Keratinous cysts, the most common type of epidermal cyst, are keratin-filled lesions that originate from the epidermis, typically arising from a hair follicle. This case highlights an uncommon presentation of a keratinous epidermal cyst within the third metatarsal bone, which caused significant pain, swelling, and impaired mobility. Surgical excision combined with curettage proved to be an effective treatment approach.
Dr. R V Raghav, Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: raghavravi2193@gmail.com
Introduction: Keratinous cysts are benign lesions that primarily affect the skin but can occasionally involve bones, presenting a diagnostic challenge due to their rarity and varied manifestations.
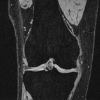
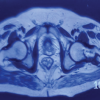
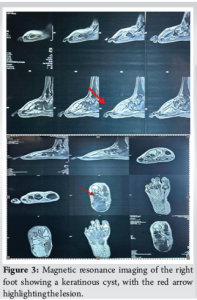
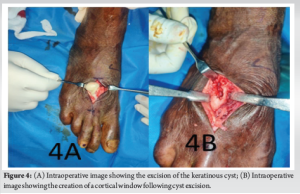
Case Report: We present a case of a 65-year-old male farmer who presented with swelling and persistent pain in the right foot, particularly over the third toe. The patient had a history of trivial trauma and previous incision and drainage for a foot swelling. Radiographic and magnetic resonance imaging findings indicated a well-defined lytic lesion with cortical thinning and breach over the third metatarsal, raising suspicion for tuberculous osteomyelitis. Surgical exploration revealed an encapsulated cyst filled with cheesy material. No sequestrated bone or osteomyelitis was found.
Conclusion: The cyst was excised, and the affected bone underwent curettage. Histopathological examination confirmed the diagnosis of a keratinous cyst with no evidence of granuloma or malignancy. Postoperatively, the patient experienced an uneventful recovery, undergoing immobilization and later non-weight-bearing mobilization. This case highlights the importance of considering non-infective causes, such as keratinous cysts, when evaluating bone lesions with lytic characteristics, especially in the presence of a history of trauma or previous interventions. Prompt surgical intervention and histopathological examination are critical for accurate diagnosis and management.
Keywords: Keratinous cyst, bone lesion, metatarsal, histopathology, osteomyelitis.
Keratinous cysts, also known as epidermoid cysts, are benign, slow-growing lesions that arise from the epidermal or follicular cells. Typically, these cysts form as a result of the abnormal proliferation of keratin-producing cells, leading to the accumulation of keratin in a sac-like structure. They are most commonly found in the skin, but in rare cases, they can affect deeper tissues, including bone. The involvement of bone by a keratinous cyst is an unusual and infrequent presentation, often leading to diagnostic challenges due to its rarity and similarity to other conditions such as infections, tumors, or even cystic bone lesions [1]. Keratinous cysts are generally asymptomatic when located in the skin, often presenting as small, painless lumps. However, when located in deeper structures such as bones, they may cause symptoms such as swelling, pain, or tenderness, which can be mistaken for other, more common conditions. The clinical presentation of these cysts is often nonspecific, making it essential to differentiate them from more common conditions such as osteomyelitis, benign tumors, or metastatic lesions [2]. The diagnosis is typically confirmed through a combination of radiologic imaging and histopathological examination, with surgical intervention providing the most definitive approach for management [3]. The foot, particularly the metatarsal bones, is a rare site for the development of a keratinous cyst. In most cases, bone involvement is secondary to trauma, which may lead to the formation of a cyst-like structure as a result of the body’s healing process [4]. Other risk factors that have been associated with keratinous cysts include chronic inflammation, infection, or developmental anomalies. This case report describes a 65-year-old male farmer who presented with an unusual presentation of a keratinous cyst in the third metatarsal of the right foot, which was initially misdiagnosed as an infectious lesion [5]. In this particular case, the patient experienced swelling and pain over the right foot, which persisted despite antibiotic and analgesic treatment. The patient had a history of trivial trauma to the foot and a previous episode of swelling for which an incision and drainage procedure had been performed. His radiographic and magnetic resonance imaging (MRI) findings revealed a lytic lesion with cortical thinning over the third metatarsal, which suggested the possibility of an infective process, such as tuberculous osteomyelitis [6]. These findings highlight the challenge clinicians face when attempting to differentiate keratinous cysts from other conditions that can cause bone destruction and soft-tissue involvement. Epidemiologically, keratinous cysts are more commonly found in younger individuals, but they can also affect older patients, often presenting with complications due to delayed diagnosis or chronicity. When they do occur in the bone, these cysts can cause cortical thinning and lytic changes, which may mimic the appearance of a neoplastic or infectious process. Although a diagnosis of osteomyelitis or a tumor is typically suspected when there is bone involvement, keratinous cysts can often present in a similar fashion, leading to confusion and delays in the correct diagnosis [7]. Imaging techniques such as X-rays and MRI are crucial in the diagnostic workup of bone lesions. X-ray imaging can reveal characteristic lytic changes, such as cortical thinning, loss of the bone cortex, or the presence of a radiolucent area, which may suggest a benign lesion. MRI can provide more detailed information, showing the exact extent of bone involvement and whether there is soft-tissue extension, which is