Tuberculous tenosynovitis can manifest as compound palmar ganglion, leading to wrist swelling and potential carpal tunnel syndrome, necessitating timely diagnosis and treatment with both surgery and antitubercular therapy in tuberculosis-endemic areas to prevent serious complications
Dr. Shristi Singh, Department of Orthopaedics MMIMSR, Address-I block, Room No-233, MMU Campus, Mullana, Ambala - 133207, Haryana, India. E-mail: shristi2710@gmail.com
Introduction: Tuberculous tenosynovitis is a rare condition predominantly found in developing countries that require prompt medical intervention. Due to its atypical presentation, diagnosis through biopsy and culture is necessary to distinguish it from other diseases. Compound palmar ganglion is an unusual manifestation that can cause swelling around the wrist joint and potentially compress the neural structures, resulting in carpal tunnel syndrome.
Case Report: A 27-year-old female, homemaker complained of pain and tingling sensations in her right hand. Radiological analysis revealed juxta-articular osteopenia with soft tissue swelling. Magnetic resonance imaging identified a spongy soft tissue lesion compressing the median nerve over the flexor retinaculum of the right wrist. The decision was to surgically explore and excise the lesion along with carpal tunnel release. Histopathological examination confirmed tubercular tenosynovitis.
Conclusion: Tubercular compound ganglion is a rare condition that must be kept in mind while treating patients with carpal tunnel syndrome, especially in developing countries where tuberculosis is prevalent. Delayed diagnosis is common due to gradual progression and subtle symptoms except for swelling. Surgical intervention and antitubercular treatment are crucial components of compound palmar ganglion management. Early diagnosis and management are essential for preventing complications.
Keywords: Tuberculous, compound palmar ganglion, carpal tunnel syndrome, flexor retinaculum, tenosynovitis, radical synovectomy.
Tuberculous tenosynovitis is still prevalent in developing countries and it typically occurs through hematogenous dissemination or direct inoculation. Its varied clinical presentation poses a significant public health concern, necessitating immediate medical and surgical treatment in musculoskeletal cases [1-3]. In some instances, this condition can cause compound palmar ganglion, which may result in carpal tunnel syndrome due to the already cramped flexor compartment around the wrist.
A 27-year-old female, homemaker residing in Saharanpur reported pain and tingling sensations in her right hand. We observed a spongy swelling across the wrist with signs of median nerve compression, which was transmitting a fluid impulse across the wrist joint. She had no history of tuberculosis (TB) or contact with any TB patient nor any symptoms of night sweats, weight loss, chronic cough, dyspnea, or hemoptysis. Based on the history, we made few differential diagnoss such as carpal tunnel syndrome, ganglion cyst, rheumatoid arthritis, and fungal infection. Wrist and forearm radiology revealed juxta-articular osteopenia with soft tissue swelling. She did not show any clinical manifestations of TB, but her erythrocyte sedimentation rate (ESR) level was elevated (45 mm), and the Mantoux test was positive. Upon magnetic resonance imaging (MRI), we identified a spongy soft tissue lesion compressing the median nerve over the flexor retinaculum of the right wrist (Fig. 1). Our decision was to surgically explore and excise the lesion, along with carpal tunnel release to decompress the median nerve. During surgery, we discovered a small lesion compressing the structures within the wrist, with the flexor tendon sheaths encapsulated by the mass. Careful dissection enabled us to remove the complete lesion while preserving all essential structures. During surgery, there was a singular encapsulated mass that was fully excised, followed by thorough washing and wound closure (Fig. 2).
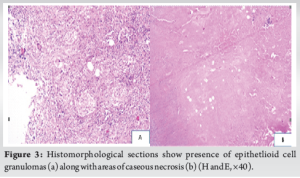
 Histopathological examination confirmed the presence of epithelioid cell granulomas, areas of caseous necrosis, and solid chronic inflammatory infiltrate. The Langhan’s and foreign-body giant cells altogether suggested tubercular tenosynovitis (Fig. 3).
Histopathological examination confirmed the presence of epithelioid cell granulomas, areas of caseous necrosis, and solid chronic inflammatory infiltrate. The Langhan’s and foreign-body giant cells altogether suggested tubercular tenosynovitis (Fig. 3).
 According to the World Health Organization guidelines, the patient was started with 2 months of isoniazid (H), rifampicin (R), pyrazinamide (Z), ethambutol (E) in the intensive phase followed by 4-month continuation phase of Isoniazid and Rifampicin HR thrice a week [4]. Since the disease was in its early stages and joint cartilage remained preserved, we initiated early rehabilitation to avoid severe complications such as stiffness and reflex sympathetic dystrophy. We began range-of-movement exercises of the wrist and hand on the 2nd post-operative day and gradually increased them based on the patient’s pain tolerance. On subsequent follow-up visits, the patient exhibited total recovery from numbness, and after 3 months, regained full functionality of the affected side. After completion of 6 months of antitubercular treatment (ATT), the patient underwent a review, and there was no indication of recurrence.
