Short femoral stems, though traditionally used in primary THA, may be a viable option in select revision THA cases with preserved bone stock, offering benefits like reduced surgical trauma and bone preservation. However, their use remains off-label in revisions, and further research is needed to define proper guidelines.
Ioannis S Vasios, Department of Academic Orthopaedics, Unit for Surgical Reconstruction of Major Joints University General Hospital of Alexandroupolis, Alexandroupolis, Greece. E-mail: giannisvasios@hotmail.gr
Introduction: Total hip arthroplasty (THA) is the gold standard treatment for end-stage hip osteoarthritis. The rise in primary THA incidence has led to a corresponding increase in THA revision rates. Revision surgeries are challenging and pose significant burdens on patients and on healthcare systems worldwide. The use of short stems as revision implants are considered “off-label” and the literature on this application is scarce. Our purpose is to present the results of a revision surgery using a short femoral prosthesis as well as a review of the current literature on this perspective.
Case Report: A 64-year-old male patient suffered from aseptic loosening of the right THA that was revised with a type-3 short femoral prosthesis.
Conclusion: Short femoral stems are a viable option for revision surgeries especially for young patients. Although there are many surgeons who would oppose to their usage in this setting, few would deny that their advantages outnumber their cons.
Keywords: Hip arthroplasty, revision surgery, short stem, downsizing.
Total hip arthroplasty (THA) is one of the most commonly performed procedures and its incidence is increasing exponentially in the last decades along with the increase in life expectancy [1,2]. It is considered the gold-standard treatment of end-stage of hip osteoarthritis as it offers relief from pain, improved mobilization and quality of life [1,2]. More importantly, the excellent long-term outcomes reported in the literature, have rendered THA to be described as the operation of the century [3]. However, along with the increase in primary THA incidence, there is a consequent increase in THA revision rates.[1,4] In fact, an increase of up to 70% is expected until 2030 [1]. Revision surgeries are challenging to treat and cause significant financial burden to patients and healthcare systems [1,5,6]. Taking into account that in the last years a growing number of young patients is subjected to THA and the implants have a limited survival period, it is reasonable for the surgeon to consider that these patients will need in the future one or more revision surgeries [7]. Thus, it is clear that the preservation of as much bone stock as possible is of utmost importance, especially for this group of patients. Cementless short femoral stems have gained in popularity in the last decades. In the current literature, there is neither a clear definition for these stems nor a standardized classification system [8-14]. The following two definitions seem to be the most prevalent: Short stems are considered those whose total length is less than twice the vertical distance between the tip of the greater trochanter and the base of the lesser trochanter or those stems whose total length is <120 mm [8,15,16]. Despite the existence of several classification systems, none of them provides a fully integrated approach, and none is widely adopted in clinical practice [10,17]. Routinely, revision surgeries are accompanied by extended skin incisions, bone osteotomies, and excessive bone loss. For these reasons, more complex implants and longer stems are used, so sufficient anchoring in the diaphysis could be achieved [4,7,15]. The use of a short stem as a revision implant is still considered an “off-label’’ indication. Although it may seem reasonable when short stems are used for the revision of a failed hip resurfacing arthroplasty or in failed internal fixation of a proximal femoral fracture, their use when revising a conventional THA is considered unconventional [18,19]. Therefore, the evidence in the literature regarding this application is still scarce [4,15]. The objective of this study is to present a case report of a revision THA using a short stem implant, with the aim of providing valuable insights in respect to indications, technique, and advantages of this approach. This study aims to contribute to the literature by providing significant information and stimulating further research on a yet under-reported topic.
A 64-year-old male patient presented to the orthopedic outpatient department complaining of painful right THA during his everyday activities and severe limping. The indication for the primary THA was end-stage primary hip osteoarthritis and it was performed 7 years ago through the modified Hardinge’s approach. The past medical history included benign prostatic hyperplasia. The clinical evaluation revealed approximately 2.5 cm leg-length discrepancy and at the standard pre-operative radiological evaluation it was identified loosening of the right femoral stem since radiolucent lines around the stem, anterior thigh pain, and varus malalignment were evident. The pre-operative work-up was negative for infection, and aseptic loosening was considered the final diagnosis. The severe leg-length discrepancy and the high hip center were the two main reasons for the revision of the acetabular component. A modified Hardinge’s approach was performed. After the removal of the acetabular and femoral components, a thorough debridement of the acetabular bone bed and the femoral canal was performed until sufficient bleeding was evident. The femoral bone defect was classified as type I whereas the acetabular bone defect was classified as type IIIA according to Paprosky classification (type III according to Saleh classification) [20,21] (Fig. 1). Moreover, intra-operative tissue samples were collected and sent for microbiological cultures which were finally negative. The acetabular bone defect was addressed with a cup-cage construct in conjunction with the impaction of morselized allograft (fresh-frozen femoral head). The ischial hook was placed at the obturator foramen and the iliac flanges were adjusted accordingly to the iliac bone and stabilized with five screws. The femoral component was revised using a type 3 (trochanteric sparing) short stem since there was sufficient bone stock and of good quality the proximal femur. Before the placement of the final components, an intra-operative fluoroscopic image was obtained to confirm the correct sizes and position of the implants.
