Cryptococcosis should be considered as a rare differential diagnosis in patients presenting with bone pain and multiple lytic lesions.
Dr. Prannoy Paul, Department of Orthopaedics, M.O.S.C Medical College Hospital, Ernakulam, Kerala, India. E-mail: prannoypaul@gmail.com
Introduction: Cryptococcus is a rare cause of osteomyelitis, especially in immunocompromised individuals. This case report discusses a rare case of disseminated cryptococcosis with multiple bone lesions in a patient with isolated CD4 lymphocytopenia.
Case Report: A 31-year-old apparently normal Indian male presented with pain and swelling of his right proximal femur for 8 months without any history of trauma. He also reported a similar swelling in his chest wall with allergic respiratory symptoms for 8 years. Laboratory analysis revealed mild elevation in inflammatory markers. Magnetic resonance imaging of the pelvis revealed osteolytic lesions in the right proximal femur and pubic bone with soft tissue collections, and computed tomography scan of the chest showed an osteolytic lesion in the right 9th rib with an overlying soft tissue collection and a subpleural cavitary nodule in the left lower lobe posterior basal segment. Although initially treated as a case of clinically diagnosed tuberculosis, the patient did not get any relief with antitubercular therapy. Fine needle aspiration cytology and fungal culture identified Cryptococcus neoformans from both lesions and from the blood culture. The patient responded well to antifungal treatment and is currently symptom free.
Conclusion: Cryptococcosis should be considered as a rare differential diagnosis in patients presenting with bone pain and multiple lytic lesions. Definitive diagnosis requires a fungal culture from the affected areas. Early treatment with antifungals is important in preventing complications and death.
Keywords: Cryptococcus neoformans, cryptococcal osteomyelitis, cryptococcosis, osteomyelitis.
Cryptococcus is a recognized fungal pathogen which predominantly infects immunocompromised individuals, especially those infected with human immunodeficiency virus (HIV), recipients of organ transplants, and those with malignancies [1]. Although immunocompromised individuals are the most affected by cryptococcosis, incidents of such infections in immunocompetent individuals have also been reported in the literature [2]. More than 95% of cryptococcal infections are caused by Cryptococcus neoformans, whereas a small proportion of cases are caused by Cryptococcus gattii, especially in immunocompetent hosts [1,3]. Birds are the usual carriers of Cryptococcus and the pathogen is commonly isolated from bird droppings and from contaminated soil [4]. Cryptococcus usually infects through the respiratory route, resulting in respiratory complications, and also has an affinity to the central nervous system [5]. Although the respiratory system and the central nervous system are the primary targets of Cryptococcus, infections of the skeletal system are also reported in about 10% cases of disseminated cryptococcosis [6]. This report describes a rare case of disseminated cryptococcosis infecting multiple bones and the respiratory system in a patient with idiopathic isolated CD4 lymphocytopenia.
A 31-year-old male, a tailor by profession, presented with pain and swelling of his right upper thigh for 8 months. The swelling was insidious in onset, gradually increasing in size over the past 8 months. He was prescribed analgesics from a local clinic, which only gave temporary relief. He also reported difficulty in walking due to the pain. The patient also complained of a similar tender swelling in the back of right lower chest wall for 2 months. He complained of allergic respiratory symptoms since 2015, for which he was on an intermittent metered dose inhaler (MDI). He had an occasional cough with scanty mucoid sputum. There was a history of on-and-off fever, which was more toward evening. He also reported weight loss and loss of appetite in the recent past. He had a category A COVID-19 infection in 2021. Initial differential diagnoses were tuberculosis (TB), malignancy, or osteomyelitis. Blood investigations revealed normal total white blood cell counts, with a raised erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) (Table 1). Investigations also ruled out a malignancy with normal prostate-specific antigen, carcinoembryonic antigen, and carbohydrate antigen 19-9 and imaging was negative.
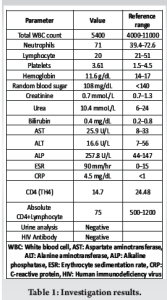
On evaluation of the swelling of the proximal thigh, X-ray of the pelvis with hip revealed a lytic lesion in the right proximal femur (Fig. 1). Further imaging with magnetic resonance imaging (MRI) revealed lytic lesions in right proximal femur and right pubic bone, with a heterogeneous hypoechoic collection in the thigh extending into the femur (Fig. 2). X-ray of the chest revealed a lytic lesion in the right 9th rib (Fig. 3). A computed tomography (CT) scan of the thorax revealed an expansile lytic lesion in 9th rib on the right side with a soft tissue collection, along with a subpleural cavitary nodule in the left lower lobe posterior basal segment. Routine sputum culture yielded no growth. Sputum acid-fast staining and culture for TB were also negative. He was hence diagnosed as a case of clinically diagnosed TB and was started on anti-tubercular therapy from elsewhere. However, even after 2 months of anti-tubercular therapy, the patient reported no improvement in symptoms and presented to our hospital.
