Prophylactic intramedullary nailing in impending AFF can prevent catastrophic fractures and reduce the need for complex surgical interventions. Proper vigilance and close follow-up post-fixation are also important
Dr. Rahul Shah, Department of Orthopaedics, Aster Whitefield Hospital, Bengaluru - 560066, Karnataka, India. E-mail: dr.rahulshahortho@gmail.com
Introduction: Bisphosphonates are effective in osteoporosis management but have been linked to atypical femoral fractures (AFFs) with prolonged use. The management of incomplete AFF remains controversial, particularly regarding the role of prophylactic fixation.
Case Report: A 67-year-old female on long-term bisphosphonate therapy presented with a left subtrochanteric fracture following a minor fall. Imaging revealed an impending AFF in the contralateral right femur, leading to prophylactic intramedullary nailing. Six weeks postoperatively, she developed a minimally displaced fracture on the right femur, which was managed conservatively due to the minimal displacement of the fracture as a result of prophylactic nailing. She achieved full fracture healing and unaided mobility without additional surgical intervention.
Conclusion: Prophylactic intramedullary nailing can effectively mitigate fracture displacement and the need for re-surgery in patients with impending AFF. However, further studies are needed to establish standardized management protocols.
Keywords: Atypical femoral fracture, bisphosphonate, bisphosphonate therapy, prophylactic nailing.
Bisphosphonates have proven to be highly effective in managing osteoporosis, significantly reducing the risk of fractures [1]. However, an emerging concern is the association of bisphosphonate therapy with atypical femoral fractures (AFFs), particularly in the femoral shaft. Stress fractures often begin subtly but can progress to complete fractures over time. While complete atypical fractures are widely accepted to be best treated with intramedullary nailing, there remains significant debate regarding the optimal management of incomplete atypical femoral shaft fractures in patients on long-term bisphosphonate therapy. Prolonged use of bisphosphonates (exceeding 5 years) is known to compromise bone microarchitecture, increasing the risk of progression from incomplete to complete fractures [2]. Orthopaedic surgeons face the challenge of accurately identifying and managing these fractures using clinical and radiographic findings. Despite the lack of standardized guidelines, prophylactic fixation is often recommended when diagnostic imaging, such as isotope bone scans or magnetic resonance imaging (MRI), reveals increased uptake or evidence of an incomplete fracture on the tension side of the femoral diaphysis. This case report details the management of bilateral AFFs in a patient with a history of long-term bisphosphonate therapy, who underwent prophylactic nailing on the contralateral side as she had features of impending AFF clinically and radiologically. She eventually developed a complete fracture on the side of prophylactic nailing but did not have to undergo any re-surgery as there was minimal displacement and angulation, emphasizing the rationale for prophylactic intramedullary nailing and its outcomes.
A 67-year-old female presented to the emergency department following a minor fall, reporting injury to her left lower limb. Clinical examination revealed external rotation and shortening of the left leg, with radiographs confirming a subtrochanteric fracture of left femur with features of an AFF (Fig. 1). She gave a drug history of consuming oral ibandronic acid (150 mg/month) for 7 years, as she was diagnosed with osteoporosis, indicated by a spine T-score of −3.22 on bone densitometry. In addition, the patient reported persistent right thigh pain for the preceding 3 months. Given the history of prolonged bisphosphonate use, the trivial nature of the fall, and the contralateral pain, MRI of the right femur was performed, revealing marrow edema (Fig. 2) in the subtrochanteric region, correlating with the clinical site of pain.