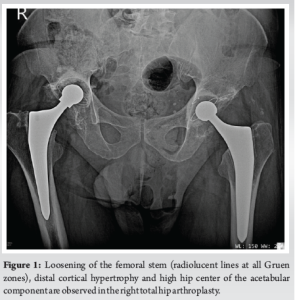
The post-operative course was uneventful and at the final 27 months of follow-up, the patient was free of pain and reported excellent patient-reported outcome measures (PROMs) (Harris Hip Score=93.85, Oxford Hip Score=41, Forgotten Joint Score=86.36, Patient Health Questionnaire-9=0, EQ-5D-5L=0.928, Pain Catastrophizing Scale=2, visual analogue scale=1). No radiolucent lines were observed around the stem as well as around the acetabular component. Moreover, the allograft osseointegration was classified as successful according to the Oswestry radiological classification system [22]. Small amounts of heterotopic ossification were developed in the right hip joint both at the lateral (Brooker 1) and medial side (type 3) [23,24] (Fig. 2).

The increase in primary THA incidence has led to a subsequent increase in THA revision rates [1,4]. In the current literature, it still remains unclear whether the more active lifestyle of the patients, especially the younger ones, leads to a more accelerated loosening of the implants [25]. Considering the increasing trend of younger patients undergoing THA in the last decades, coupled with the finite lifespan of implants, it is prudent for surgeons to anticipate the likelihood of these patients requiring one or more revision surgeries in the future [7]. Consequently, it becomes evident that preserving the maximum possible bone stock is crucial, particularly for this demographic. Short stems are accompanied by numerous advantages as their design aims to mimic the proximal femoral anatomy and hip biomechanics [26]. They are less invasive, in the context of causing less damage in the proximal femur, since less bone is removed during femoral canal’s broaching. Moreover, they allow for easier insertion and more physiological loading which subsequently leads to less stress shielding compared to standard stems. Furthermore, they can be used in femurs with special-unique proximal anatomy such as in cases with proximal-distal mismatch, and they have been associated with diminished anterior thigh pain [2,8,11,16,27,28]. All these features have rendered short stems attractive to the contemporary orthopaedic hip surgery and have led many hip surgeons to include them into their armamentarium [28]. Despite the unique characteristics and the potential benefits of the short stems, there is still a lack of clarity regarding their indications and contraindications. Subsequently, their implementation is depended on surgeon’s preference and experience [7]. However, there are some key points that a hip surgeon should bear in mind when this implant type is utilized. First and foremost, good bone quality of the proximal femur is necessary in order to achieve a stable press-fit fixation [7,29]. However, this does not mean that preoperatively the patients need to undergo bone mineral density testing. Moreover, advanced age, high body mass index, Dorr C femoral canal, rheumatoid arthritis, post-traumatic arthritis, and proximal femoral deformities (with or without previous corrective osteotomies) are not absolute contraindications for the implementation of a short femoral prosthesis [7,27,30]. The concept of downsizing the femoral component in a revision setting was initially introduced in a limited case series of Coutandin et al. The study reported excellent results, both clinical and radiological, without serious complications in the mid-term follow-up (100% survival rate, mean follow-up=3.32 years), concluding that this approach may offer advantages in selected cases [4]. However, the principles of revision arthroplasty should always be adhered to ensure optimal patient outcomes. Some key principles include: stable implant fixation, preservation of as much bone stock as possible (in the already compromised), and minimization of surgical trauma along with its consequences [31]. Considering all the aforementioned principles and the extensive experience of our major joint reconstruction unit in utilizing short stems during primary total hip arthroplasties, we were able to employ the “downsizing” approach for the femoral component using a type 3 short stem (trochanteric sparing type) [8,32]. The short femoral prosthesis was implanted easily, achieved excellent short-term outcomes, both clinically and radiologically, maintained the bone mineral density as its conventional counterparts and did not cause anterior thigh pain [12,26]. Our patient did not experience any minor or major post-operative complications, was free of pain and reported excellent PROMs in the short-term follow-up period.
