Dedifferentiated adamantinoma is a rare, aggressive tumor requiring careful histopathological and immunohistochemical evaluation for accurate diagnosis and management.
Dr. Pavithra Ethirajan, Department of Histopathology, Apollo Cancer Centre, No. 320, Anna Salai, Teynampet, Nandanam, Chennai - 600 035, Tamil Nadu, India. E-mail: pavithraethirajan1306@gmail.com
Introduction: Adamantinoma is a primary low-grade malignant bone tumor. It is most common in tibia with slight predilection in males. Dedifferentiated adamantinoma is an aggressive variant with worse prognosis.
Case Report: Patient is a 70-year-old female who presented with leg pain. Imaging showed a lytic lesion in the metaphyseo diaphyseal region. Curettings were done and were reported as adamantinoma. Two years later, the patient presented with a recurrent lesion at the same site. Histopathology showed a neoplasm with focal classical adamantinoma and many areas with aggressive morphology including sarcomatoid differentiation. The neoplastic cells in high-grade areas were positive for vimentin with variable loss of cytokeratin. Proliferative index as determined by Ki67 was 20–25% in these areas. With these given immuno-morphological findings, a diagnosis of dedifferentiated adamantinoma was rendered.
Conclusion: Dedifferentiated adamantinoma is an unusual and aggressive variant of adamantinoma. This case highlights the awareness of such a rare entity, thereby preventing misdiagnosis and improper treatment.
Keywords: Adamantinoma, tibia, malignant, osteofibrous dysplasia, sarcoma.
Adamantinoma is a rare primary malignant bone tumor that typically occurs in individuals during their 2nd or 3rd decade of life, with a higher incidence in males. The most common location for this tumor is tibia, followed by fibula. Patients may present with swelling, which can either be painful or painless. On imaging, it appears as a well-defined cortical lesion, often extending into the medullary cavity or surrounding soft tissue. Histologically, the tumor is biphasic, containing both epithelial and bland looking osteofibrous elements. Over time, the clinicopathologic understanding of adamantinoma has expanded, with the identification of an aggressive and rare variant, dedifferentiated adamantinoma [1,2]. On histological examination, this subtype reveals a mixture of classic adamantinoma and areas with pleomorphic sarcomatous cells, marked by increased mitotic figures and occasional osteoid production. In addition, features such as chondroid differentiation, osteoid formation, and clear cell changes have been reported [2,3].
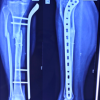
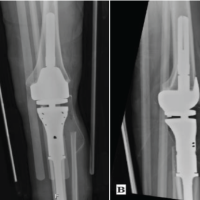
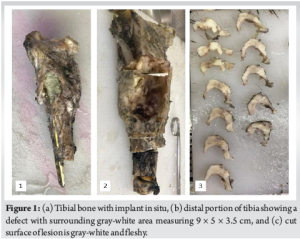
A 72-year-old female presented with leg pain and swelling. Imaging revealed a lytic lesion in the metaphyseal and diaphyseal regions with imaging differentials of giant cell tumor versus aneurysmal bone cyst. Curettage was performed, and the lesion was initially diagnosed as classic adamantinoma. Two years later, the patient developed a recurrence at the same site, following which right distal tibial resection was done. Distal portion of tibia showed a defect filled with bone cement surrounded by gray white lesion measuring 9 × 5 × 3.5 cm (Fig. 1). Cut surface of the lesion was gray white and fleshy. Representative sections were taken, processed, paraffin embedded and 4 microns thick sections were taken and stained with hematoxylin and eosin. Histopathological examination showed a neoplasm with focal classic adamantinoma like areas and many areas showed epithelioid looking cells with marked atypia and nuclear pleomorphism. Background showed osteofibrous stroma. Patchy sarcomatoid areas were also noted. A mitotic count of 12–14/10 high-power field was obtained in these areas (Fig. 2). Immunohistochemistry was done and the neoplastic cells in high-grade and sarcomatoid areas were positive for vimentin with patchy loss of pancytokeratin. Cells also showed p53 overexpression in both high-grade epithelioid and sarcomatoid areas. The proliferation index as determined by Ki-67 was high (20–25%) in these areas (Fig. 3). With the given immune-morphological findings, a diagnosis of dedifferentiated adamantinoma was rendered. A previous diagnosis of adamantinoma combined with the recurrence showing a foci of classic adamantinoma with a clear transition to sarcomatous areas favored this diagnosis. The patient subsequently underwent amputation but did not receive any adjuvant therapy and was lost to follow-up after 1 year.

