Clavicle nailing though a standard procedure has its own complications.
Dr. S Udayan, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Room No. G-125, 1st floor, Gent’s Hostel, Sri Ramachandra Medical College, Porur, Chennai - 600116, Tamil Nadu, India. E-mail: udayan9796@gmail.com
Introduction: Clavicle fractures are common injuries and the trend from non-operative management has been now changed toward operative management. Plate fixation after open reduction and intramedullary nail fixation after closed reduction are the standard operative management techniques. Nail fixation although has advantages of being minimally invasive, it has its own complications. This case series aims to report some of the complications observed in patients referred to our institution after undergoing intramedullary nail fixation of the clavicle at outside hospitals.
Case Report: In this article, we present three patients who underwent closed reduction and intra-medullary nail fixation for displaced middle third clavicle fractures in an outside hospital and developed significant complications post-operatively. In the first case, the patient developed a delayed union of fracture with subsequent implant migration. In the second case, the patient developed a delayed union of fracture with nail bending, causing persistent pain and deformity. The third case presented with a neck abscess resulting from implant-related infection. Each patient was treated with a systematic approach of implant removal, followed by fixation with plate and screws, and appropriate antibiotic therapy for infection.
Conclusion: This case series highlights the potential complications associated with clavicle nailing, emphasizing the need for proper technique and research on implant design. Although clavicle nailing has the advantages of being minimally invasive with lesser soft tissue stripping, clavicle plating remains the gold standard as it provides more rigid fixation and promotes early rehabilitation and recovery. If clavicle nailing is being done, one must be aware of potential complications such as non-union, implant migration, hardware failure, and infections. Early referral and timely intervention are crucial for favorable outcomes.
Keywords: Clavicle nailing, implant migration, neck abscess, delayed union.
Clavicle fractures are one of the common injuries and they account for about 2–5% of all fractures in adults and 10–15% in children [1]. Middle third of the clavicle is the most common site to get fractured. The debate over whether to surgically fix displaced middle third clavicle fractures has evolved significantly, with numerous studies now demonstrating that operative management offers clear advantages over conservative treatment, including lower rates of nonunion and accelerated functional recovery [2]. Clavicle fractures can be surgically treated with a plate or an intramedullary device, most commonly a titanium elastic nail (TENS). Although clavicle open reduction and internal fixation with plate osteosynthesis is the gold standard, intramedullary fixation with TENS s can be preferred in midshaft clavicle fractures with no comminution [3]. This case series presents three patients who underwent clavicle nailing at an outside facility and subsequently presented to our institution with significant complications
Case 1
A 43-year-old gentleman who is a known diabetic and coronary artery disease (stenting done in 2020) on regular medications presented with complaints of persistent pain and implant prominence over the right clavicle for the past 3 months. He had an alleged history of road traffic accident involving a skid and a fall from a two-wheeler 3 months back, during which he sustained a right clavicle fracture. He underwent closed reduction and intramedullary nail fixation in an outside hospital. He denied a history of fever or any repeated trauma after initial injury.
Clinical examination
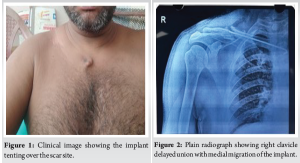
On examination, a healed surgical scar with a mass of size 2 × 2 cm was present over the medial end of the right clavicle (Fig. 1) and the implant tip was well palpable subcutaneously further medial to the previous scar site. There was no discharge or erythema over the scar site. There was no warmth; however, mild tenderness was present. He was able to do a full range of movements but it was painful.
Radiographic findings
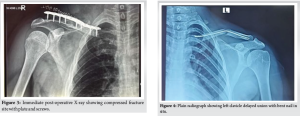
Radiographic evaluation revealed a persistent fracture line over the middle third of the right clavicle, with no radiological evidence of callus formation, suggesting delayed union. The intramedullary nail was observed to have migrated medially, with no fixation or purchase in the lateral fragment (Fig. 2).
Diagnosis and surgical management
The patient was diagnosed to have right clavicle delayed union with medial migration of the implant and planned for revision fixation using a plate and screws.
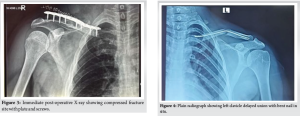
A skin incision was made directly over the clavicle, and the intramedullary nail was removed; the fracture ends were freshened. Reduction was done and fixed using 10-hole pre-contoured clavicle plate with four bicortical purchases made on either side of the fracture and augmented with iliac crest bone graft. Post-operative check X-ray was satisfactory (Fig. 3).
Post-operative protocol
Postoperatively, the patient was put on a sling allowing only pendulum exercises for 2 weeks following which gentle mobilization till 90° of abduction/flexion was allowed. He is currently on follow-up, and radiological assessment of healing is yet to be done.