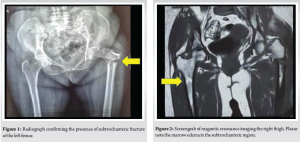
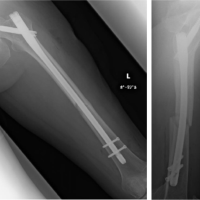
Recognizing the bilateral AFFs and the imminent risk of a right-sided fracture, prophylactic intramedullary nailing was performed on the right femur (Fig. 3), based on the current clinical evidence. This approach also facilitated positioning for subsequent fracture reduction and reconstruction nailing of the left femur (Fig. 4), conducted 2 days later. The postoperative course was uneventful. Bisphosphonate therapy was discontinued, and the patient was started on teriparatide injections, calcium, and vitamin D supplementation. After satisfactory post-operative X-rays (Fig. 5), full weight-bearing mobilization with walker support was initiated.

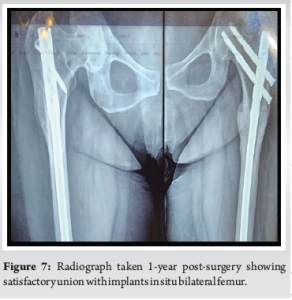
Six weeks into rehabilitation, during one of the mobilization sessions, the patient reported pain at the site of prophylactic nailing in the right femur. Radiographs revealed a minimally displaced fracture in the proximal third of the right femur (Fig. 6). Conservative management was pursued due to the absence of significant displacement or angulation, which was probably due to the prophylactic nail in situ. Mobilization was restricted to bedside exercises for 6 weeks, followed by a gradual return to full weight-bearing activity. There was no complaint of worsening of pain or any other symptoms with this conservative approach. With regular clinical and radiological follow-ups, the patient demonstrated progressive healing, transitioning to single crutch-assisted ambulation by 6 months. One-year post-surgery, complete bilateral fracture consolidation was observed (Fig. 7), and the patient achieved unaided, pain-free mobility. She is still under follow-up and is doing well, with no further symptoms so far.

AFFs account for 1.1% of all femoral fractures and are bilateral in up to 63% of cases [3]. Bisphosphonates are the leading treatments for osteoporosis, acting by inhibiting bone resorption [4-6]. They have been proven to effectively enhance bone density and lower the risk of vertebral and non-vertebral fractures. Prolonged bisphosphonate-induced impairment of bone remodeling may cause an accumulation of microfractures and weakening of the bone [7]. According to the American Society for Bone and Mineral Research, atypical femur fractures are characterized by their location, usually in the subtrochanteric region and diaphysis, their transverse or short oblique configuration, and the absence of trauma history or comminution. The definition also distinguishes complete fractures, marked by characteristic medial spikes, from incomplete fractures confined to the lateral cortex, which correspond to regions of highest biomechanical stress. Additional minor features include radiological signs such as periosteal reaction and increased cortical thickness, along with prodromal symptoms, bilateral occurrence, and delayed healing.
AFFs associated with long-term bisphosphonate therapy exhibit characteristic radiological features, including a transverse or short oblique fracture pattern without comminution, cortical hypertrophy, and thickening of the lateral cortex in the contralateral femur. These fractures typically occur following minimal trauma and are often located between the lesser trochanter and the supracondylar flare of the femur. Concerns regarding AFF have led to suggestions to either pause bisphosphonate treatment, known as a “drug holiday,” or switch to a different anti-osteoporosis therapy. The standard treatment for AFFs is intramedullary fixation. Koh et al. [8] reviewed treatment outcomes and recommended intramedullary devices as the first-line approach, noting that fracture healing can be delayed. Adjunctive therapies, such as teriparatide, and the immediate cessation of bisphosphonates, have been shown to enhance fracture union. Conservative management of AFF is discouraged, as surgical intervention is often required. The prevention and prediction of contralateral femoral fractures are crucial in minimizing patient morbidity. As they are usually bilateral, it is recommended that plain radiograph of the contralateral side is imperative to be screened to avoid a further fracture on the opposite side. In case of no evidence of any fracture but with the presence of prodromal symptoms like thigh pain, advanced imaging modalities, including MRI, isotope bone scans, micro-computed tomography, and positron emission tomography, have been explored for early detection. Prophylactic fixation is advocated in cases of intractable thigh pain, bilateral disease, or previous fracture on the opposite side, particularly when imaging reveals evidence of incomplete fractures [8,9]. Oh et al. [10] in a retrospective study found that 11 out of 17 patients receiving bisphosphonate therapy with subtrochanteric fractures had contralateral fractures (complete or incomplete), all of which were treated with prophylactic nailing. A complete fracture occurred in one patient, which subsequently healed with a bridging callus. Similarly, in our case, the development of a minimally displaced fracture following prophylactic nailing highlights the potential biomechanical challenges in AFF management. Prophylactic nailing was done after evidence of impending AFF and pain. She developed a fracture 6 weeks later, but due to the presence of the nail, there was no significant displacement or angulation, thus avoiding the need for any re-surgery. This also stresses on the importance of prophylactic nailing in suitable patients with AFF.
