Arthroscopic surgery should be considered for elderly patients with recurrent inferior patellar dislocation to prevent further episodes and facilitate early mobilization, as closed reduction alone may not be sufficient.
Dr. Jeremy Silver, Rutgers Robert Wood Johnson Medical School, Department of Orthopaedic Surgery, 1 Robert Wood Johnson Place, New Brunswick, NJ 08901. E-mail: Jeremy.Silver@rutgers.edu
Introduction: Inferior patellar dislocations in elderly patients are rare and typically occur in the presence of significant patellofemoral arthritis. These dislocations often present as a locked knee, which can be mistaken for other knee pathologies. While treatment has generally involved closed reduction, there is limited literature on recurrence and the role of surgical intervention.
Case Report: An 85-year-old female presented with a locked right knee following a fall, unable to bear weight or extend the knee. Radiographs and MRI revealed an inferior patellar dislocation due to a superior patellar osteophyte interacting with a defect in the lateral femoral condyle. Initial closed reduction was successful but followed by a recurrence of the dislocation seven weeks later. Arthroscopic surgery, including debridement of the patellar osteophyte and trochlear osteochondral defect, provided definitive treatment. The patient remained symptom-free at 12 months follow-up with no further dislocations.
Conclusion: This case highlights the challenge of managing inferior patellar dislocations in elderly patients, with closed reduction and immobilization often insufficient to prevent recurrence. Arthroscopic surgery should be considered in cases of recurrent dislocation to allow for early mobilization and minimize the risk of further episodes. Level of evidence: Level V Case Report
Keywords: Knee, arthroscopy, inferior patellar dislocation, locked knee, patellofemoral arthritis.
The differential diagnosis of patients presenting with a locked knee is broad but most often includes meniscal lesions, ligamentous injuries, loose bodies, and degenerative changes [1]. Patellar dislocations are a more rare cause of acute locked knee. While most patellar dislocations occur laterally, they can occur in any direction. Uncommonly, inferior patellar dislocations may present with a locked knee. Bankes and Eastwood proposed a classification system for inferior patellar dislocations [2]. Type I injuries occur in younger males and involve horizontal rotation of the patella. Type II injuries occur in elderly patients with significant patellofemoral arthritis. These are most commonly hyperflexion injuries where superior patellar osteophytes hinge on the intercondylar area of the femur. Type II injuries are rare and are limited to case reports. Several studies have shown successful treatment of these type II inferior patellar dislocations with closed reduction and immobilization [2-7]. In other cases, arthroscopic or open surgery was necessary to treat the condition [7-11]. In two of these cases, successful initial closed reduction was complicated by quick recurrence of the dislocation, which necessitated surgery [8,10]. To our knowledge, we present the first published case of a recurrent inferior patellar dislocation several weeks after initial treatment with closed reduction.
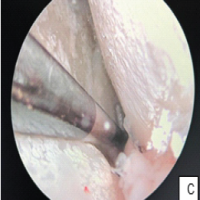
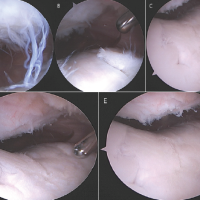
The patient is an 85-year-old female who presented 3 weeks after suffering acute onset right knee pain after a fall at home onto her bent knee. She was unable to bear weight or extend her knee since the injury and was stuck in 80° of flexion. Initial work-up at an outside institution included radiographs and magnetic resonance imaging (MRI) which revealed an inferior patella dislocation where a superior patellar osteophyte hinged on a defect in the lateral femoral condyle (Fig. 1). MRI showed an intact quadriceps and significant patellofemoral osteoarthritis. In the office, a closed reduction maneuver was performed. The patient was placed supine, and the knee was injected with 2% lidocaine. The knee was then hyperflexed while inferiorly translating the patella out of the osteochondral defect (OCD) after which the knee was brought back into extension. Clinically, the patella was reduced with immediate resolution of pain. However, the patella dislocated while being flexed during post-reduction X-rays requiring a second reduction maneuver. The reduction was maintained the second time and confirmed on radiographs. The patient was made weight-bearing as tolerated with a walker and knee immobilizer. One week later, her pain was resolved and radiographs in the office confirmed maintenance of reduction. She remained weight-bearing as tolerated and was encouraged to do straight leg raises to improve quadriceps strength. The knee immobilizer was maintained. At three weeks after reduction, she was pain-free and able to flex and extend from 0 to 90°. She was started on formal physical therapy and given a hinged knee sleeve with instructions to not flex beyond 90°. At 7 weeks, she had regained full range of motion and quadriceps strength. The hinged knee sleeve was discontinued. Two days after discontinuing the knee brace, she