Prompt diagnosis, appropriate surgical intervention, and effective physical therapy of VISI are pivotal factors in enhancing patient outcomes.
Dr. Abdelrahman Mustafa-Kamel Alfarra, Department of Orthopaedics, The Artificial Limbs and Polio Center, Gaza, Palestine. E-mail: aboad84@hotmil.com
Introduction: Advancements in radiology have enhanced the understanding of carpal instability and its biomechanics.
Case Report: This case report discusses a 37-year-old male patient who suffered a distal radius fracture and subsequent volar intercalated segment instability (VISI). Despite being less common than other forms of carpal instability, VISI presents clinical significance. Initial evaluations post-fracture did not identify the instability. After identifying VISI, an open reduction and internal fixation procedure with Luno-Triquetral Fusion and bone grafting was performed. Post-operative immobilization aided successful fusion and enhanced wrist stability. Follow-up showed symptom improvement, increased range of motion, and improved hand function.
Conclusion: This study underscores the importance of diagnosing and addressing lesser-known carpal instability patterns, emphasizing careful clinical assessments, advanced radiology, appropriate surgical and physical therapy interventions, and vigilant follow-up.
Keywords: Carpal instability, volar intercalated segment instability, distal radius fracture, open reduction and internal fixation, luno-triquetral fusion, immobilization, clinical outcome, radiology, wrist function.
Lunotriquetral (LT) joint instability is often undetected, potentially resulting in LT dissociation. Diagnosis challenges stem from associated injuries in high-impact sports and the difficulty in identifying LT ligament injury through typical radiographs [1]. LT ligamentous injury is rarer compared to other proximal carpal row ligamentous injuries, leading to limited understanding and diagnosis [2]. The prevalence of ligamentous injury associated with fractures of the distal radius has been reported to be in 8.5–15% of patients when evaluated arthroscopically [3]. The interosseous LT ligament is the main intrinsic ligamentous supporter of the LT joint. It is described as “C” shaped and is divided into 3 parts. The volar portion is the strongest and thickest portion and provides the most stability and mainly prevents volar translation. The dorsal portion limits rotational movement, and the combination of all parts of the LT intrinsic ligament prevents dorsal translation [4]. Advancements in radiology have improved understanding of carpal instability and its biomechanics [5]. The lunate bone plays a vital role in upholding carpal stability, yet it could experience destabilization if its linkage to the LT and the scapholunate ligament is compromised [6]. Volar intercalated segment instability (VISI), a lesser-known form of carpal instability, involves lunate tilting toward the palm due to the rupture of the LT ligament [7]. Despite being less common than dorsal intercalated segment instability (DISI), VISI has clinical significance. Patients with VISI experience wrist discomfort and “clunking” sounds during ulnar deviation. Disruptions in radiocarpal ligaments, especially the ulnar part of the volar arcuate ligament and the LT ligament, are central to this instability [2]. Whether static or dynamic, careful attention is essential due to potential complications.
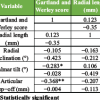
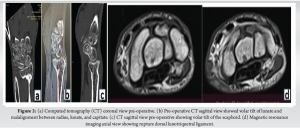
The medical record pertains to a 37-year-old male patient who initially sought medical attention at a different facility subsequent to a fall from a ladder on April 11, 2022. The patient’s instinctive reaction to the fall involved extending his hand to mitigate impact force, resulting in fractures at the distal ends of both radius and ulna [3]. To address these fractures, a closed reduction percutaneous pinning (CRPP) procedure and plaster of Paris (POP) for 6 weeks was performed with the objective of restoring anatomical integrity. Afterward, a physiotherapy program lasting for 6 months was initiated; however, regrettably, there was no observed improvement or advancement in joints’ range of motion (ROM) and grip strength [1]. Importantly, the initial examination following the CRPP procedure did not identify any carpal instability. Following this, evaluations conducted at our facility in January 2023 revealed clinical indications consistent with volar segmental intercalated instability, as seen in X-rays, magnetic resonance imaging and computed tomography scans Figs. 1d and 2a, b, c, d. Furthermore, limitations in ROM were apparent in wrist extension and flexion, as well as wrist supination and pronation as seen clinically presented in Fig. 1a, b, c of the clinical presentation [2,7].

Intervention done
On January 12, 2023, an open reduction and internal fixation procedure was performed utilizing a dorsal wrist approach (Fig. 3a and b), which includes midline dorsal wrist incision over the carpal bone, between the 4th (EDC) and 5th (EIP) dorsal wrist extensor compartments, opening of joint capsule, exposure of lunate and triquetrum carpal bones. This surgical intervention aimed to achieve Luno-Triquetral Fusion, employing an Autologous cancellous bone graft sourced from the iliac crest (Fig. 3b). A K-wire was employed as a joystick to assist in the reduction of the scaphoid, and an additional wire was placed between the lunate and triquetrum before insertion of cancellous bone graft in the gap between lunate and triquetrum bones as seen in Fig. 3c and d. the 1st K-wire is kept between scaphoid and radius to maintain the position of scaphoid, closure of capsule and skin was done with interrupted sutures.

Following surgery, a defined period of immobilization through a POP cast was implemented for 3 months. This post-operative immobilization was intended to facilitate healing and promote successful fusion between the lunate and triquetral bones. The outcome of the surgical procedure exhibited successful fusion, as indicated by X-ray assessments demonstrating osseous integration and consolidation (Fig. 4). Once the cast was removed, a physiotherapy treatment plan was initiated promptly to regain mobility, enhance the ROM in the joint, and restore optimal hand functionality [5,8].

