This case series presents various manifestations of acute carpal tunnel syndrome across different clinical scenarios, emphasising the need for heightened physician awareness and underscoring the importance of early diagnosis and effective treatment
Dr. Panos Christodoulou, Department of Trauma and Orthopaedics, Dr Gray’s Hospital, Elgin, United Kingdom. E-mail: panos_xristodoulos@hotmail.com
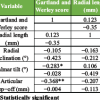
Introduction: Acute carpal tunnel syndrome (CTS) is a rare but serious condition requiring prompt diagnosis and intervention to prevent permanent neurological deficits. This case series presents our department’s experience in managing this condition, highlighting diagnostic challenges, treatment strategies, and patient outcomes.
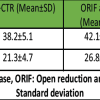
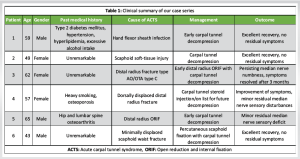
Materials & Methods: This retrospective study analyses medical records of patients diagnosed with acute carpal tunnel syndrome from 2021 to 2023 within our coverage area. Information was extracted from medical records, including diagnostic codes and clinical assessments for all cases of acute carpal tunnel syndrome, diagnosed during the period from 2021 to 2023. Data analysed, include age, sex, medical history, symptoms, mechanism of injury, clinical features, imaging, management, and follow-up. Six native Scottish patients, aged 43 to 65, developed acute carpal tunnel syndrome due to various causes, including flexor sheath infection, wrist soft tissue injury, distal radius fractures (with and without plate fixation), and scaphoid fracture.
Discussion and Results: Our case series highlights the heterogeneous presentation and aetiology of acute carpal tunnel syndrome, with causes ranging from trauma to infection. Early recognition remained challenging due to overlapping symptoms with other wrist pathologies. Surgical decompression was the mainstay of treatment, performed with variable urgency depending on clinical progression. Despite intervention outcomes were mixed. Some patients experienced full recovery while others had lingering symptoms.
Conclusion: These findings underscore the importance of high clinical suspicion and prompt surgical intervention to optimise outcomes.
Keywords: Acute carpal tunnel syndrome, diagnostic challenges, distal radius fracture, carpal tunnel decompression, neurological deficits, limited literature.
Carpal tunnel syndrome (CTS) is one of the most common and extensively studied chronic compressive neuropathies, accounting for 90% of cases. Its etiology can be linked to repetitive exposure to vibrations, forceful angular motions, genetic predisposition, injury, and conditions such as diabetes, pregnancy, and morbid obesity [1]. Symptoms primarily include pain, numbness, and paresthesias in the sensory distribution of the median nerve. Additional manifestations include hand weakness, diminished fine motor coordination, clumsiness, and atrophy of the thenar muscles, which develop gradually over months or years.
Acute CTS (ACTS), in contrast, presents with a sudden and rapidly progressive increase in pain and altered sensation in the median nerve distribution. It is uncommon and most often results from wrist or hand injuries, though atraumatic causes such as infections, inflammatory conditions, coagulopathies, malignancies, and fluid shift syndromes have been reported. The primary treatment is carpal tunnel decompression, performed either urgently or within a short – term follow up. Differentiating ACTS from less severe injuries or neuropathies is crucial and should be based on the speed of symptom onset, progression and severity [2]. Early diagnosis is essential for timely surgical intervention and to prevent permanent nerve injury.
This case series highlights a district general hospital’s experience in the management of ACTS.
Case 1
A 59-year-old male with type 2 diabetes, hypertension, dyslipidemia, and high alcohol intake presented with atraumatic flexor sheath infection. He was initially treated with intravenous antibiotics and underwent finger flexor sheath exploration and washout under general anesthesia. Intraoperatively, calcified tissue suggested chronic infection.
Postoperatively, despite improved range of motion, he experienced persistent hand and wrist pain without neurological deficits. Ultrasound revealed anterior bowing of the flexor retinaculum, indicating ACTS (Fig. 1).
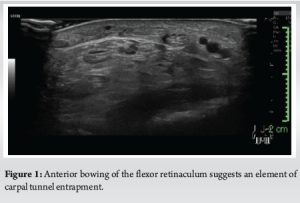
He underwent repeat washout and carpal tunnel decompression 48 h later, leading to significant symptom relief. He was discharged pain-free the next day and showed excellent recovery in follow-ups, with no residual symptoms or complications.
Case 2
This case involves a late presentation of ACTS in a 49-year-old woman referred to the fracture clinics 10 days after a right wrist injury, with no fractures identified. A highly active construction worker with well-controlled medical issues, she sustained a fall on her outstretched hand, initially developing wrist joint swelling, tenderness in the anatomic snuffbox and scaphoid tubercle, along with decreased sensation and “pins and needles” in the median nerve distribution. She had two prior assessments at other hospitals, both ruling out bony injury, and was treated with a removable wrist splint per local guidelines.
On presentation, she continued to exhibit these symptoms, prompting an urgent wrist computed tomography (CT) scan, which excluded a scaphoid fracture. She scored high on the Kamath questionnaire [3] and underwent decompression under general anesthesia without complications. The patient reported immediate improvement in median nerve sensation and complete resolution at final follow-up.
