This case emphasizes the importance of thorough neuropsychiatric evaluation to identify appropriate candidates for bilateral robotic total knee replacement, thereby preventing the rare complication of sequential bilateral posterior knee dislocation
Dr. Deepak D Chitragar, Consultant Joint Replacement Surgeon, Devadoss Multispeciality Hospital, Madurai, Tamil Nadu, India. E-mail: drdeeppak@gmail.com
Introduction: To date, there have been no documented cases of sequential bilateral posterior knee dislocation following robotic-assisted bilateral total knee arthroplasty (TKA) in the literature. Robotic-assisted TKA is gaining traction due to its potential advantages in precision and patient outcomes. Sequential bilateral TKA offers several benefits, Nevertheless, complications can still arise, some of which are rare and difficult to manage. One such complication is posterior tibiofemoral dislocation after primary TKA, can lead to severe consequences and is influenced by various patient-related and surgeon-related risk factors, we present case of rarest of rare sequential knee dislocation and challenges in managing such a case, bring awareness about the risk factor to surgeons.
Case Report: A 65-year-old woman presented with an atraumatic posterior knee dislocation 3 months after undergoing robotic-assisted total knee replacement (TKR) 8 months earlier. The right knee was managed with extensive hamstring release and the debridement, antibiotics, and implant retention technique with change of poly insert, while the left knee was treated with knee arthrodesis. The underlying cause of these complications was identified as patient-related neuropsychiatric illness accompanied by hypertonia.
Conclusion: Posterior knee dislocation is a rare complication that can occur even after robotic-assisted TKR. The occurrence of sequential bilateral dislocation is exceptionally uncommon and presents significant management challenges. It is crucial to consider patient-related factors, such as neuropsychiatric disorders, when planning robotic TKR. A thorough neuropsychiatric evaluation is essential for selecting candidates for bilateral procedures to ensure optimal outcomes and patient satisfaction following robotic TKR.
Keywords: Posterior knee dislocation, sequential, bilateral, robotic assisted total knee replacement, neuropsychiatric.
Robotic-assisted total knee arthroplasty (TKA) is increasingly recognized for its potential advantages in precision and improved patient outcomes, by significantly improving alignment and reduce complications, ultimately contributing to higher patient satisfaction and better functional results post-surgery [1]. Sequential bilateral TKA offers several benefits. These advantages contribute to improved patient satisfaction and efficiency in managing bilateral knee conditions. Studies have shown that performing TKA bilaterally in a single stage can lead to shorter recovery times and lower overall healthcare costs compared to staged procedures or unilateral surgeries [2]. However, despite these advantages, complications can still arise, some of which are rare and challenging to manage. One such complication is tibiofemoral dislocation after primary TKA. The prevalence of knee dislocation following TKA with early posterior stabilized (PS) designs ranged from 1% to 2%, but this has fallen to 0.15–0.5% with newer designs that incorporate changes in the height of the tibial polyethylene post and its anterior translation [3].
While uncommon, this serious complication can lead to significant morbidity and is influenced by various risk factors. The causes of dislocation can be classified into three categories: Patient-related factors, surgeon-related techniques, and implant designs. Patient-related factors identified in the literature include comorbidities, such as obesity, neuropsychiatric disorders, and severe pre-operative deformities (varus/valgus >10°) [4].
Surgeon-related factors often involve technical errors, including improper ligament balancing in flexion and extension, excessive soft-tissue release, and malalignment issues, such as tibial implant malpositioning. In addition, a deficient extensor mechanism may contribute to instability following total knee replacement (TKR) [5]. To date, there have been no documented cases of bilateral sequential posterior knee dislocation following robotic-assisted bilateral TKA in the literature. This case report describes an unusual occurrence of bilateral knee dislocation following robotic-assisted primary knee replacement in a 65-year-old woman. Despite an initially uneventful post-operative course, she developed complications like sequential bilateral knee dislocations. These complications were further complicated by undiagnosed neurological conditions, including late-onset Parkinson’s disease with Alzheimer’s traits. This case underscores the complex interplay between surgical outcomes, patient-specific factors, and undiagnosed comorbidities. It highlights the necessity for comprehensive preoperative assessments, vigilant post-operative monitoring, and adaptable management strategies in response to unexpected complications. The report aims to contribute to the literature on rare complications in robotic-assisted knee arthroplasty while providing insights into managing such challenging cases.
