Diagnosing chronic recurrent multifocal osteomyelitis [CRMO], a rare benign bone lesion with non-specific features, is a diagnosis of exclusion requiring comprehensive evaluation and multidisciplinary discussion to guide appropriate, often conservative management and long-term monitoring for potential complications.
Dr. Mohammed Tavfiq, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai - 600116, Tamil Nadu, India. E-mail: tavfiqmm@gmail.com
Introduction: Chronic recurrent multifocal osteomyelitis (CRMO) is a benign, noninfectious, self-limiting inflammatory bone disease that predominantly affects children and adolescents, characterized by multiple, recurrent osteolytic and sclerotic lesions typically involving the metaphysis of long tubular bones, clavicle, spine, and pelvic. The clavicle, particularly its medial end, is the most common and characteristic site affected.
Case Report: A 13-year-old boy presented with a 5-month history of acute gradually progressive, dull aching pain over the bilateral hip radiating to the thigh, knee, and ankle. Myeloproliferative disorders were ruled out with a bone marrow biopsy. Magnetic resonance imaging pelvis with hip, thigh, and clavicle screening showed altered signal intensities involving the bilateral acetabulum, pubic bones, iliac bone, right femur, bilateral tibia, and clavicle, along with diffuse periosteal thickening involving the left iliac wing. After ruling out all possible differential diagnosis and discussion in a multidisciplinary team, a final diagnosis of CRMO was made. The patient was started on Inj. Pamidronate and responded well to treatment.
Conclusion: CRMO is a rare benign bone lesion with diverse clinical presentation and lack of specific clinical, laboratory, or pathological features, which leads to misdiagnosis or delayed diagnosis. A high index of suspicion and characteristic radiological involvement of the clavicle may help to clinch the diagnosis. Familiarity with this condition greatly increases the likelihood of early diagnosis and appropriate management.
Keywords: Chronic recurrent multifocal osteomyelitis, clavicle, inflammatory.
Chronic recurrent multifocal osteomyelitis (CRMO) is a benign, noninfectious, self-limiting inflammatory bone disease that predominantly affects children and adolescents. It was first reported by Giedion et al. in 1972 [1,2]. CRMO is characterized by multiple, recurrent osteolytic and sclerotic lesions typically involving the metaphysis of long tubular bones, clavicle, spine, pelvis, and mandible [3]. The most common symptoms include multiple joint pains, on-and-off swelling, redness, and fever. It can also be associated with other conditions such as psoriasis, palmoplantar pustulosis (8%), inflammatory bowel diseases (10%), and severe acne (10%) [2]. Investigations include total blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor (RF), antinuclear antibody, and human leucocyte antigen-B27 (HLA B27). Radiological investigations, such as X-ray, are usually normal, and magnetic resonance imaging (MRI) shows marrow edema at multiple sites. Due to the lack of typical symptoms or definitive laboratory tests, CRMO is often misdiagnosed or diagnosed late. Diagnosis is based on Jansson et al. criteria [1,4]. Treatment is based on the symptoms, and non-steroidal anti-inflammatory drugs (NSAIDs) are given as first-line drugs. Counseling of parents is important due to the nature of on-and-off disease. Corticosteroids play an important role in reducing inflammation and edema in bone. We report a case of 13-year-old boy who presented with multiple joint pains. Blood cultures were negative. Bone marrow biopsy showed no evidence of malignancy. MRI revealed bone marrow edema in the pelvis, bilateral tibia, and clavicle characteristic of CRMO.
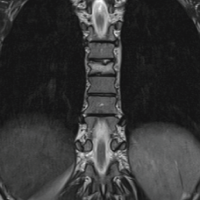
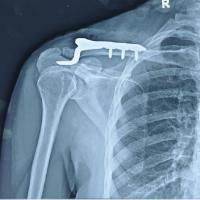
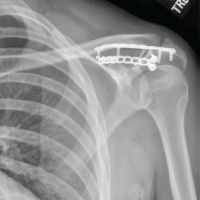
A 13-year-old boy presented to the outpatient department with a 5-month history of bilateral knee, hip and ankle pain. The pain was predominantly over the hips and radiating to the thighs. Pain was acute in onset, gradually progressive, and described as a dull ache and relieved by medication. No constitutional symptoms were present, and he was able to do his daily activities. His birth history, developmental milestones, and immunization records were normal. His older sister had a history of Juvenile Idiopathic oligoarthritis. His clinical examination was normal. Laboratory investigations such as ESR (46 mm/h), CRP (0.9), uric acid (5.1 mg/dL) were normal, and the Mantoux test was negative. HLA B27 and RF test were also negative. Blood culture showed no growth. His X-ray radiographs were normal. MRI pelvis with hip, thigh, and clavicle screening was done (Fig. 1-7), which showed altered signal intensities involving the bilateral acetabulum, pubic bones, iliac bone, right femur, bilateral tibia, and clavicle, along with diffuse periosteal thickening involving the left iliac wing. Bone marrow biopsy was also done to rule out any hematological malignancy – showed trilineage hematopoiesis with erythroid hyperplasia. No blast cells were noted.