Case 3
A fit and active 62-year-old woman sustained a distal radius fracture (DRF) after a fall while roller skating. The fracture demonstrated impaction, dorsal angulation, and intra-articular involvement (AO/OTA type C). She underwent manipulation under sedation and fracture reduction in the ED, followed by the application of a backslab in a neutral position. The radiographic reduction was deemed marginally satisfactory, with no neurological or vascular deficits noted.
Following discharge, a 24-h telephone review revealed median nerve symptoms, including pain and complete numbness in her radial three digits, despite appropriate plaster application. An open reduction and internal fixation (ORIF) of the fracture, along with carpal tunnel decompression, was performed under general anesthesia 24 h after symptom onset. No complications occurred, though the median nerve was found bruised. The patient reported improved sensation within an hour postoperatively. At 2 weeks, finger and wrist mobility were nearly normal, though numbness persisted. Complete resolution occurred at 3 months.
Case 4 and case 5 (unusual ACTS following DRFs)
A 57-year-old active woman, a former heavy smoker with a history of osteoporosis, sustained a fall on slippery ice, resulting in bilateral dorsally displaced DRFs. Initial reduction and radiographic assessment confirmed acceptable fracture alignment, leading to conservative management involving casting for both fractures. During follow-up, she reported mild “pins and needles,” predominantly in the left hand. This was closely monitored, and conservative treatment continued. Upon cast removal, she demonstrated stiffness but showed good overall recovery in both hands, except for persistent “pins and needles” in the left. She was offered a diagnostic left carpal tunnel steroid injection, which resulted in a reported 60% improvement. Subsequently, she was placed on the waiting list for a semi-urgent carpal tunnel decompression.
A 65-year-old fit and active male, a self-employed floor layer with a history of right hip and lumbar spine osteoarthritis, presented to our ED after sustaining a comminuted and dorsally angulated DRF. He was initially treated conservatively, but due to fracture displacement within 2 weeks, the decision was made to proceed with an ORIF using standard volar plating. The procedure was performed under general and regional anesthesia without complications. At his 10-day post-operative follow-up, he reported altered sensation in the thenar eminence and decreased sensation in the tips of his index and middle fingers, raising suspicion of ACTS. Despite close monitoring, there was only marginal improvement. He was subsequently offered a carpal tunnel decompression under general anesthesia, which was uneventful. Following surgery, he demonstrated a significant recovery in grip strength and finger function. Although a minor residual sensory deficit remained, he expressed satisfaction with the outcome and successfully returned to work.
Case 6
A 43-year-old male, a non-smoker with no significant medical history, was involved in a head-on road traffic collision. Imaging revealed a minimally displaced (<0.5 mm) left scaphoid waist fracture, for which conservative management in a cast was chosen. At the 5-week follow-up, he reported pins and needles with numbness in the median nerve distribution. A CT scan showed <50% union of the scaphoid fracture, meeting the threshold for surgical fixation per local protocols. Carpal tunnel decompression was also indicated. Urgent surgical intervention was performed, including percutaneous scaphoid fixation and carpal tunnel decompression under general anesthesia. The procedure was uneventful, and symptoms fully resolved by the 3-month follow-up (Table 1).
Discussion
ACTS is a rare condition, with limited data on its prevalence and incidence. We conducted a retrospective study within a defined population, calculating the incidence by dividing new ACTS cases by the total population. The British Orthopaedic Association estimated an incidence of 281 CTS cases/100,000 people in 2017 [4]. Our analysis found an incidence of 1.4 new ACTS cases/100,000/year from 2021 to 2023. This highlights its rarity, underscoring the need for further research to establish a more accurate incidence rate.
While the importance of early decompression is widely acknowledged, the exact timeframe for initiating decompression remains a subject of debate. Our findings align with the consensus that early decompression is pivotal in achieving favorable outcomes in ACTS cases. Patients who underwent decompression within 48 h of symptom onset demonstrated excellent and rapid recovery within hours of the procedure. In contrast, those with delayed presentations (>3 days) experienced residual symptoms, including median nerve pain and paresthesias. However, even in delayed cases, recovery was observed within a 3-month period. Samuel et al. [2] previously suggested that decompression within 36 h of symptom onset yields excellent long-term results. Mack et al. [5] identified a sudden increase in carpal canal pressure of 40 mmHg or greater as an indication for emergent carpal tunnel release within 8 h of symptoms onset, with a delay of more than 24 h associated with less favorable long-term results. Our study adds to this body of evidence by demonstrating that decompression within 48 h can still lead to excellent recovery.
Urgent decompression of ACTS poses distinct challenges and differs from elective carpal tunnel release. Chronic CTS allows for gradual symptom adaptation, making local anesthesia feasible. However, in our ACTS cases, general anesthesia was always required due to significant pre-operative discomfort and difficulty positioning the hand. Elevated pressures in ACTS may also alter anatomy, contributing to worse outcomes. Compared to elective carpal tunnel decompression, acute carpal tunnel decompression has higher rates of residual symptoms, pain, and complex regional pain syndrome. These factors should be carefully considered during pre-operative planning and consent discussions.