According to the World Health Organization guidelines, the patient was started with 2 months of isoniazid (H), rifampicin (R), pyrazinamide (Z), ethambutol (E) in the intensive phase followed by 4-month continuation phase of Isoniazid and Rifampicin HR thrice a week [4]. Since the disease was in its early stages and joint cartilage remained preserved, we initiated early rehabilitation to avoid severe complications such as stiffness and reflex sympathetic dystrophy. We began range-of-movement exercises of the wrist and hand on the 2nd post-operative day and gradually increased them based on the patient’s pain tolerance. On subsequent follow-up visits, the patient exhibited total recovery from numbness, and after 3 months, regained full functionality of the affected side. After completion of 6 months of antitubercular treatment (ATT), the patient underwent a review, and there was no indication of recurrence.
Tuberculous tenosynovitis is a well-known condition that primarily affects the volar tendons of the wrist; however, it seldom affects the synovial sheath of the hand [5]. It constitutes <1% of skeletal TB cases. Other conditions, such as systemic lupus erythromatous (SLE), rheumatoid arthritis, gouty arthritis, pigmented villonodular synovitis, and fungal infection of the tendon sheaths, can present similarly. A compound palmar ganglion causing compression neuropathy of the median nerve is a rare occurrence. Due to the gradual progression and subtle symptoms of the disease, diagnosis is often delayed [6]. Therefore, timely recognition and treatment are crucial, as the lesion can cause significant destruction. Histopathological examination and culture are necessary as it can mimic other inflammatory conditions such as SLE, rheumatoid arthritis, gouty arthritis, and fungal infections [7-9]. Wide excision of the lesion, thorough debridement, and release of the carpal tunnel are necessary surgical measures to prevent further recurrences. Our patient did not exhibit the commonly described risk factors in the literature, and the mechanism of infection remained unclear, despite her residence in a TB-endemic region.
Tubercular tenosynovitis TTS progresses through three histopathological stages, determined by the organism’s virulence, disease duration, and the individual’s resistance [10].
- Hygromatous stage: Characterized by serous exudates within the tendon sheath, with the tendon itself remaining intact
- Serofibrinous stage: Granulation tissue replaces the tendon sheath, leading to the formation of rice or melon bodies
- Fungoid stage: Marked by caseation, abscess and sinus formation, bone involvement, and potential tendon rupture.
If untreated, TTS can spread to adjacent bones, joints, and the deep spaces of the hand and forearm [11].
Our patient had signs of nerve compression but there were no local signs of inflammation over the swelling, and a systemic evaluation did not reveal any tubercular foci of infection. Laboratory tests, including complete blood count, ESR, and C-reactive protein, may be either normal [11-13] or elevated [14,15]; however, these markers are non-specific for TTS, and a normal result does not exclude the diagnosis [1,12]. In extrapulmonary TB, chest X-rays are typically normal and cannot rule out TTS [1,12,15]. Radiographic findings of TTS involving the wrist may include bone erosions or cavitation, localized osteoporosis, severe destruction, and ankylosis in advanced stages [16]. These features are non-specific and can mimic inflammatory arthritis, pigmented villonodular synovitis, gout, or soft-tissue tumors [16]. Ultrasonography can help detect synovial thickening, peritendinous effusion, pus formation, and lesion extension in suspected TTS cases, but it is operator-dependent and non-specific [12]. MRI, being more sensitive and specific than ultrasound, is preferred for detecting and visualizing tubercular involvement of the synovial tendon sheaths. According to the literature, the duration of ATT for TTS ranges from 6 to 12 months when combined with surgical debridement [1,11-14]. Some authors have reported complete resolution with 12 months of ATT alone, without the need for surgical intervention [15]. ATT should be initiated as soon as the diagnosis is established, and completing the full course is crucial to prevent recurrence and the development of resistant strains [12]. The role of surgical debridement as a first-line treatment for TTS remains controversial [10,15]. Tuli suggests that surgery should be considered in patients who show resistance to 4–5 months of ATT [10]. Other indications for surgical intervention include large mass lesions requiring debulking, advanced disease (Stage 2 or 3) [12], and cases causing median nerve compression [14,17]. Many authors advocate for surgical management through debulking tenosynovectomy, combined with appropriate chemotherapy and carpal tunnel release, to reduce the risk of recurrence [14,15,17].
In developing countries like India, where TB is prevalent, physicians should keep tubercular compound ganglion as a differential diagnosis while treating patients with carpal tunnel syndrome. Slow progression and an initially asymptomatic presentation, except for swelling, contribute to delayed diagnosis of this condition. Meanwhile, compound palmar ganglion is more commonly linked to rheumatoid arthritis in western countries. MRI combined with nerve conduction studies is the gold standard investigation for diagnosing tubercular tenosynovitis. Both surgical intervention and ATT are crucial components of compound palmar ganglion treatment. Early diagnosis and management are critical for preventing complications [18,19].