A multidisciplinary team discussion was held during which the collective input from orthopedics, radiology, pediatric rheumatology, and pediatric oncology concluded that all the features were suggestive and supportive to the diagnosis of CRMO. We started the patient on injection pamidronate 40 mg once daily (2 doses). Supportive measures, including appropriate analgesia and nutritional optimization, were maintained. The patient responded well to the treatment. His pain reduced, and he showed symptomatic improvement.
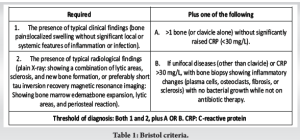
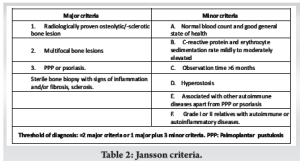
CRMO is a recurrent autoinflammatory nonbacterial osteomyelitis characterized by lytic, sclerotic and hyperostotic bone lesions [3]. Despite the chronicity character, CRMO often exhibits periodic flares and phases of remission. It often affects children and adolescents, with a female-to-male ratio of 2:1 [5]. The pathogenesis of CRMO remains unclear and may be linked to an imbalance between pro-inflammatory cytokines (Interleukin [IL]-6, IL-1, tumor necrosis factor alpha) and anti-inflammatory cytokines (IL-10). These cytokines are involved in bone resumption and remodeling through osteoblasts and osteoclasts activation [5]. A consistent feature of CRMO is the gradual onset of pain, accompanied by swelling and tenderness over the affected bones. Patients commonly present in many clinical forms, from unifocal or multifocal lesions with a relapsing and remitting course. Symptoms include fever, pain, swelling, and a limited range of motion in the affected region [6]. Metaphysis of long tubular bones such as the femur, tibia, clavicula are commonly affected, followed by the spine and pelvis. Clavicle, mandible, and sternum are the typically affected sites [7]. The clavicle and mandible are the classical locations of involvement. It is the most common disease to affect the medial end of the clavicle, similar to our case. Nevertheless, a unifocal unusual location in the absence of trauma should prompt suspicion for CRMO [4,8]. A subset of patients also present with comorbidities affecting other systems, including the skin, gastrointestinal tract or joints [9]. Radiological findings are nonspecific. Plain radiographs are frequently unremarkable. On MRI, active disease shows oedematous marrow changes [8,10]. Active disease in the clavicle is characterized by lytic destruction of the medullary bone in the medial aspect. A lamellated periosteal reaction is often seen, although sequestra are not formed. At this stage, MRI typically reveals a mass involving the clavicular marrow, cortex, and periosteal new bone formation. MRI shows homogeneous T1 hypointense and T2 hyperintense images [8]. The role of biopsy is controversial since histological features are nonspecific but it may help to exclude infectious osteomyelitis and malignant bone tumors [11]. An accurate diagnosis is often challenging due to a lack of specific clinical findings, laboratory tests, and radiology. Therefore, CRMO remains a diagnosis of exclusion [12]. Two diagnostic criteria, the Jansson criteria and Bristol criteria, have been proposed (Tables 1 and 2). The clavicle is an unusual location for infectious osteomyelitis and is therefore very specific for inflammatory lesions, such that unifocal clavicular lesions are considered positive in the Bristol criteria [3].
There are no consensus recommendations for the treatment of CROM. Non-steroidal anti-inflammatory drugs are given as the first-line drugs in therapeutic management to control pain and prevent bone damage. Corticosteroids are used in patients who are resistant to NSAIDs. Methotrexate represents a second-line treatment. Sulfasalazine is generally used in patients with associated inflammatory bowel disease [12]. Bisphosphonates are effective and well-tolerated. In children, pamidronate is the bisphosphonate of choice [5]. Most cases follow a benign, protracted course. An early diagnosis can avoid unnecessary over treatment. Taylor et al. [3] in their study on retrospective review of 80 patients with CRMO observed that 74% of their total cohort had residual symptoms. 48% had complaints of recurrent pain, 4% had vertebral flattening/height loss, 2.5% had bone deformity, and 2.5% had immobility. Duffy et al. [13] observed in their follow-up study of 8 cases with CRMO that only two patients experienced complete resolution. Five had leg-length inequality of at least 1.5 cm. Among these, one patient experienced a significant 5.5 cm shortening and subsequently underwent a leg-lengthening procedure. Seven patients had noticeable deformity. This underscores that CRMO needs to be followed up to maturity since it can have disabling sequelae.