Our fourth case highlights an unusual, gradual onset of ACTS, differing from typical acute presentations. Transient CTS, as described by Watanabe and Ota [6] and Pope and Tang [7], often resolves spontaneously, and symptoms do not progress over time. Close monitoring in this case is crucial for accurate diagnosis, timely intervention, and avoiding unnecessary urgent surgery.
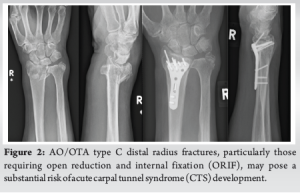
Distal radius fractures are the leading cause of ACTS. Earp et al. [8] identified open DRFs and also AO/OTA type C fractures as the main risk factors for developing the syndrome. Cooke et al. [9] reported a higher ACTS incidence in patients undergoing ORIF, likely due to high-energy trauma. Among the cases reviewed, three patients developed ACTS after surgical management of AO/OTA type C DRFs – one acute and two transient or subacute. The acute case occurred post-ORIF, suggesting a higher risk with this procedure. High-energy trauma, complete articular fractures, and open fractures appear to also increase ACTS incidence, likely due to post-operative swelling, hematoma, and biomechanical changes. This study highlights the need for vigilant monitoring and awareness of ACTS in such cases, notably in AO/OTA type C DRFs particularly those requiring an ORIF, as demonstrated by our study (Fig. 2). Finally, further research is needed to clarify the role of prophylactic carpal tunnel release, as its use in DRFs is debatable in medical literature.

Scaphoid fractures, the most common carpal fractures (2–7% of all fractures and 60–70% of carpal fractures), can lead to ACTS (Fig. 3). Olerud et al. [3] reported ACTS within 3 h of scaphoid and fifth metacarpal fractures, while Lee et al. [10] described delayed ACTS from an old displaced fracture. Monsivais and Scully [11] noted persistent CTS due to median nerve compression by the scaphoid’s distal pole. Within our population, three cases presented with ACTS following scaphoid bone injury. Early neurovascular assessment is essential for timely intervention and optimal outcomes in such cases.
ACTS requires prompt recognition and treatment. Unlike elective decompression, acute decompression differs markedly in terms of anesthesia requirements, complexity, and outcomes. Awareness of these differences is key to optimising care and preventing long-term disability, especially in patients with AO type C DRFs and scaphoid injuries.
ACTS is rare but can cause long-term dysfunction if not managed promptly. Limited literature highlights the need for research and clinical guidelines to improve outcomes, especially in high-risk patients. The authors hope that this article contributes to a more profound understanding of this condition.
References
- 1.Osiak K, Elnazir P, Walocha JA, Pasternak A. Carpal tunnel syndrome: State-of-the-art review. Folia Morphologica 2022;81:851-62. [Google Scholar | PubMed]
- 2.Samuel TD, Jeffrey H, Hayter E, Lee G, Little M, Hardman J, et al. Acute carpal tunnel syndrome: Early nerve decompression and surgical stabilization for bony wrist trauma. Plast Reconstr Surg Glob Open 2023;11:e4929. [Google Scholar | PubMed]
- 3.Olerud C, Lonnquist L. Acute carpal tunnel syndrome caused by fracture of the scaphoid and the 5th metacarpal bones. Injury 1984;16:198-9. [Google Scholar | PubMed]
- 4.British Orthopaedic Association. Commissioning Guide: Treatment of Carpal Tunnel Syndrome. London: Royal College of Surgeons; 2017. [Google Scholar | PubMed]
- 5.Mack GR, McPherson SA, Lutz RB. Acute median neuropathy after wrist trauma. The role of emergent carpal tunnel release. Clin Orthop Relat Res 1994;300:141-6. [Google Scholar | PubMed]
- 6.Watanabe K, Ota H. Carpal malalignment as a predictor of delayed carpal tunnel syndrome after colles’lles pred. Plast Reconstr Surg Glob Open 2019;7:e2165. [Google Scholar | PubMed]
- 7.Pope D, Tang P. Carpal tunnel syndrome and distal radius fractures. Hand Clin 2018;34:27-32. [Google Scholar | PubMed]
- 8.Earp BE, Mora AN, Floyd WE, Blazar PE. Predictors of acute carpal tunnel syndrome following ORIF of distal radius fractures: A matched casef acute carpdy. J Hand Surg Glob Online 2019;1:6-9. [Google Scholar | PubMed]
- 9.Cooke ME, Gu A, Wessel LE, Koo A, Osei DA, Fufa DT. Incidence of carpal tunnel syndrome after distal radius fracture. J Hand Surg Glob Online 2022;4:324-37. [Google Scholar | PubMed]
- 10.Lee DJ, Fechter J, Schnall SB. Old displaced fracture of the scaphoid. An unusual cause of carpal tunnel syndrome. Orthop Rev 1993;22:842-4. [Google Scholar | PubMed]
- 11.Monsivais JJ, Scully S. Rotary subluxation of the scaphoid resulting in persistent carpal tunnel syndrome. J Hand Surg 1992;17:642-4. [Google Scholar | PubMed]