We report a 65-year-old woman (IP No2309804) with 2 years of bilateral knee pain and swelling, worsened by activity. She experienced night pain, cracking sounds, and reduced mobility due to advanced bilateral osteoarthritis (stage 4) with varus and fixed flexion deformity (FFD) (Fig. 1).Sequential bilateral robotic-assisted TKA was recommended.
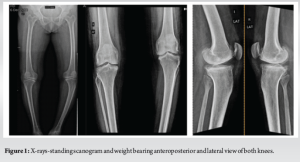
We commenced robotic-assisted TKA at our institution utilizing the Curexo-Meril Cuvis system, a fully automated robotic platform from Korea, in September 2023. This image-based ,implant specific system utilizes computed tomography scans and mill technology, featuring a pre-cut gap check that assists in addressing gaps and achieving soft tissue balance. It allows for the adjustment of implant positioning without the need for soft tissue release or excision of osteophytes. This marks our 25th case, highlighting our initial experience amid a significant learning curve. After obtaining physical fitness, the patient undergone surgery on December 08, 2023. The procedure adhered to standard robotic-assisted surgical protocols, employing kinematic alignment alongside pre- and post-cut gap assessments. Optimal balance was maintained throughout the range of motion, resulting in satisfactory patellar tracking. We utilized the Destinee Maxx-Meril cobalt-chromium-based multiradii curve femoral implant (size D), along with a titanium tibial tray (size 3) featuring an 11 mm high-flexion design polyethylene insert on both sides (Fig. 2). Intraoperative navigation confirmed satisfactory alignment, and post-operative radiographs corroborated this. The post-operative period proceeded without complications. The patient was assisted in walking with a walker 8 h after surgery. Standard post-operative protocols for antibiotic administration and deep vein thrombosis prevention were implemented. On the 5th day following surgery, the patient was discharged with detailed instructions for rehabilitation. The patient returned on the 14th post-operative day for suture removal, showing proper wound healing and no signs of infection. A check x-ray revealed satisfactory implant alignment (Fig. 3). The patient was then referred to the physiotherapy department to begin stage 2 and 3 of the rehabilitation program. There is limitation for collection of quantitative data.

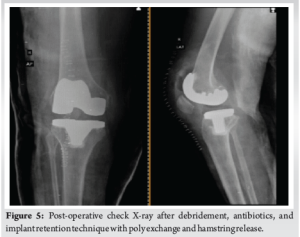
At the 3-month follow-up, the patient exhibited walking difficulties with a 10° FFD in the left knee and a urinary tract infection (UTI). She was hospitalized for supervised physiotherapy and received intravenous antibiotics. The patient was discharged after satisfactory training. Eight months post-surgery, the patient arrived at the emergency department with swelling in the right knee and FFD in both knees, which had persisted for 2 days. While the patient couldn’t recall any traumatic incident, her attendant suggested a possible bathroom slip. Radiographic examination revealed a posterior knee dislocation in the right knee (Fig 4). The medical team promptly reduced the dislocation under sedation in the operating room, using fluoroscopy guidance. Knee aspiration, performed under aseptic conditions, revealed liquefied hematoma, indicating a chronic condition. The knee was immobilized in a posterior slab. Periprosthetic infection tests were negative, and the neurological examination was inconclusive due to whole-body stiffness, hypertonia, and an uncooperative patient. The knee remained unstable, attributed to significant hamstring hypertonia. During reoperation, the surgical team observed collateral ligament laxity and hamstring tightness without signs of infection. They performed a pulse lavage wash, extensive hamstring release, and replaced the poly insert with a thicker 17 mm, following the debridement, antibiotics, and implant retention technique (Fig. 5). The infection work up did not yield any result. The left knee was manipulated and fitted with a brace to address FFD. The post-operative period was uneventful, with suture removal on the 12th day and proper wound healing. The right knee was immobilized in a brace for 6 weeks, while the left knee began mobilization with continuous passive motion and night time bracing. Physical therapy was initiated, but the patient remained uncooperative, with persistent whole-body hypertonia and reluctance to leave the bed. The patient was discharged with appropriate instructions.