often a key feature in identifying cystic lesions [8]. In cases of suspected infection, MRI can also help differentiate between an abscess and a cyst by identifying fluid-filled spaces within the lesion. Histopathological examination remains the gold standard for diagnosing keratinous cysts. The cyst is typically lined by stratified squamous epithelium, with a granular layer filled with keratinous material. The presence of histiocytes and giant cells in the surrounding tissues can also be observed, but there are usually no features indicative of malignancy or granuloma formation. This case emphasizes the importance of histopathology in confirming the diagnosis and ruling out other conditions, such as infections or neoplasms [8]. The aim of this case report is to present an unusual presentation of a keratinous cyst in the right foot, focusing on the diagnostic challenges posed by its bone involvement and the importance of surgical intervention and histopathological examination in confirming the diagnosis. By discussing this rare case, we hope to raise awareness of the possibility of keratinous cysts presenting as lytic bone lesions and to highlight the need for a comprehensive approach to diagnosing bone lesions, particularly when there is a history of trauma or prior interventions.
A 65-year-old male farmer presented to the outpatient department with complaints of swelling and persistent pain in the right foot, particularly over the third toe. The patient had been experiencing localized swelling and pain for the past 4–6 weeks, which did not subside despite treatment with antibiotics and analgesics prescribed by his local practitioner. The patient, a farmer by profession, lives with his spouse in a rural setting. His occupation, which involves significant physical activity, including walking, standing, and heavy lifting, likely contributed to the stress on his feet. He has no significant history of smoking or alcohol use. The patient reported a prior history of minor trauma to the right foot 5 years ago, which was managed conservatively with no long-term complications. Two years ago, the patient experienced similar swelling in the same foot, for which an incision and drainage procedure was performed at an outside hospital. Still, there were no subsequent issues after the procedure. At the time of presentation, the patient denied any systemic symptoms such as fever, weight loss, or malaise. He also reported no history of chronic conditions like diabetes, hypertension, or autoimmune disorders. The patient was not taking any long-term medications except for those prescribed for pain and swelling during the current episode. He had no prior history of significant illnesses or surgeries other than the previous minor trauma and surgical intervention on his right foot (Fig. 1-7).
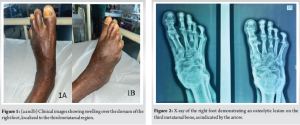
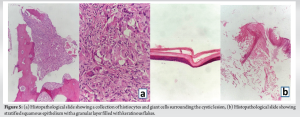


A 65-year-old male farmer presented with localized swelling and persistent pain in the right foot, particularly over the third toe, which had been ongoing for 4–6 weeks and failed to resolve with antibiotics and analgesics. The patient had a history of minor trauma to the foot 5 years prior and a previous surgical intervention for similar swelling 2 years ago. This case shares similarities with other studies of keratinous cysts, particularly in terms of the cyst’s association with trauma and physical activity. For instance, a 71-year-old woman with rheumatoid arthritis developed a plantar epidermoid cyst that was initially mistaken for callosities but was later diagnosed through imaging and excised [9]. Likewise, a 29-year-old woman with a hybrid cyst on the sole, thought to arise from trauma, also had a lesion on the foot, reinforcing the connection between mechanical stress and the formation of these cysts [10]. In addition, a case of a keratinous cyst in the parotid region of a 52-year-old male was linked to prior trauma, further supporting the role of trauma in the development of epidermal cysts [11]. Similarly, a 53-year-old female with a subungual epidermoid cyst that developed after a previous trauma to the finger highlights the recurring theme of cyst formation post-trauma [12]. These cases, like the current one, emphasize the importance of considering keratinous cysts in individuals with a history of trauma and mechanical strain, particularly when swelling persists despite initial conservative treatments. A keratinous cyst of the metatarsal represents an exceedingly rare clinical entity, with keratinous (epidermoid) cysts themselves being infrequently encountered in the bones of the foot, particularly the metatarsal region. These cysts typically arise in cutaneous or subcutaneous locations and are most commonly observed on the face, neck, scalp, and trunk, with plantar or metatarsal involvement being exceptional. The clinical presentation can mimic infectious, tubercular, or neoplastic processes, often leading to diagnostic uncertainty, especially when associated with signs of inflammation or atypical imaging findings. In the presented case, the differential diagnosis included infection and neoplastic etiologies, highlighting the importance of thorough evaluation. Definitive diagnosis hinges on histopathological examination, which reveals a cystic cavity lined by stratified squamous epithelium containing lamellated keratin, distinguishing it from other possible lesions and confirming its benign nature. The rarity of keratinous cysts in the metatarsal underscores the significance of this case, as such localization is scarcely reported in the literature, making it a noteworthy contribution to the understanding of unusual presentations of keratinous cysts. This case emphasizes the necessity of considering keratinous cysts in the differential diagnosis of metatarsal lesions and the crucial role of histopathology in establishing a precise diagnosis.