Short stems are gaining in popularity in the contemporary orthopedic surgery with various implants being available regarding their design and features. However, their use is mainly restricted to primary THAs in young patients with good bone quality in the proximal femur. There are only scarce reports (including the current one) of short stems being used as “off label” revision implants, showing good-to-excellent outcomes. Despite the promising reported outcomes, further studies are needed to confirm their efficacy either as a primary or as a revision implant in cases with the corresponding indications. Nevertheless, in order to give clear answers to all these questions, it may be necessary to clarify firstly their definition and adopt a single-unified classification system.
Short femoral stems offer a viable option for revision THA, particularly in younger patients with preserved bone quality. Despite being considered an “off-label” approach, short stems provide several benefits, including reduced bone resection, less stress shielding, and the potential for improved patient outcomes with fewer complications. While these advantages make short stems an attractive choice in revision settings, further research is necessary to solidify their role, particularly in defining their indications, contraindications, and a standardized classification system. This study contributes valuable insight into the use of short stems in revision THA, supporting the need for additional exploration in this area.
References
- 1.Patel I, Nham F, Zalikha AK, El-Othmani MM. Epidemiology of total hip arthroplasty: Demographics, comorbidities and outcomes. Arthroplasty 2023;5:2. [Google Scholar | PubMed]
- 2.Tottas S, Ververidis A, Kougioumtzis I, Tilkeridis K, Tsigalou C, Karaglani M, et al. MINIMA short stem versus standard Profemur (TL) stem in primary total hip replacement: A comparative study. Cureus 2022;14:e23771. [Google Scholar | PubMed]
- 3.Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. Lancet 2007;370:1508-19. [Google Scholar | PubMed]
- 4.Coutandin M, Afghanyar Y, Rehbein P, Dargel J, Drees P, Kutzner KP. Downsizing in total hip arthroplasty. A short stem as a revision implant. Orthopade 2022;51:230-8. [Google Scholar | PubMed]
- 5.Lamb JN, Jain S, King SW, West RM, Pandit HG. Risk factors for revision of polished taper-slip cemented stems for periprosthetic femoral fracture after primary total hip replacement: A registry-based cohort study from the national joint registry for England, wales, Northern Ireland and the Isle of man. J Bone Joint Surg Am 2020;102:1600-8. [Google Scholar | PubMed]
- 6.Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, et al. Current epidemiology of revision total hip arthroplasty in the United States: National inpatient sample 2009 to 2013. J Arthroplasty 2017;32:2088-92. [Google Scholar | PubMed]
- 7.Ishaque BA. Short stem for total hip arthroplasty (THA) - overview, patient selection and perspectives by using the metha® hip stem system. Orthop Res Rev 2022;14:77-89. [Google Scholar | PubMed]
- 8.Drosos GI, Touzopoulos P. Short stems in total hip replacement: Evidence on primary stability according to the stem type. HIP Int 2019;29:118-27. [Google Scholar | PubMed]
- 9.Gómez-García F, Fernández-Fairen M, Espinosa-Mendoza RL. A proposal for the study of cementless short-stem hip prostheses. Acta Ortop Mex 2016;30:204-15. [Google Scholar | PubMed]
- 10.Kim JT, Yoo JJ. Implant design in cementless hip arthroplasty. Hip Pelvis 2016;28:65-75. [Google Scholar | PubMed]
- 11.Feyen H, Shimmin AJ. Is the length of the femoral component important in primary total hip replacement? Bone Joint J 2014;96-B:442-8. [Google Scholar | PubMed]
- 12.Van Oldenrijk J, Molleman J, Klaver M, Poolman RW, Haverkamp D. Revision rate after short-stem total hip arthroplasty: A systematic review of 49 studies. Acta Orthop 2014;85:250-8. [Google Scholar | PubMed]
- 13.Stulberg SD, Patel RM. The short stem: Promises and pitfalls. Bone Joint J 2013;95-B 11 Suppl A:57-62. [Google Scholar | PubMed]