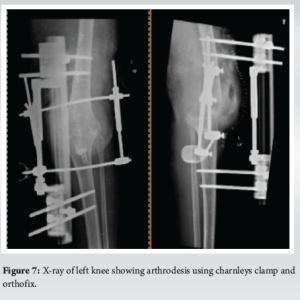
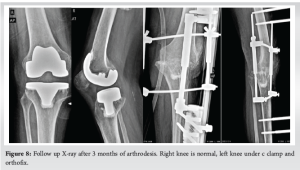
Three months after her second surgery, the patient presented with a deformity on the left side, which was diagnosed as an atraumatic posterior knee dislocation (Fig. 6). The right side was normal but stiff. Immediate reduction was performed under sedation in the operating room, followed by immobilization using an above-knee plaster slab with side support. A periprosthetic joint infection workup was conducted. The patient had a UTI due to a catheter inserted by a local physician, and her blood tests showed low hemoglobin levels of 6 g%. She was treated with intravenous antibiotics and blood transfusion. Comprehensive neurological and hormonal evaluations revealed late-onset Parkinson’s disease with Alzheimer’s traits. Follow-up X-rays indicated an unstable left knee, for which revision with a constrained implant was recommended. However, due to financial constraints and the patient’s uncooperative nature, knee arthrodesis using a Charnley clamp and Ortho fix was chosen to address the unstable left knee dislocation. During the procedure, no signs of infection were observed, but hamstring tightness was noted. The surgical team thoroughly cleaned the area with pulse lavage, removed the implant, freshened the edges, and achieved arthrodesis (Fig. 7). The infection work up did not yield result. At the 3-month follow-up, the patient had a pain-free, arthrosed left knee and a stable right knee with a range of motion from 5° to 100°, without any neuromuscular deficits (Fig. 8).

Robotic-assisted TKA is increasingly recognized for its potential advantages in precision and improved patient outcomes, making it a valuable option in orthopedic surgery. This technique enhances surgical accuracy, minimizes soft tissue damage, and leads to faster recovery times compared to traditional methods. Studies have shown that robotic-assisted TKA can significantly improve alignment and reduce complications, ultimately contributing to higher patient satisfaction and better functional results post-surgery. It is associated with a learning curve for surgical time, but not for component alignment, limb alignment, and gap balancing [1,6,7]. Sequential bilateral TKA offers several benefits, including the convenience of a single anesthesia administration, a unified surgical episode, and streamlined hospitalization and rehabilitation processes. These advantages contribute to improved patient satisfaction and efficiency in managing bilateral knee conditions. Studies have shown that performing TKA bilaterally in a single stage can lead to shorter recovery times and lower overall healthcare costs compared to staged procedures or unilateral surgeries [2,8]. However, despite these advantages, complications can still arise, some of which are rare and challenging to manage. One such complication is tibiofemoral dislocation after primary TKA. The prevalence of knee dislocation following TKA with early PS designs ranged from 1% to 2%, but this has fallen to 0.15–0.5% with newer designs that incorporate changes in the height of the tibial polyethylene post and its anterior translation [3,5]. While uncommon, this serious complication can lead to significant morbidity and is influenced by various patient-related and surgeon-related risk factors. The causes of dislocation can be classified into three categories: Patient-related factors, surgeon-related techniques, and implant designs. Patient-related factors identified in the literature include comorbidities, such as obesity, neuropsychiatric disorders, and severe preoperative deformities (varus/valgus >10°) [4,9]. Surgeon-related factors often involve technical errors, including improper ligament balancing in flexion and extension excessive soft-tissue release and malalignment issues, such as tibial implant malpositioning. In addition, a deficient extensor mechanism may contribute to instability following TKR [5]. This case report describes an unusual occurrence of bilateral knee dislocation following robotic-assisted primary knee replacement in a 65-year-old woman. Our patient had a well-functioning TKR at 8 months post-operatively and did not have any component malalignment, instability, extensor tendon dysfunction she developed complications like sequential bilateral knee dislocations. There is need for future studies to assess durability and long-term quality of life after such interventions like arthrodessis. Insall et al., reported cases of TKR dislocation due to unopposed hamstring pull following extensor malfunction or excess lateral patellar mal tracking. This has been noted in Parkinson’s disease and multiple sclerosis diagnosed patients [10]. In our patient, we presume that the cause was an unopposed hamstring pull with an intact extensor mechanism, complicated by undiagnosed neurological conditions, including late-onset Parkinson’s disease with Alzheimer’s traits. This case underscores the complex interplay between surgical outcomes, patient-specific factors, and undiagnosed comorbidities. It highlights the necessity for the routine use of validated cognitive assessment protocols for future candidates undergoing bilateral robotic TKA, especially in elderly patients with comprehensive preoperative assessments, vigilant post-operative monitoring, and adaptable management strategies in response to unexpected complications. The importance of supervised rehabilitation, especially in patients with neurocognitive impairment, is emphasized. The report aims to contribute to the literature on rare complications in robotic-assisted knee arthroplasty while providing insights into managing such challenging cases. The observations are hypothesis-generating and should be interpreted with caution.