dislocated in her sleep. The knee was again injected but two attempted closed reductions in the office were unsuccessful and operative intervention was performed that evening. After intubation in the operating room, she remained stuck in flexion. She subsequently underwent arthroscopic takedown of the patellar osteophyte and debridement of the lateral trochlear OCD with the resolution of her dislocation (Fig. 2 and 3). An accessory superomedial portal allowed easier access to the patellar osteophyte. The patient was discharged home the following day, weight bearing as tolerated, with an ace bandage but no immobilization. She received home physical therapy. At one-month follow-up, the patient was pain-free, had a good range of motion, and was very satisfied with the outcome. Radiographs showed maintenance of reduction. At the final follow-up 12 months later, the patient remains pain-free with no recurrence of the dislocation.


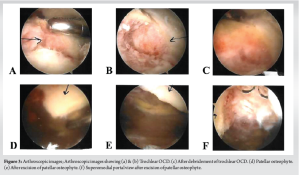
There have been several case reports describing inferior patellar dislocation in elderly patients [2-11]. Treatment of these injuries has ranged from closed reduction to arthroscopic or open surgical treatment. We present the first late recurrence of inferior patellar dislocation in an elderly patient after initial treatment with closed reduction and immobilization. Multiple studies have shown successful treatment of type II inferior patellar dislocations with closed reductions and 3–4 weeks of immobilization [2-7]. Closed reduction under general anesthesia was performed in two cases [3,4]. Reduction under IV sedation in the emergency department was performed in two cases [2,6]. Intra-articular injection was used in one case and a peripheral nerve block was used in another [5,7]. While follow-up varied in these cases, there was no reported recurrence of dislocation. In our case, initial closed reduction was accomplished after intra-articular injection via hyperflexion of the knee and a downward force on the patella followed by gradual knee extension. Several other studies reported similar reduction mechanisms [2,4,5,7,8]. Wight et al. reported a different mechanism that included flexing the knee to 90°, applying an anterior drawer force to the tibia, and then counter-pressure to the inferior pole of the patella [6]. Two studies reported a recurrence of the dislocation after the initial closed reduction [8,10]. Syed and Ramesh reported a case of a patient who re-dislocated 8 days after the initial closed reduction [10]. The patient was immobilized in a knee splint for only 6 days and then dislocated while in bed. Subsequent closed reduction was unsuccessful, and she was treated with osteophyte removal via an open medial parapatellar approach. Barlow et al. reported a recurrent dislocation 1 day after the initial closed reduction as the patient was unable to tolerate her splint [8]. She was treated with arthroscopic resection of a patellar osteophyte and smoothing of the lateral femoral condyle. In our study, the patient had an immediate initial recurrence of her dislocation while being flexed during her post-reduction X-rays. While the second reduction was successful and maintained for 7 weeks, repeat dislocations may suggest increased instability that would benefit from surgical treatment. Two additional studies reported failed initial attempts at closed reduction resulting in operative treatment [9,11]. Shivarathre and Keys reported a unique case of inferior patellar dislocation 12 months after total knee arthroplasty without patellar resurfacing [9]. This case was successfully treated through open debridement of osteophytes. Zimmermann et al. reported a case of failed closed reduction treated successfully with arthroscopic debridement [11]. Yoshioka et al. reported two cases, one of which they performed open removal of osteophyte and plate fixation of a lateral femoral condyle fracture even after successful closed reduction [7]. The differential diagnosis of an acute locked knee is broad and work-up relies on history, physical exam, and diagnostic tests, which often include an MRI [1,12]. In our case, the patient presented with a locked knee and patella baja. While this clinical scenario often points towards a quadriceps tendon rupture, the unique appearance of the lateral knee X-ray indicates inferior patellar dislocation (Fig. 1). In fact, the quadriceps tendon was intact in all of the reported cases of type II inferior patellar dislocations. In the case of an elderly patient presenting with acute locked knee and patella baja, inferior patellar dislocation must be considered. Initial work-up should include AP and lateral X-rays of the knee. A lateral view demonstrating a superior patellar osteophyte hinged on the femoral condyle is pathognomonic of this injury and obviates the need for an MRI. Closed reduction under intra-articular block or sedation should be attempted and confirmed via AP and lateral knee X-rays. Even if closed reduction is successful, however, arthroscopic surgery to debride the patellar osteophyte and smooth the femoral condyle should be considered. This minimally invasive treatment allows early mobilization and limits the chance of recurrence.