The case emphasizes the critical importance of judicious bisphosphonate use and heightened clinical vigilance for AFFs in patients presenting with fractures after trivial trauma. Screening for bilateral involvement with X-ray or MRI is essential. Prophylactic intramedullary nailing, as demonstrated in this patient, effectively alleviated pain, minimized fracture displacement, and eliminated the need for additional surgery, prolonged hospitalization, or increased costs. The unique presentation of a fracture occurring weeks after prophylactic nailing further highlights the complexity of AFF management, particularly in the context of long-term bisphosphonate therapy. This case underscores the need for further research and development of standardized guidelines to optimize patient outcomes in managing AFF. Further studies are needed to establish well-defined protocols in the management of symptomatic AFFs.
AFF should be suspected in patients on long-term bisphosphonate therapy presenting with thigh pain or minimal trauma fractures. Bilateral screening with imaging is essential for early detection. Prophylactic intramedullary nailing in impending AFF can prevent catastrophic fractures and reduce the need for complex surgical interventions. However, clinicians must remain vigilant, as fractures may still occur post-fixation, requiring close follow-up and conservative management when appropriate. Discontinuation of bisphosphonates and initiation of alternative osteoporosis therapies, such as teriparatide, play a crucial role in optimizing fracture healing and patient outcomes.
References
- 1.Maraka S, Kennel KA. Bisphosphonates for the prevention and treatment of osteoporosis. BMJ 2015;351:h3783. [Google Scholar]
- 2.Ma S, Goh EL, Jin A, Bhattacharya R, Boughton OR, Patel B, et al. Long-term effects of bisphosphonate therapy: Perforations, microcracks and mechanical properties. Sci Rep 2017;7:43399. [Google Scholar]
- 3.Khan AA, Kaiser S. Atypical femoral fracture. CMAJ 2017;189:E542. [Google Scholar]
- 4.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture intervention trial research group. Lancet 1996;348:1535-41. [Google Scholar]
- 5.Liberman UA, Weiss SR, Bröll J, Minne HW, Quan H, Bell NH, et al. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The alendronate phase III osteoporosis treatment study group. N Engl J Med 1995;333:1437-43. [Google Scholar]
- 6.Napoli N, Novack D, Armamento-Villareal R. Bisphosphonate-associated femoral fracture: Implications for management in patients with malignancies. Osteoporos Int 2010;21:705-8. [Google Scholar]
- 7.Baig MU, Maqbool A. Bisphosphonate-induced atypical femoral shaft fracture. Cureus 2017;9:e1750. [Google Scholar]
- 8.Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: Issues and controversies related to their surgical management. Bone Joint J 2017;99-B:295-302. [Google Scholar]
- 9.Yadav S, Khanna V. Bisphosphonates-induced atypical subtrochanteric fracture femur: A case report. Cureus 2018;10:e2937. [Google Scholar]
- 10.Oh CW, Oh JK, Park KC, Kim JW, Yoon YC. Prophylactic nailing of incomplete atypical femoral fractures. ScientificWorldJournal 2013;2013:450148. [Google Scholar]