A differential diagnosis of RA should be kept in all cases of wrist swelling, even in the absence of features of inflammatory arthropathy
Dr. Pradeep Kumar Pathak, Department of Orthopaedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India. E-mail: dr.pathak09@gmail.com
Introduction: Chronic volar wrist swelling is a diagnostic challenge, particularly in tuberculosis-endemic regions, where both infectious and inflammatory causes must be considered. Rheumatoid tenosynovitis, an extra-articular manifestation of rheumatoid arthritis (RA), can mimic infectious tenosynovitis, especially in seronegative patients.
Case Report: We report a case of a 44-year-old male presenting with progressive pain and swelling over the volar aspect of the right wrist for 2 months. Clinical findings of a local rise in temperature, tenderness, and limitation of range of motion suggested flexor tendon tenosynovitis, with differential diagnoses including abscess, tuberculous tenosynovitis, Giant cell tumours, or inflammatory arthritis. Ultrasound and magnetic resonance imaging revealed tendon sheath thickening and features of median nerve compression. The patient had elevated inflammatory markers, but rheumatoid factor and anti-cyclic citrullinated peptide were negative. Excision biopsy and synovectomy with median nerve decompression were performed. Surgical exploration revealed hypertrophied synovium around the flexor tendons. Histopathology confirmed a rheumatoid nodule, establishing the diagnosis of rheumatoid tenosynovitis despite negative serology. The patient’s recovery was uneventful postoperatively.
Conclusion: This case highlights the importance of considering rheumatoid tenosynovitis in the differential diagnosis of chronic wrist swelling, even in seronegative individuals. In ambiguous cases, surgical intervention not only alleviates symptoms but also allows for definitive diagnosis through histopathology. A multidisciplinary and vigilant approach is crucial to prevent misdiagnosis and preserve hand function in such presentations.
Keywords: Rheumatoid arthritis, tenosynovitis, tenosynovectomy.
Chronic wrist swelling and pain is a clinical presentation with a broad differential diagnosis, ranging from overuse injuries and infections to systemic inflammatory diseases. Tenosynovitis, particularly of the flexor tendons, can be caused by repetitive strain, localized infection, or autoimmune conditions such as rheumatoid arthritis (RA) [1]. The disorder can affect any sheathed tendon in the body; however, it is most common in the hand, wrist, and foot [1]. Diagnosing inflammatory tenosynovitis can be challenging, especially in seronegative patients, where laboratory markers may not point clearly toward an autoimmune cause. In tuberculosis (TB)-endemic areas, TB tenosynovitis is often a strong consideration when imaging and clinical symptoms suggest synovial thickening or mass-like lesions [2]. Flexor tenosynovitis is a deep space infection of an upper extremity digit that causes significant morbidity [3]. This case report details a patient who presented with signs and symptoms suggestive of infectious and giant cell tumour (GCT) and was ultimately diagnosed with rheumatoid tenosynovitis on histopathology after surgical intervention [4].
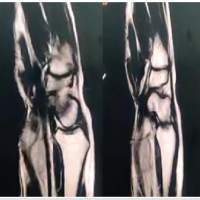
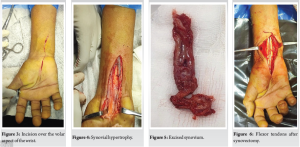
A 44-year-old male presented with complaints of pain and swelling over the volar aspect of his right wrist that had persisted for the past 2 months. The pain had started earlier than the swelling. The pain was insidious in onset and gradual in progression and was moderate-to-severe in intensity. It is aggravated with passive and active movements of the wrist and metacarpophalangeal (MCP) joints. The patient was unable to make a fist, resulting in weakness of grip, which led to difficulty in performing activities of daily living. There was no history of involvement of any other small or large joints of the body. There was no history of morning stiffness, fever, weight loss, or night cries. On examination, local temperature was raised, and diffuse tenderness was present over the swelling. The skin was normal and not adherent to underlying structures. A full range of extension was present in the MCP, proximal interphalangeal, and distal interphalangeal joints, but flexion of these movements was limited. Laboratory investigations revealed raised C-reactive protein and erythrocyte sedimentation rate, whereas the total leukocyte count remained within normal limits at 6800/µL. Rheumatoid factor and anti-cyclic citrullinated peptide (CCP) antibodies were negative. Basic imaging in the form of a plain X-ray of the wrist (Fig. 1) showed no abnormalities. Given the persistent swelling and non-specific laboratory findings, a high-resolution ultrasound of the wrist was performed. The ultrasound demonstrated a heterogeneous hypoechoic collection with thickening of the tendon sheath along the flexor pollicis longus (FPL) tendon, as well as flattening of the median nerve within the carpal tunnel, suggesting possible compressive tenosynovitis. Based on the above findings, a differential diagnosis of TB and GCT of the flexor sheath was made. The differential diagnosis of RA was not kept as there were no signs or symptoms suggestive of RA, and also the anti-CCP antibody and RA factors were negative. To further evaluate the extent and nature of the lesion, a contrast-enhanced magnetic resonance imaging (MRI) of the wrist was done. It showed tenosynovitis of the flexor tendons with marked synovial enhancement of the wrist joint, suggestive of an inflammatory aetiology (Fig. 2a and b). Based on the imaging and persistent symptoms, a surgical approach was planned for both diagnostic and therapeutic purposes. The patient underwent an open exploration of the wrist through a volar approach (Fig. 3).