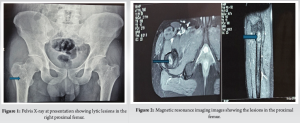
On repeat imaging, the lesions in the proximal thigh and the chest wall were noted to have increased in size. Repeat blood investigations yielded a similar picture and repeat culture of the sputum with investigations for TB with acid-fast staining, culture, cartridge-based nucleic acid amplification test, and QuantiFERON gold TB test were negative and ruled out a tuberculous infection. We aspirated fluid from the soft tissue lesion in the right proximal femur and the right posterior chest wall for analysis, with a fine-needle aspiration cytology (FNAC) of the affected rib, cytology, extended culture for atypical organisms, and a fungal culture were sent. Although other investigations were unyielding, the fungal culture from the thigh swelling turned out to be positive for C. neoformans. A fungal culture from the collection on the chest wall and a blood culture also yielded C. neoformans. Cerebrospinal fluid (CSF) cultures were negative. Further, as Cryptococcus usually occurs in those exposed to birds, further questioning revealed exposure to pigeons at his home. Hence, he was diagnosed as a case of disseminated cryptococcosis and was started on lipophilic amphotericin B and fluconazole with serial monitoring of renal parameters. The anti-tubercular therapy was stopped. Amphotericin B was given at a dose of 0.8 mg/kg infusion over 2–4 h in 5% dextrose daily and oral fluconazole 400 mg once daily was given for 1 month. The patient became symptomatically better, and his general condition improved significantly. After 1 month of intravenous therapy, he was started on the consolidation phase with oral fluconazole 400 mg once daily for a total 8 weeks, followed by the maintenance phase with fluconazole 200 mg once daily. As cryptococcosis occurs predominantly in immunocompromised individuals, and as his HIV enzyme-linked immunosorbent assay was negative, further search into immunodeficiency was done. A clinical exome sequencing, lymphocyte subset analysis, immunoglobin profile, native T cell assay and a nitroblue tetrazolium test for immune function. The results revealed an isolated CD4 lymphocytopenia with a CD4 count of 75 (<14%) (Table 1). As he is also at risk of infection with Pneumocystis jirovecii pneumonia due to his immunodeficiency, he was also started on trimethoprim-sulfamethoxazole prophylaxis. The patient is currently at 1-year follow-up. A repeat MRI of the pelvis revealed consolidation of the lesion in the proximal femur and pubic bone. CT of the thorax revealed complete resolution of the lesions in the chest. Chest X-ray (Fig. 4) and X-ray pelvis (Fig. 5) at 1-year follow-up revealed consolidation of the lytic lesions. ESR and CRP have also stayed consistently normalized at 1-year follow-up, and the patient has been symptom free after discharge.
Cryptococcosis is a fungal infection affecting immunocompromised individual worldwide. It primarily affects individual with HIV, recipients of organ transplantation, and can potentially turn fatal [1]. Cryptococcal infection typically occurs through the respiratory route, resulting in a pneumonia or meningitis [7]. Cryptococcus forms phagosomes and “titan cells” to prevent phagocytosis and evades the immune system [8]. Cryptococcal infections of the bone are rare, though it can possibly occur through a spread from the bloodstream or through direct inoculation from soil in an open wound [9,10]. Our patient reported respiratory allergic symptoms since 2015 and an exposure to pigeons at his home, for which he was on symptomatic treatment with an MDI. 8 years later, he developed widespread bone pain and a new onset of on-and-off fever. He had no history of previous serious respiratory infections. This could suggest that the primary focus could be the lung with a bloodstream spread to the right proximal femur and pubic bone. CT thorax revealed an expansile lytic lesion in the 9th rib on the right side with soft tissue component. Blood culture as well as cultures from the lesions in the chest and in the femur were positive for Cryptococcus. Although rare instances of cryptococcal infections have been reported in immunocompetent hosts [2], the majority of cryptococcal infections occur in immunocompromised hosts. The infections in immunocompetent hosts are more frequently caused by C. gattii and are associated with smoking [3]. Bone infections by Cryptococcus are commonly caused by C. neoformans and typically affect immunocompromised individuals [2]. Patients usually affected include those with HIV, particularly those with a CD4 cell count <100, transplant recipient patients, those with chronic steroid use, or those with hematological malignancies [11-13]. Our patient had no identifiable risk factors for immunodeficiency. The patient had no history of diabetes or organ transplantation. Workup for malignancies was negative, and serology was negative for HIV. He did not have a history of steroid intake or treatment with any immunomodulator. However, on further immunological evaluation, he was identified to have an isolated deficiency of CD4 lymphocytes. In this individual, CD4 cell count was found to be 75 (14.7%), without any other associated abnormality, and he was diagnosed as a case of isolated CD4 lymphocytopenia. The clinical presentation and radiological appearance of skeletal cryptococcosis can often mimic metastatic malignancy as skeletal cryptococcosis lacks any typical radiological features [10]. In our case, all tests for malignancy were negative and FNAC of the lesions with a fungal culture helped in diagnosing the infection. Once diagnosed, cryptococcosis is usually treated with systemic therapy, with surgery indicated only in few cases to decrease the infective load or in cases of meningeal involvement [11]. In our patient, the CSF studies and imaging were negative for any cranial involvement. Amphotericin B is the mainstay of treatment of cryptococcosis, with better results also reported with combination chemotherapy with amphotericin and fluconazole [12]. In patients presenting with bone pain and multiple osteolytic lesions, skeletal cryptococcosis should be included as one of the differential diagnoses, especially when the host is suspected to be immunocompromised. Further, conditions like isolated CD4 lymphocytopenia could be rare causes. Idiopathic CD4 lymphocytopenia is defined by the Centers for Disease Control as an unexplained deficiency of circulating CD4 cells below 300 cells/mm3 in the absence of HIV or other immunodeficiencies or treatments that might lead to a decrease in CD4 count, leading to opportunistic infections [14]. Causes for this puzzling syndrome still remain unclear, and treatment mainly involves treating and preventing opportunistic infections [15].
