PC, Mertens F, editors. WHO Classification of Tumours of Soft Tissue and Bone: WHO Classification of Tumours. 4th ed., Vol. 5. Switzerland: World Health Organization; 2013. [Google Scholar | PubMed]
- 2.Rouger-Gaudichon J, Gariazzo L, Thébault E, Brethon B, Fenwarth L, Gambart M, et al. Impact of COVID-19 on cancer care: A survey from the French society of pediatric oncology (SFCE). Pediatr Blood Cancer 2021;68:e28554. [Google Scholar | PubMed]
- 3.Gronchi A, Colombo C, Le Pechoux C, Dei Tos AP, Le Cesne A, Marrari A, et al. Sporadic desmoid-type fibromatosis: A stepwise approach to a non-metastasising neoplasm--a position paper from the Italian and the French sarcoma group. Ann Oncol 2014;25:578-83. [Google Scholar | PubMed]
- 4.Kasper B, Baumgarten C, Bonvalot S, Haas R, Haller F, Hohenberger P, et al. Management of sporadic desmoid-type fibromatosis: A European consensus approach based on patients’ and professionals’ expertise - a sarcoma patients EuroNet and European organisation for research and treatment of cancer/soft tissue and bone sarcoma group initiative. Eur J Cancer 2015;51:127-36. [Google Scholar | PubMed]
- 5.Fiore M, Rimareix F, Mariani L, Collini P, Le Péchoux C, Casali PG, et al. Desmoid-type fibromatosis: A front-line conservative approach to select patients for surgical treatment. Ann Surg Oncol 2009;16:2587-93. [Google Scholar | PubMed]
- 6.Bonvalot S, Ternes N, Fiore M, Bitsakou G, Colombo C, Honoré C, et al. Spontaneous regression of primary abdominal wall desmoid tumors: More common than previously thought. Ann Surg Oncol 2013;20:4096-102. [Google Scholar | PubMed]
- 7.Crago AM, Denton B, Salas S, Dufresne A, Mezhir JJ, Hameed M, et al. A prognostic nomogram for prediction of recurrence in desmoid fibromatosis. Ann Surg 2013;258:347-53. [Google Scholar | PubMed]
- 8.Merchant NB, Lewis JJ, Woodruff JM, Leung DH, Brennan MF. Extremity and trunk desmoid tumors: A multifactorial analysis of outcome. Cancer 1999;86:2045-52. [Google Scholar | PubMed]
- 9.Jelinek JA, Stelzer KJ, Conrad E, Bruckner J, Kliot M, Koh WJ, et al. The efficacy of radiotherapy as postoperative treatment for desmoid tumors. Int J Radiat Oncol Biol Phys 2001;50:121-5. [Google Scholar | PubMed]
- 10.Goy BW, Lee SP, Eilber F, Dorey F, Eckardt J, Fu YS, et al. The role of adjuvant radiotherapy in the treatment of resectable desmoid tumors. Int J Radiat Oncol Biol Phys 1997;39:659-65. [Google Scholar | PubMed]
- 11.Garbay D, Le Cesne A, Penel N, Chevreau C, Marec-Berard P, Blay JY, et al. Chemotherapy in patients with desmoid tumors: A study from the French sarcoma group (FSG). Ann Oncol 2012;23:182-6. [Google Scholar | PubMed]
- 12.Camargo VP, Keohan ML, D’Adamo DR, Antonescu CR, Brennan MF, Singer S, et al. Clinical outcomes of systemic therapy for patients with deep fibromatosis (desmoid tumors). Cancer 2010;116:2258-65. [Google Scholar | PubMed]
- 13.Deyrup AT, Tretiakova M, Montag AG. Estrogen receptor-beta expression in extraabdominal fibromatoses: An analysis of 40 cases. Cancer 2006;106:208-13. [Google Scholar | PubMed]
- 14.Ali Kaygin M, Dag O, Erkut B, Ates A, Kayaoglu RC, Kadioglu H. Extra-abdominal fibromatosis (desmoid tumor): A rare tumor of the lower extremity arising from the popliteal fossa. Case Rep Vasc Med 2011;2011:184906. [Google Scholar | PubMed]
- 15.Pallarés Martí B, Oishi N, Valdivieso L, Zapater E, Basterra J. A giant desmoid neck tumor: A case report. Braz J Otorhinolaryngol 2021;87:634-7. [Google Scholar | PubMed]
- 16.Ekinci S, Karnak I, Tanyel FC. Infantile fibromatosis of the sternocleidomastoid muscle mimicking muscular torticollis. J Pediatr Surg 2004;39:1424-5. [Google Scholar | PubMed]