Case 2
A 25-year-old woman with no co-morbidities presented with a 4-month history of pain and a noticeable swelling over the left clavicle. The pain was insidious, non-progressive, dull, and non-radiating. It was exacerbated with left shoulder movements and relieved with analgesics. She also reported functional impairment in daily activities and cosmetic concerns due to visible deformity. She sustained a left clavicle middle third fracture following a road traffic accident involving 4-wheeler versus 4-wheeler collision. She underwent left clavicle closed reduction and intra-medullary fixation with TENS nail at an outside hospital, primarily for cosmetic reasons. She had no history of fever or any repeated trauma or fall after the initial injury.
Clinical examination
On examination, a bony hard swelling was noted over the middle third of the left clavicle. The swelling was tender and a palpable crepitus was present over the middle third of the clavicle. A healed surgical scar was present at the medial end of the clavicle. The tip of the implant was palpable over the scar site. There are no signs of local infection such as warmth, discharge, or erythema. Her abduction was found to be restricted and painful beyond 120°.
Radiographic findings
Radiographs of the left clavicle showed a persistent fracture line over the middle third of the clavicle, with no evidence of callus formation or healing. Intra-medullary nail was noted to be bent along with apex superior angulation at the fracture site (Fig. 4).
Diagnosis and surgical management
The patient was diagnosed with delayed union of left midshaft clavicle fracture with implant failure and was planned for revision fixation with plate and screws.
Initially, nail removal was attempted through a small incision over the previous scar site but was unsuccessful. Skin incision was made directly over the clavicle, and the intra-medullary nail was removed after great difficulty after cutting it at the fracture site. The fracture site was freshened, reduced, and fixed using 8-holed pre-contoured clavicle plate with three bi-cortical purchases made on either side of the fracture. Post-operative radiograph confirmed satisfactory alignment and implant position (Fig. 5).

Post-operative care and follow-up
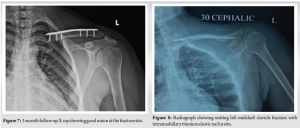
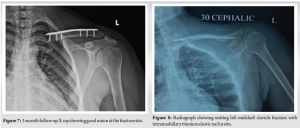
Postoperatively, the patient was put on a sling allowing only pendulum exercises for the first 2 weeks, following which gentle mobilization till 90° of abduction/flexion was allowed. At 1-month follow-up, the patient’s radiography showed good signs of healing (Fig. 6). After 6 weeks, full range of mobilization was started.
The patient was being followed up for 3 months as of now, and the patient’s radiography at 3 months showed good union with the implant intact and well-positioned (Fig. 7). The patient regained full, pain-free shoulder motion and was satisfied with functional outcomes.
Case 3
A 50-year-old male with known chronic liver disease presented to the emergency department with complaints of pain, swelling over the left side of the neck, and progressive difficulty in breathing over the past 24 h. He also reported a history of fever for the past 2 days.
Medical and surgical history
2 months prior, the patient was involved in a road traffic accident and sustained a left midshaft clavicle fracture. He underwent surgical fixation using an intramedullary TENS at an outside hospital. There had been no recent trauma or intervention in the interim.
Clinical examination
On presentation, the patient was febrile and in respiratory distress. Local examination revealed a 3 × 4 cm tender, fluctuant swelling over the left side of the neck. There was no evident skin discoloration or external discharge at the site.
Initial investigations
- Ultrasound of the neck revealed a localized collection adjacent to the left sternocleidomastoid muscle, extending toward the left sternoclavicular joint.
- Plain radiograph of the clavicle demonstrated a uniting midshaft fracture with an intramedullary TENS nail in situ (Fig. 8).
Surgical management
An emergency incision and drainage procedure of the neck abscess was performed by the otolaryngology (ENT) team. Simultaneously, the orthopedic team removed the intramedullary clavicle nail due to suspicion of a contiguous spread of infection from the implant site. Intraoperatively:
- Approximately 10 mL of pus was evacuated from the abscess
- An additional 20 mL of purulent material was drained from the medial entry site of the intramedullary implant (Fig. 9).

- A direct communication between the clavicle implant tract and the neck abscess cavity was observed, indicating implant-related deep-seated infection tracking into the neck.
All specimens were sent for microbiological culture and histopathological examination.
Postoperative course and outcome
Despite timely surgical intervention and initiation of broad-spectrum antibiotics, the patient’s condition rapidly deteriorated. He developed septicemia, followed by multiorgan dysfunction, and ultimately suffered a cardiac arrest. After maximum resuscitative efforts, the patient could not be revived and was declared deceased.