As advanced investigations are required to diagnose some immune deficiencies, high suspicion is needed to detect such rare causes of osteomyelitis. Even in immunocompetent hosts presenting with bone pain and osteolytic lesions, cryptococcal osteomyelitis should be included in the differential diagnosis and investigated with FNAC, fungal cultures, and further immunological assessments.
Cryptococcosis is a rare differential diagnosis in patients presenting with multiple lytic bone lesions and respiratory symptoms, especially in immunocompromised.
References
- 1.Maziarz EK, Perfect JR. Cryptococcosis. Infect Dis Clin North Am 2016;30:179-206. [Google Scholar | PubMed]
- 2.Zhao Y, Ye L, Zhao F, Zhang L, Lu Z, Chu T, et al. Cryptococcus neoformans, a global threat to human health. Infect Dis Poverty 2023;12:20. [Google Scholar | PubMed]
- 3.Chen SC, Meyer W, Sorrell TC. Cryptococcus gattii infections. Clin Microbiol Rev 2014;27:980-1024. [Google Scholar | PubMed]
- 4.Siqueira NP, Favalessa OC, Maruyama FH, Dutra V, Nakazato L, Hagen F, et al. Domestic birds as source of Cryptococcus deuterogattii (AFLP6/VGII): Potential risk for cryptococcosis. Mycopathologia 2022;187:103-11. [Google Scholar | PubMed]
- 5.Vu K, Tham R, Uhrig JP, Thompson GR 3rd., Pombejra NS, Jamklang M, et al. Invasion of the central nervous system by Cryptococcus neoformans requires a secreted fungal metalloprotease. mBio 2014;5:e01101-14. [Google Scholar | PubMed]
- 6.Zhou HX, Lu L, Chu T, Wang T, Cao D, Li F, et al. Skeletal cryptococcosis from 1977 to 2013. Front Microbiol 2015;5:740. [Google Scholar | PubMed]
- 7.Li SS, Mody CH. Cryptococcus. Proc Am Thorac Soc 2010;7:186-96. [Google Scholar | PubMed]
- 8.Wager CM, Hole CR, Wozniak KL, Wormley FL Jr. Cryptococcus and phagocytes: Complex interactions that influence disease outcome. Front Microbiol 2016;7:105. [Google Scholar | PubMed]
- 9.Al-Tawfiq JA, Ghandour J. Cryptococcus neoformans abscess and osteomyelitis in an immunocompetent patient with tuberculous lymphadenitis. Infection 2007;35:377-82. [Google Scholar | PubMed]
- 10.Witte DA, Chen I, Brady J, Ramzy I, Truong LD, Ostrowski ML. Cryptococcal osteomyelitis. Report of a case with aspiration biopsy of a humeral lesion with radiologic features of malignancy. Acta Cytol 2000;44:15-8. [Google Scholar | PubMed]
- 11.Liu M, Jiang GN. Surgical treatment of pulmonary cryptococcosis. Zhonghua Jie He He Hu Xi Za Zhi 2006;29:307-9. [Google Scholar | PubMed]
- 12.Moen MD, Lyseng-Williamson KA, Scott LJ. Liposomal amphotericin B: A review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Drugs 2009;69:361-92. [Google Scholar | PubMed]
- 13.Seffah K, Agyeman W, Madeo JL, Ahmad A. Cryptococcus infection in an immunocompetent patient. Cureus 2022;14:e27635. [Google Scholar | PubMed]
- 14.Smith DK, Neal JJ, Holmberg SD. Unexplained opportunistic infections and CD4+ T-lymphocytopenia without HIV infection. An investigation of cases in the United States. The centers for disease control idiopathic CD4+ T-lymphocytopenia task force. N Engl J Med 1993;328:373-9. [Google Scholar | PubMed]
- 15.Regent A, Autran B, Carcelain G, Cheynier R, Terrier B, Charmeteau-De Muylder B, et al. Idiopathic CD4 Lymphocytopenia: Clinical and immunologic characteristics and follow-up of 40 patients. Medicine (Baltimore) 2014;93:61-72. [Google Scholar | PubMed]