Surgical technique
A 10 cm long incision was given starting from 3 to 4 cm distal to the distal wrist crease in line with the radial border of the ring finger and extended 7 cm proximal to the wrist crease. The incision was curved ulnar in the wrist to protect the palmar cutaneous branch of the median nerve. Subcutaneous tissue and fascia were cut and retracted. The synovial sheath around the FPL, flexor digitorum superficialis, and flexor digitorum profundus tendons was found to be swollen, boggy, and dirty looking (Fig. 4). Transverse carpal ligaments were cut, and complete synovectomy was performed along with decompression of the median nerve. The excised synovium (Fig. 5) was sent for histopathological examination. The gross appearance of tendons became normal after tenosynovectomy (Fig. 6). Histopathological analysis revealed granulation tissue and fibrocollagenous stroma with nodular areas exhibiting central fibrinoid necrosis. There was peripheral palisading of epithelioid histiocytes and the presence of multiple Langhans-type giant cells. These findings were consistent with a rheumatoid nodule, confirming the diagnosis of rheumatoid tenosynovitis despite the absence of serological markers for RA (Fig. 7a and b). Postoperatively, the patient had an uneventful recovery. Follow-up showed resolution of pain, with a complete, and painless range of motion restored in the wrist, and no evidence of recurrence.
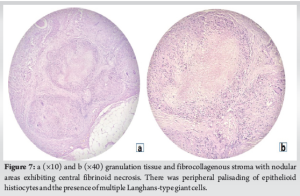
This case underscores the diagnostic complexity of chronic wrist swelling, particularly when seronegative inflammatory arthritis presents with localized symptoms that mimic infection. This becomes even more challenging when isolated tenosynovitis is the sole manifestation, with no involvement of other small or large joints. Rheumatoid tenosynovitis is a common manifestation in patients with RA, often leading to significant morbidity due to tendon sheath inflammation and compression neuropathies such as carpal tunnel syndrome [5]. While rheumatoid factor and anti-CCP antibodies are useful diagnostic tools, their absence does not exclude the disease [6,7]. In this patient, the negative rheumatoid factor and lack of systemic RA features delayed the consideration of an inflammatory etiology. In TB-endemic settings, tubercular tenosynovitis is an important consideration in cases of chronic synovial swelling [8]. However, the absence of systemic signs of TB and negative findings on imaging for caseation or bone involvement made TB less likely in this case [4]. Imaging modalities such as ultrasound and MRI were essential in identifying soft tissue pathology, suggesting tenosynovitis and median nerve compression, although they could not distinguish the exact cause. Ultimately, the diagnosis was confirmed only after surgical intervention and histopathological examination. Histology remains the gold standard in differentiating rheumatoid nodules from infectious granulomas, especially in ambiguous clinical scenarios. The characteristic features of fibrinoid necrosis, palisading histiocytes, and Langhans-type giant cells provided conclusive evidence of an underlying autoimmune pathology [9,10]. Early surgical intervention not only provided symptomatic relief but also allowed for definitive diagnosis and prevention of long-term functional impairment (Table 1).