Posterior knee dislocation is a rare complication that may arise even after robotic-assisted TKR. The occurrence of sequential bilateral dislocation is particularly uncommon and poses significant management challenges. It is vital to take patient-related factors, including neuropsychiatric disorders, into account when planning robotic TKR. A comprehensive neuropsychiatric evaluation is crucial for selecting candidates for bilateral procedures to achieve optimal outcomes and enhance patient satisfaction post-surgery.
It underscores the essential requirement for thorough neuropsychiatric evaluations in patients undergoing bilateral robotic total knee replacement to reduce the risk of rare complications, such as sequential bilateral posterior knee dislocation, which can be difficult to manage, ultimately enhancing surgical outcomes and improving patient satisfaction.
References
- 1.Mancino F, Cacciola G, Malahias MA, De Filippis R, De Marco D, Di Matteo V, et al. What are the benefits of robotic-assisted total knee arthroplasty over conventional manual total knee arthroplasty? A systematic review of comparative studies. Orthop Rev (Pavia) 2020;12:8657. [Google Scholar | PubMed]
- 2.Meehan JP, Blumenfeld TJ, White RH, Kim J, Sucher M. Risks and benefits of simultaneous bilateral total knee arthroplasty: A critical analysis review. JBJS Rev 2015;3:e3. [Google Scholar | PubMed]
- 3.Spierenburg W, Mutsaerts EL, Van Raay JJ. Dislocation after posterior stabilized primary total knee replacement: A rare complication in four cases. Case Rep Orthop 2021;2021:9935401. [Google Scholar | PubMed]
- 4.Rouquette L, Erivan R, Pereira B, Boisgard S, Descamps S, Villatte G. Tibiofemoral dislocation after primary total knee arthroplasty: A systematic review. Int Orthop 2019;43:1599-609. [Google Scholar | PubMed]
- 5.Galanis A, Papagrigorakis E, Vavourakis M, Karampinas P, Vlachos C, Patilas C, et al. Tibiofemoral dislocation after total knee arthroplasty treated successfully with an external fixation device. J Surg Case Rep 2023;2023:rjad063. [Google Scholar | PubMed]
- 6.Aneja K, Rudraraju RT, Shyam A. Robotic-assisted total knee arthroplasty: Innovations, precision, and the future of joint reconstruction. J Orthop Case Rep 2024;14:4-7. [Google Scholar | PubMed]
- 7.Vermue H, Luyckx T, Winnock de Grave P, Ryckaert A, Cools AS, Himpe N, et al. Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 2022;30:593-602. [Google Scholar | PubMed]
- 8.Agarwala S, Menon A. Safety and efficacy of sequential simultaneous bilateral total knee arthroplasty: A single centre retrospective cohort study. J Clin Orthop Trauma 2020;11(Suppl 4):S636-44. [Google Scholar | PubMed]
- 9.Jethanandani RG, Maloney WJ, Huddleston JI 3rd, Goodman SB, Amanatullah DF. Tibiofemoral dislocation after total knee arthroplasty. J Arthroplasty 2016;31:2282-5. [Google Scholar | PubMed]
- 10.Jisam PM, Jacob G, Theruvil B, Thomas AB, Varughese J. An unusual case of posterior knee dislocation following total knee arthroplasty: A case report. J Orthop Case Rep 2021;11:62-4. [Google Scholar | PubMed]