CRMO is a rare benign bone lesion and essentially a diagnosis of exclusion due to a lack of specific symptoms and nonspecific laboratory and radiological features. A detailed history, thorough clinical examination, and rational investigations are required. Furthermore, a multidisciplinary discussion is a must. As the disease is self-limiting, knowledge of its characteristic appearance can lead to the most appropriate treatment and can prevent aggressive medical and surgical evaluation and treatment. Some cases can have significant residual deformity, including wasting and shortening of affected limbs. Hence, patients should be followed up till maturity.
Diagnosing challenging CRMO, a condition requiring exclusion of other causes, benefits from symptomatic treatment, with injectable pamidronate playing a significant role.
References
- 1.Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV. Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis. Pediatr Rheumatol Online J 2016;14:47. [Google Scholar | PubMed]
- 2.Giedion A, Holthusen W, Masel LF, Vischer D. Subacute and chronic “symmetrical” osteomyelitis. Ann Radiol (Paris) 1972;15:329-42. [Google Scholar | PubMed]
- 3.Taylor TN, Bridges CS, Ezeokoli EU, Smith TS, Montgomery NI. Retrospective review of 80 patients with chronic recurrent multifocal osteomyelitis evaluated by pediatric orthopaedic surgeons. J Pediatr Orthop Soc N Am 2023;5:575. [Google Scholar | PubMed]
- 4.Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A, et al. Classification of non-bacterial osteitis: Retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatol Oxf Engl 2007;46:154-60. [Google Scholar | PubMed]
- 5.Sergi CM, Miller E, Demellawy DE, Shen F, Zhang M. Chronic recurrent multifocal osteomyelitis. A narrative and pictorial review. Front Immunol 2022;13:959575. [Google Scholar | PubMed]
- 6.Chronic Recurrent Multifocal Osteomyelitis: A Multidisciplinary Experience of 22 Pediatric Cases with a Mean Follow-Up of 27 Months - ClinicalKey. Available from: https://www.clinicalkey.com/#!/content/journal/1-s2.0-S0949265821003742 [Last accessed on 2025 Mar 04]. [Google Scholar | PubMed]
- 7.Himuro H, Kurata S, Nagata S, Sumi A, Tsubaki F, Matsuda A, et al. Imaging features in patients with SAPHO/CRMO: A pictorial review. Jpn J Radiol 2020;38:622-9. [Google Scholar | PubMed]
- 8.Iyer RS, Thapa MM, Chew FS. Chronic recurrent multifocal osteomyelitis: Review. AJR Am J Roentgenol 2011;196 Suppl 6:S87-91. [Google Scholar | PubMed]
- 9.Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlöhner S, et al. Chronic nonbacterial osteomyelitis in childhood: Prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther 2010;12:R74. [Google Scholar | PubMed]
- 10.Fritz J, Tzaribatchev N, Claussen CD, Carrino JA, Horger MS. Chronic recurrent multifocal osteomyelitis: Comparison of whole-body MR imaging with radiography and correlation with clinical and laboratory data. Radiology 2009;252:842-51. [Google Scholar | PubMed]
- 11.Kamoun K, Arfa W, Chaalia MB, Oueslati W, Abid L, Jenzri M. Chronic recurrent multifocal osteomyelitis of clavicle: A rare isolated location (a case report). Pan Afr Med J 2023;46:53. [Google Scholar | PubMed]
- 12.Liu L, Zhang R, Nie N, Wang D, Lin Y, Gao Z, et al. Chronic recurrent multifocal osteomyelitis: Case report and review of the literature. Medicine (Baltimore) 2024;103:e38850. [Google Scholar | PubMed]
- 13.Duffy CM, Lam PY, Ditchfield M, Allen R, Graham HK. Chronic recurrent multifocal osteomyelitis: Review of orthopaedic complications at maturity. J Pediatr Orthop 2002;22:501-5 [Google Scholar | PubMed]