This case highlights an unusual presentation of a keratinous cyst involving the third metatarsal bone, which mimicked the appearance of an infective or neoplastic bone lesion. The case underscores the importance of considering a wide differential diagnosis when evaluating bone lesions and the role of surgical exploration and histopathological examination in confirming the diagnosis.
Unusual intraosseous presentations of keratinous cysts should be considered in the differential diagnosis of lytic bone lesions associated with pain and swelling. Early diagnosis and surgical intervention can lead to excellent functional recovery.
References
- 1.Huo CW, Caputo C, Wang YY. Suprasellar keratinous cyst: A case report and review on its radiological features and treatment outcome. Surg Neurol Int 2018;9:15. [Google Scholar | PubMed]
- 2.Goulart MC, Freitas-Faria P, Goulart GR, Oliveira AM, Carlos-Bregni R, Soares CT, et al. Pleomorphic adenoma with extensive squamous metaplasia and keratin cyst formations in minor salivary gland: A case report. J Appl Oral Sci 2011;19:182-8. [Google Scholar | PubMed]
- 3.Sabhlok S, Kalele K, Phirange A, Kheur S. Congenital giant keratinous cyst mimicking lipoma: Case report and review. Indian J Dermatol 2015;60:637. [Google Scholar | PubMed]
- 4.Faltaous AA, Leigh EC, Ray P, Wolbert TT. A rare transformation of epidermoid cyst into squamous cell carcinoma: A case report with literature review. Am J Case Rep 2019;20:1141. [Google Scholar | PubMed]
- 5.Zhang ZD, Li X, Li M, Zhao J, Zhou KJ, Qu J. Clinicopathological features and surgical treatment of intratarsal keratinous cysts. Am J Dermatopathol 2013;35:78-82. [Google Scholar | PubMed]
- 6.Bothra N, Mishra D, Ali MJ. Atypical presentation of punctal keratin cyst: An underdiagnosed entity. Orbit 2023;42:431-3. [Google Scholar | PubMed]
- 7.McGavran MH, Binnington B. Keratinous cysts of the skin. Identification and differentiation of pilar cysts from epidermal cysts. Arch Dermatol 1966;94:499-508. [Google Scholar | PubMed]
- 8.Jakobiec FA, Stagner AM, Freitag SK, Yoon MK. Unusual eyelid dermal keratinous cysts of pilosebaceous origin. Ophthalmic Plast Reconstr Surg 2016;32:93-7. [Google Scholar | PubMed]
- 9.Yamanaka H, Tamai H, Suzuki M, Kobayashi T, Eguchi Y. Plantar epidermoid cyst in a patient with rheumatoid arthritis. J Clin Diagn Res 2018;10:555785. [Google Scholar | PubMed]
- 10.Lee JH, Jung H, Kim G, Kim S. Hybrid cyst on the sole. J Dermatol 2012;39:41-6. [Google Scholar | PubMed]
- 11.Sudhagar S, Bhatia K, Kumar M. Keratinous cyst of external auditory canal masquerading as parotid lesion: A clinical dilemma. J Ear Nose Throat Disord 2020;5:1041. [Google Scholar | PubMed]
- 12.Molloy D, Herbert K. Subungual epidermoid cyst. J Hand Surg Br Eur 2006;31:345-5. [Google Scholar | PubMed]