- 14.Gulow J, Scholz R, Freiherr Von Salis-Soglio G. [Short-stemmed endoprostheses in total hip arthroplasty]. Orthopade 2007;36:353-9. [Google Scholar | PubMed]
- 15.Liu Z, Liu B, Zhang B, Ma W, Wu T, Huo J, et al. Short uncemented femoral component for hip revision: Prognosis and risk factors associated with failure. BMC Surg 2021;21:192. [Google Scholar | PubMed]
- 16.Drosos GI, Tottas S, Kougioumtzis I, Tilkeridis K, Chatzipapas C, Ververidis A. Total hip replacement using MINIMA® short stem: A short-term follow-up study. World J Orthop 2020;11:232-42. [Google Scholar | PubMed]
- 17.Radaelli M, Buchalter DB, Mont MA, Schwarzkopf R, Hepinstall MS. A new classification system for cementless femoral stems in total hip arthroplasty. J Arthroplasty 2023;38:502-10. [Google Scholar | PubMed]
- 18.Afghanyar Y, Coutandin M, Schneider M, Drees P, Kutzner KP. Conversion of failed internal fixation in proximal femur fractures using calcar-guided short-stem total hip arthroplasty. J Orthop Traumatol 2022;23:34. [Google Scholar | PubMed]
- 19.Coutandin M, Afghanyar Y, Drees P, Dargel J, Rehbein P, Kutzner KP. Can hip resurfacing be safely revised with short-stem total hip arthroplasty? A case series of six patients. J Orthop 2021;24:274-9. [Google Scholar | PubMed]
- 20.Ibrahim DA, Fernando ND. Classifications in brief: The paprosky classification of femoral bone loss. Clin Orthop Relat Res 2017;475:917-21. [Google Scholar | PubMed]
- 21.Ghanem M, Zajonz D, Heyde CE, Roth A. Acetabular defect classification and management : Revision arthroplasty of the acetabular cup based on 3-point fixation. Orthopade 2020;49:432-42. [Google Scholar | PubMed]
- 22.Ding H, Mao Y, Yu B, Zhu Z, Li H, Yu B, et al. The use of morselized allografts without impaction and cemented cage support in acetabular revision surgery: A 4- to 9-year follow-up. J Orthop Surg Res 2015;10:77. [Google Scholar | PubMed]
- 23.Hug KT, Alton TB, Gee AO. Classifications in brief: Brooker classification of heterotopic ossification after total hip arthroplasty. Clin Orthop Relat Res 2015;473:2154-7. [Google Scholar | PubMed]
- 24.DeBaun MR, Ziino C, LaPrade C, Pun S, Avedian RS, Bellino MJ. An anatomic classification for heterotopic ossification about the hip. J Orthop 2020;21:228-31. [Google Scholar | PubMed]
- 25.Negm AM, Beaupre LA, Goplen CM, Weeks C, Jones CA. A scoping review of total hip arthroplasty survival and reoperation rates in patients of 55 years or younger: Health services implications for revision surgeries. Arthroplast Today 2022;16:247-58.e6. [Google Scholar | PubMed]
- 26.Sivaloganathan. Neck-Sparing Short Femoral Stems: A Meta-Analysis - ScienceDirect; 2020. Available from: https://www.sciencedirect.com/science/article/pii/S1877056820301900?via%3dihub [Last accessed on 2024 Mar 02]. [Google Scholar | PubMed]
- 27.Bostian PA, Grisez BT, Klein AE, Frye BM. Complex primary total hip arthroplasty: Small stems for big challenges. Arthroplasty Today 2021;8:150-6. [Google Scholar | PubMed]
- 28.Zhang Z, Xing Q, Li J, Jiang Z, Pan Y, Hu Y, et al. A comparison of short-stem prostheses and conventional stem prostheses in primary total hip arthroplasty: A systematic review and meta-analysis of randomized controlled trials. Ann Transl Med 2021;9:231. [Google Scholar | PubMed]
- 29.Gruner A, Heller KD. Patient selection for shorter femoral stems. Orthopedics 2015;38 3 Suppl:S27-32. [Google Scholar | PubMed]
- 30.Zhen P, Chang Y, Yue H, Chen H, Zhou S, Liu J, et al. Primary total hip arthroplasty using a short bone-conserving stem in young adult osteoporotic patients with Dorr type C femoral bone. J Orthop Surg Res 2021;16:17. [Google Scholar | PubMed]
- 31.Lombardi AV Jr., Head WC, Mallory TH, Emerson RH Jr. Principles of reconstruction in revision hip arthroplasty: Technique and results of bone grafts for treatment of femoral and acetabular deficits. J Orthop Sci 1997;2:442-6. [Google Scholar | PubMed]
- 32.Falez F, Casella F, Papalia M. Current concepts, classification, and results in short stem hip arthroplasty. Orthopedics 2015;38 3 Suppl:S6-13. [Google Scholar | PubMed]