Inferior patellar dislocations in elderly patients are rare and limited to case reports. Treatment has involved closed reduction alone or in combination with arthroscopic or open surgery. We have presented the first late re-dislocation after the closed reduction. Arthroscopic surgery should be considered for all elderly patients with inferior patellar dislocation to limit recurrence and allow early mobilization.
Elderly patients presenting with a locked knee and patella baja may have an inferior patellar dislocation, often caused by a superior patellar osteophyte hinging on the femoral condyle. While closed reduction can be initially successful, arthroscopic debridement should be considered to reduce recurrence and enable early mobilization.
References
- 1.Allum RL, Jones JR. The locked knee. Injury 1986;17:256-8. [Google Scholar | PubMed]
- 2.Bankes MJ, Eastwood DM. Inferior dislocation of the patella in the degenerate knee. Injury 2002;33:528-9. [Google Scholar | PubMed]
- 3.Joshi RP. Inferior dislocation of the patella. Injury 1997;28:389-90. [Google Scholar | PubMed]
- 4.McCarthy TA, Quinn B, Pegum JM. Inferior dislocation of the patella: An unusual cause of a locked knee. Ir J Med Sci 2001;170:209-10. [Google Scholar | PubMed]
- 5.Qin Y, Mei J. Inferior dislocated patella locked by a loose body. BMJ Case Rep 2021;14:e240471. [Google Scholar | PubMed]
- 6.Wight L, James D. Intra-articular patellar dislocation: A technique for closed reduction: A case report and review of the literature. JBJS Case Connect 2017;7:e94. [Google Scholar | PubMed]
- 7.Yoshioka S, Arai Y, Ikoma K, Fujita S, Akai T, Sakuragi R, et al. Two cases of inferior dislocation of the patella with impaction into the femoral trochlea of osteophytes on the superior pole of the patella. Case Rep Orthop 2013;2013:691739. [Google Scholar | PubMed]
- 8.Barlow D, Foong KS, Rhee SJ, Sutcliffe W, Griffin SJ. Recurrent locked knee caused by an impaction fracture following inferior patellar dislocation: A case report. J Med Case Rep 2011;5:347. [Google Scholar | PubMed]
- 9.Shivarathre DG, Keys GW. Inferior dislocation of patella after a total knee replacement-a case report. J Knee Surg 2013;26:S16-8. [Google Scholar | PubMed]
- 10.Syed MA, Ramesh P. Recurrent inferior patellar dislocation in an osteo-arthritic knee. Knee 2004;11:141-2. [Google Scholar | PubMed]
- 11.Zimmermann J, Gruninger P, Babians A, Zingg U. Unusual total knee immobilization in an elderly patient due to inferior patella dislocation: Case report and review of the literature. Trauma Case Rep 2021;33:100481. [Google Scholar | PubMed]
- 12.Bansal P, Deehan DJ, Gregory RJ. Diagnosing the acutely locked knee. Injury 2002;33:495-8. [Google Scholar | PubMed]