Rheumatoid tenosynovitis should remain a differential consideration in cases of chronic wrist swelling and pain, even in the absence of classical symptoms or positive serological markers. This case illustrates that imaging may suggest but not confirm the diagnosis, and a definitive diagnosis may require surgical exploration and histopathology. Prompt synovectomy and decompression can provide excellent clinical outcomes, as demonstrated in this patient, who had complete resolution of symptoms and regained full wrist function. A high index of suspicion and a multidisciplinary approach are key in managing such atypical presentations of seronegative RA.
A differential diagnosis of RA should be kept in all cases of wrist swelling, even in the absence of features of inflammatory arthropathy.
References
- 1.Ray G, Sandean DP, Tall MA. Tenosynovitis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: http://www.ncbi.nlm.nih.gov/books/NBK544324 [Last accessed on 2025 May 26]. [Google Scholar | PubMed]
- 2.Pimm LH, Waugh W. Tuberculous tenosynovitis. J Bone Joint Surg Br 1957;39-B:91-101. [Google Scholar | PubMed]
- 3.Mehta P, Thoppil J, Koyfman A, Long B. High risk and low prevalence diseases: Flexor tenosynovitis. Am J Emerg Med 2024;77:132-8. [Google Scholar | PubMed]
- 4.Wakefield RJ, Balint PV, Szkudlarek M, Filippucci E, Backhaus M, D’Agostino MA, et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol 2005;32:2485-7. [Google Scholar | PubMed]
- 5.Izumiyama T, Miyazawa M. Importance of tenosynovitis in preventing the progression through rheumatoid arthritis continuum. Mod Rheumatol 2023;33:868-74. [Google Scholar | PubMed]
- 6.Paroli M, Sirinian MI. When autoantibodies are missing: The challenge of seronegative rheumatoid arthritis. Antibodies (Basel) 2023;12:69. [Google Scholar | PubMed]
- 7.Pratt AG, Isaacs JD. Seronegative rheumatoid arthritis: Pathogenetic and therapeutic aspects. Best Pract Res Clin Rheumatol 2014;28:651-9. [Google Scholar | PubMed]
- 8.Shah MA, Shah I. Wrist swelling - is it tuberculosis? J Family Med Prim Care 2017;6:865-6. [Google Scholar | PubMed]
- 9.Shah KK, Pritt BS, Alexander MP. Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis 2017;7:1-12. [Google Scholar | PubMed]
- 10.Fareez F, Moodley J, Popovic S, Lu JQ. Rheumatoid nodules: A narrative review of histopathological progression and diagnostic consideration. Clin Rheumatol 2023;42:1753-65. [Google Scholar | PubMed]
- 11.Iyengar K, Manickavasagar T, Nadkarni J, Mansour P, Loh W. Bilateral recurrent wrist flexor tenosynovitis and rice body formation in a patient with sero-negative rheumatoid arthritis: A case report and review of literature. Int J Surg Case Rep 2011;2:208-11. [Google Scholar | PubMed]
- 12.Kushwanth E, Arvind Natarajan K, Mervinrosario PM. A Rare Case of Rheumatoid Tenosynovitis with Unilateral R.A. Mimicking Tuberculosis Tenosynovitis. Available from: https://www.jrmds.in/articles/a-rare-case-of-rheumatoid-tenosynovitis-with-unilateral-ra-mimicking-tuberculosis-tenosynovitis-94880.html [Last accessed on 2025 Jun 20]. [Google Scholar | PubMed]
- 13.Boudon A, Opota O, Dan D. A refractory tenosynovitis of the wrist: A case report. J Med Case Rep 2022;16:75. [Google Scholar | PubMed]
- 14.Tiwari P, Kaur H, Bansal N, Jaura SS. Rheumatoid or tubercular: Flexor tenosynovitis of the wrist with rice bodies. J Fam Med Prim Care 2022;11:6518. [Google Scholar | PubMed]
- 15.Tian Y, Zhou HB, Yi K, Wang KJ. Idiopathic tenosynovitis of the wrist with multiple rice bodies: A case report and review of literature. World J Clin Cases 2022;10:11908-20. [Google Scholar | PubMed]