In recent days, there has been a major shift from non-operative management of clavicle fractures to operative management, particularly for displaced and comminuted fractures. Various studies have shown that surgical fixation provides superior functional outcomes and lesser non-union rates compared to non-operative management [2,4]. Open reduction and internal fixation with plate and screws is the standard operative treatment for displaced middle third clavicle fractures. Alternatively, intramedullary fixation of the clavicle can be done with Rockwood pin, Hagie pin, and TEN [5]. TEN has a stress distribution similar to the clavicle [6]. Disadvantages of TEN include routine removal of the implant, shortening, and implant migration [7]. Medial protrusion of the implant is a common complication following clavicle nailing, resulting in minor revision surgeries [8]. Medial protrusion can be reduced by using end caps [9]. Since nail is less resistant to bending forces, there is a possibility of fracture site angulation with non-union and associated bending of nail inside. This will make routine implant removal difficult. Clavicle length is better maintained with clavicle plating. In comminuted middle third clavicle fractures or those where a large butterfly fragment is present, plate fixation remains the operative procedure of choice as it offers better clavicular length maintenance [10]. Infection of implants used for internal fixation of the clavicle can spread to the neck rapidly and present as a deep neck space infection and abscess. These infections pose significant morbidity and potential mortality [11]. Implant removal should be done at the earliest once any signs of infection are noted. Many studies suggest that clinical outcomes post clavicle nailing and clavicle plating are similar, but plating offers fast recovery at 6-month period [3]. More research on proper technique, newer implant design, indications for nailing, and methods to prevent complications should be done; until then, plating remains the gold standard method for fixing clavicle fractures.
Intra-medullary nailing of clavicle fractures, although a promising technique, is not without its risks. Some of the complications observed in this case series, such as neck abscess, delayed-union with nail bending, and implant migration, highlight some of the challenges faced with this method. While nailing may offer benefits in terms of minimal invasiveness and cosmetic considerations, less refracture rate after removal, the rigid fixation and superior healing potential offered by plating make it the preferred method for clavicle fractures, particularly in complex cases.
One should always favor open reduction and internal fixation with plate osteosynthesis for clavicle fractures. Clavicle nailing although minimally invasive has its own drawbacks and needs further research on implants and techniques.
References
- 1.Paladini P, Pellegrini A, Merolla G, Campi F, Porcellini G. Treatment of clavicle fractures. Transl Med UniSa 2012;2:47-58. [Google Scholar | PubMed]
- 2.Liu GD, Tong SL, Ou S, Zhou LS, Fei J, Nan GX, et al. Operative versus non-operative treatment for clavicle fracture: A meta-analysis. Int Orthop 2013;37:1495-500. [Google Scholar | PubMed]
- 3.Fuglesang HF, Flugsrud GB, Randsborg PH, Oord P, Benth JŠ, Utvåg SE. Plate fixation versus intramedullary nailing of completely displaced midshaft fractures of the clavicle: A prospective randomised controlled trial. Bone Joint J 2017;99-B:1095-101. [Google Scholar | PubMed]
- 4.Maheshwari P, Peshin C Sr., Agarwal D. Functional outcomes in surgically treated clavicle fractures: A longitudinal observational study. Cureus 2023;15:e48081. [Google Scholar | PubMed]
- 5.Narsaria N, Singh AK, Arun GR, Seth RR. Surgical fixation of displaced midshaft clavicle fractures: Elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol 2014;15:165-71. [Google Scholar | PubMed]
- 6.Zeng L, Wei H, Liu Y, Zhang W, Pan Y, Zhang W, et al. Titanium elastic nail (TEN) versus reconstruction plate repair of midshaft clavicular fractures: A finite element study. PLoS One 2015;10:e0126131. [Google Scholar | PubMed]
- 7.Hoogervorst P, van Schie P, van den Bekerom MP. Midshaft clavicle fractures: Current concepts. EFORT Open Rev 2018;3:374-80. [Google Scholar | PubMed]
- 8.Wijdicks FJ, Houwert M, Dijkgraaf M, de Lange D, Oosterhuis K, Clevers G, et al. Complications after plate fixation and elastic stable intramedullary nailing of dislocated midshaft clavicle fractures: A retrospective comparison. Int Orthop 2012;36:2139-45. [Google Scholar | PubMed]
- 9.Frigg A, Rillmann P, Perren T, Gerber M, Ryf C. Intramedullary nailing of clavicular midshaft fractures with the titanium elastic nail: Problems and complications. Am J Sports Med 2009;37:352-9. [Google Scholar | PubMed]
- 10.Saha P, Datta P, Ayan S, Garg AK, Bandyopadhyay U, Kundu S. Plate versus titanium elastic nail in treatment of displaced midshaft clavicle fractures: A comparative study. Indian J Orthop 2014;48:587-93. [Google Scholar | PubMed]
- 11.Kataria G, Saxena A, Bhagat S, Singh B, Kaur M, Kaur G. Deep neck space infections: A study of 76 cases. Iran J Otorhinolaryngol 2015;27:293-9. [Google Scholar | PubMed]