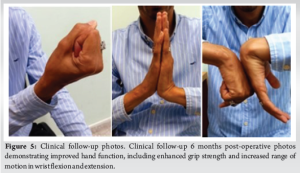
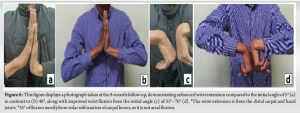
Subsequent clinical evaluations revealed progressive symptom improvement and enhanced wrist joint functionality, including reduced pain levels and increased ROM. The integration of the lunate and triquetral bones contributed to enhanced wrist stability and biomechanical function. Below, in Fig. 4, are successive X-ray images captured at the 2, 3, and 4-month follow-up intervals, depicting improved bone alignment and the gradual progression of fusion healing as time elapsed [9].
Alongside the X-ray images, presented in (Fig. 5 and 6), are photographs captured during a 6-month follow-up of the clinical case. These visuals showcase enhanced hand functionality, encompassing improved grip strength and expanded ROM in both wrist flexion and extension [3,6].
In summation, the surgical intervention yielded a successful outcome characterized by radiographic evidence of fusion, symptomatic amelioration, and improved wrist function. This underscores the effectiveness of the surgical technique, bone grafting method, and post-operative immobilization strategy in achieving the intended therapeutic objectives [4].
The coexistence of VISI with distal radius fractures highlights the necessity for comprehensive evaluation and diagnostic strategies. This case report highlights the intricate diagnostic complexities associated with VISI, an underexplored form of carpal instability. Despite its lower prevalence compared to DISI, VISI holds clinical significance [1,6]. In essence, the report emphasizes the significance of identifying and addressing lesser-known carpal instability patterns, exemplified by VISI subsequent to trauma. It emphasizes the requirement for meticulous clinical assessments, appropriate surgical interventions, and diligent post-operative care to achieve favorable outcomes. The integration of advanced radiological techniques, refined surgical approaches, and attentive clinical management collectively contributed to positive therapeutic advancements [5,7]. These findings align with Vishnu Senthil et al.’s study, suggesting a cautious approach to suspecting VISI following wrist injury and K-wire fixation [10]. Carpal instability resulting from diverse wrist injuries aids in diagnosing persistent wrist pain, aligning with the observations of Muminagic and Kapidzic [7]. Vigilant follow-up plays a pivotal role in effective treatment and the early resolution of potential complications [8].
In conclusion, the pivotal role of the lunate bone in maintaining carpal stability emphasizes its susceptibility to destabilization when stabilization is compromised. While VISI may be less recognized, its clinical significance is notable. Patients experiencing VISI often describe wrist discomfort and “clunking” sounds during ulnar deviation. Notably, disruptions in radiocarpal ligaments, particularly the ulnar part of the volar arcuate ligament and the LT ligament, are central to this instability. Whether in a static or dynamic context, vigilant attention is crucial due to potential complications.
“Early recognition, precise surgical intervention, and diligent physical therapy in cases of rare carpal instability, such as VISI, are paramount for optimizing patient outcomes and restoring wrist function effectively.”
References
- 1.Senthil V, Kottamttavide IV, Shah H. Posttraumatic static volar intercalated segment instability - iatrogenic or missed injury. J Orthop Case Rep 2016;6:59-61. Desai MJ, Kamal RN, Richard MJ. Management of intercarpal ligament injuries associated with distal radius fractures. Hand Clin 2015;31:409-16. [Google Scholar | PubMed]
- 2.Bain GI, Yao J. Diagnosis and management of scapholunate and lunotriquetral ligament tears. Tech Hand Upper Extrem Surg 2006;10:7-15. [Google Scholar | PubMed]
- 3.Wulf CA, Ackerman DB, Rizzo M. Contemporary evaluation and treatment of distal radius fractures. Hand Clin 2007;23:209-26. [Google Scholar | PubMed]
- 4.Murray PM, Peimer CA. Carpal instability: Diagnosis and treatment. J Am Acad Orthop Surg 1995;3:9-19. [Google Scholar | PubMed]
- 5.Ranzenberger LR, Carter KR. Lunotriquetral instability. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/nbk535448 [Last accessed on 2023 Jun 26]. [Google Scholar | PubMed]
- 6.Allingham B, McQueen MM. Scapholunate and lunotriquetral injuries following distal radius fractures. Bone Joint J 2014;96-B:671-7. [Google Scholar | PubMed]
- 7.Muminagic S, Kapidzic T. Wrist instability after injury. Mater Sociomed 2012;24:121-4. [Google Scholar | PubMed]
- 8.Berger RA, Weiss AP. Wrist ligament injuries: Diagnosis, management, and treatment. J Orthop Traum 2004;18:S14-20. [Google Scholar | PubMed]
- 9.Cautilli GP, Weiser RW. Missed diagnosis of carpal instability in distal radius fractures. J Hand Surg 1999;24:741-7. [Google Scholar | PubMed]
- 10.Senthil V, Kottamttavide IV, Shah H. Posttraumatic static volar intercalated segment instability - iatrogenic or missed injury. J Orthop Case Rep 2016;6:59-61. [Google Scholar | PubMed]