The clinical message of the case report is that tuberculous tenosynovitis of the wrist can present as a compound palmar ganglion, causing compression neuropathy of the median nerve and resulting in carpal tunnel syndrome. Diagnosis may be delayed due to the gradual progression and initially asymptomatic presentation, but timely recognition and treatment are crucial to prevent significant destruction. MRI combined with nerve conduction studies is the gold standard investigation for diagnosing tubercular tenosynovitis. Wide excision of the lesion, thorough debridement, and release of the carpal tunnel are necessary surgical measures to prevent further recurrences. Early diagnosis and management are critical for preventing complications, and physicians in developing countries where TB is prevalent should consider tubercular compound ganglion as a differential diagnosis while treating patients with carpal tunnel syndrome.
References
- 1.Bayram S, Ersen A, Altan M, Durmaz H. Tuberculosis tenosynovitis with multiple rice bodies of the flexor tendons in the wrist: A case report. Int J Surg Case Rep 2016;27:129-32. [Google Scholar | PubMed]
- 2.Stirrat CR. Treatment of tenosynovitis in rheumatoid arthritis. Hand Clin 1989;5:169-75. [Google Scholar | PubMed]
- 3.Patel RS, Jain PK. Epidemiology of tuberculous tenosynovitis in developing countries. J Orthop Res 2012;30:796-801. [Google Scholar | PubMed]
- 4.Maher D, Chaulet P, Spinaci S, Harries A. Treatment of Tuberculosis: Guidelines for National Programmes. 2nd ed. Switzerland: World Health Organization; 1997. [Google Scholar | PubMed]
- 5.Hoffman KL, Bergman AG, Hoffman DK, Harris DP. Tuberculous tenosynovitis of the flexor tendons of the wrist: MR imaging with pathologic correlation. Skeletal Radiol 1996;25:186-8. [Google Scholar | PubMed]
- 6.Shen PH, Chu CM, Huang GS, Wu SS, Lee CH. Tuberculous tenosynovitis of the flexor tendons of the wrist and hand. J Med Sci 2002;22:227-9. [Google Scholar | PubMed]
- 7.Cuomo A, Pirpiris M, Otsuka NY. Case report: Biceps tenosynovial rice bodies. J Pediatr Orthop B 2006;15:423-5. [Google Scholar | PubMed]
- 8.Lall H, Nag SK, Jain VK, Khare R, Mittal D. Tuberculous extensor tenosynovitis of the wrist with extensor pollicis longus rupture: A report. J Med Case Rep 2009;3:142. [Google Scholar | PubMed]
- 9.Tyllianakis M, Kasimatis G, Athanaselis S, Melachrinou M. Rice-body formation and tenosynovitis of the wrist: A report. J Orthop Surg 2006;14:208-11. [Google Scholar | PubMed]
- 10.Tuli SM. Tuberculosis of the Skeletal System: Bone, Joints, Spine, and Bursal Sheaths. 3rd ed. New Delhi: Jaypee Brothers Medical Publishers; 2004. [Google Scholar | PubMed]
- 11.Wali H, Al-Khuwaitir S, Hafeez MA. Compound palmar ganglion: A case report and literature review. Ann Saudi Med 1986;6:55-8. [Google Scholar | PubMed]
- 12.Suwannaphisit S, Ranong NN. Tuberculous tenosynovitis of the flexor tendons of the hand and wrist: A case report and mini-review. Ann Med Surg (Lond) 2020;57:249-52. [Google Scholar | PubMed]
- 13.Panigrahi S, Jain M, Panda R. Patient with tuberculous flexor tenosynovitis of the hand. BMJ Case Rep 2021;14:e243091. [Google Scholar | PubMed]
- 14.Altaf W, Attarde D, Sancheti P. Tubercular compound palmar ganglion presenting as a severe carpal tunnel syndrome a case report. J Clin Orthop Trauma 2020;11:S889-91. [Google Scholar | PubMed]
- 15.Jain A, Rohilla R, Devgan A, Wadhwani J. Tubercular tenosynovitis of hand: A rare presentation. J Orthop Case Rep 2016;6:69-72. [Google Scholar | PubMed]
- 16.Rajadurai N. Tuberculous tenosynovitis of the wrist joint: Imaging findings on MRI. J Infect Dis Ther 2016;4:307. [Google Scholar | PubMed]
- 17.Baidoo PK, Baddoo D, Ocloo A, Agbley D, Lartey S, Baddoo NA, et al. Tuberculous tenosynovitis of the flexor tendons of the wrist: A case report. BMC Res Notes 2018;11:238. [Google Scholar | PubMed]
- 18.Kumar V, Nijhawan S, Singh M. Tubercular tenosynovitis: A rare case report. Cureus 2019;11:e5806. [Google Scholar | PubMed]
- 19.Choudhary R, Ansari MT, Jain AK, Singhania S, Amrani H, Tekwani K. Tubercular tenosynovitis of the hand. J Clin Diagn Res 2017;11:PD18-20. [Google Scholar | PubMed]
- 20.Kumar V, Nijhawan S, Singh M. Tubercular tenosynovitis: A rare case report. Cureus 2019;11:e5806. [Google Scholar | PubMed]
- 21.Choudhary R, Ansari MT, Jain AK, Singhania S, Amrani H, Tekwani K. Tubercular tenosynovitis of the hand. J Clin Diagn Res 2017;11:PD18-20. [Google Scholar | PubMed]