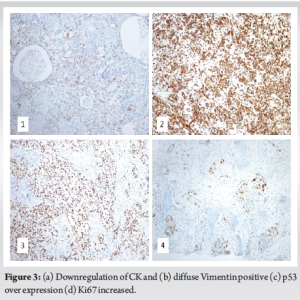
Adamantinoma is a biphasic tumor characterized by both epithelial component and a mesenchymal osteofibrous stroma. The epithelial component can exhibit various patterns, including basaloid, tubular, squamoid, and spindled forms [1,2]. Adamantinoma is classified into three subtypes: Classic adamantinoma, osteofibrous dysplasia-like (OFD-like) adamantinoma, and dedifferentiated adamantinoma. The distinction between the classic and OFD-like subtypes lies in the proportion of the epithelial component. Classic adamantinoma features a predominantly epithelial component with minimal osteofibrous areas, whereas OFD-like adamantinoma is characterized by scattered nests of epithelial cells within the stroma [1,2]. The development of adamantinoma remains a topic of intrigue, with several theories proposed to explain its origin. One theory suggests that during embryonic development, ectodermal epithelial nests become misplaced within mesenchymal tissue, particularly in the subcutaneous tibial region where adamantinoma frequently arises. Another proposed that trauma might implant epithelial cells into the bone [1]. A third hypothesis is that a possibility of a low-grade mesenchymal neoplasm undergoing transformation into an epithelial phenotype, a process that hints at OFD being a potential precursor to adamantinoma [4,5]. While these theories provide clues, the exact pathogenesis of adamantinoma remains unclear [1,6]. Dedifferentiation in adamantinoma is an extremely rare occurrence, with just over ten cases reported worldwide, including only two cases from India [3]. Dedifferentiation refers to the process where the tumor’s epithelial component undergoes a transformation, losing its distinct characteristics and reverting to a more primitive, mesenchymal-like state. This shift is referred to as the revertant mesenchymal phenotype by Izquierdo et al. [7]. Izquierdo et al. reported a case of adamantinoma of tibia treated with an en bloc resection. Five years later, the patient developed a recurrence consisting solely of the sarcomatous component, with no epithelial nests present. Immunohistochemical analysis was negative for cytokeratins. This case illustrates marked sarcomatous dedifferentiation with a complete loss of the epithelial phenotype [7]. Tibia is the most commonly reported site for dedifferentiated adamantinoma, which can either develop de novo or as a recurrence from a classic adamantinoma [2]. Nouri et al. and Hazelbag et al. have reported cases of dedifferentiated adamantinoma occurring in patients with fibrous dysplasia [8,9]. It can affect individuals across a broad age range, from 21 to 83 years. Tirabosco et al. have reported two cases of dedifferentiated adamantinoma occurring in the ulna and rib [3]. The dedifferentiated component is often a high-grade sarcoma, which can include pleomorphic sarcoma, osteosarcoma with chondroblastic differentiation, and spindle cell sarcoma. Of these, osteosarcomatous dedifferentiation is most commonly reported in dedifferentiated adamantinoma [3,7,9]. A conclusive diagnosis necessitates the use of immunohistochemical staining. Epithelial marker positivity is limited to the regions of classic adamantinoma. In contrast, the sarcomatoid-appearing areas in between are negative for these stains [7]. Rekhi et al., in his case report, demonstrated diffuse p53 expression in the sarcomatous dedifferentiated area of one case, while another case showed complete loss of expression [3]. Similarly, Hazelbag et al. reported p53 overexpression in one case [9]. In our case, diffuse p53 expression in the sarcomatous component was noted. This suggests a potential role of p53 in the dedifferentiation process [3]. Diagnostic difficulty arises when there is no definite zone of classical adamantinoma, putting forward a variety of differential diagnosis including various high-grade sarcomas and metastatic carcinoma. A panel of immunostains along with other ancillary studies would help in ruling out these differentials. Dedifferentiated adamatinoma has a worse prognosis with local recurrence and distant metastasis. Metastasis has been reported in lymph nodes and lungs [2,7,8,10]. Surgical resection remains the primary treatment approach. Adjuvant radiation therapy may be considered in instances of incomplete resection [3,9]. Chemotherapy appears to provide limited benefit [7].
Dedifferentiated adamantinoma is a rare and aggressive form of adamantinoma. This case underscores the importance of recognizing this uncommon entity. A diagnosis of dedifferentiated adamantinoma should be considered when encountering a cytokeratin-positive sarcomatous lesion in the tibia. Accurate differentiation from other neoplasms is crucial for ensuring appropriate and timely therapeutic management.
Dedifferentiated adamantinoma is a rare but aggressive variant of adamantinoma that poses diagnostic and therapeutic challenges. This case highlights the importance of long-term follow-up in adamantinoma patients to detect potential dedifferentiation and recurrence. A high index of suspicion, combined with histopathological and immunohistochemical evaluation, is essential for accurate diagnosis. Given its poor prognosis and potential for metastasis, early recognition and complete surgical resection remain crucial for optimal patient outcomes.
References
- 1.Unni KK. Dahlin’s Bone Tumors: General Aspects and Data On 10,165 Cases. 6th ed. Philadelphia, PA: Wollters Kluwer/Lippincott Williams and Wilkins Health; 2010. p. 402. [Google Scholar | PubMed]
- 2.WHO Classification of Tumours Series, Soft Tissue and Bone Tumours. 5th ed., Vol. 3. Lyon, France: World Health Organization; 2020. Available from: https://tumourclassification.iarc.who.int/chapters/33 Last accessed on 11 July 2025. [Google Scholar | PubMed]
- 3.Rekhi B, Sahay A, Puri A. Clinicopathologic features of two rare cases of dedifferentiated adamantinomas, including diagnostic implications. Int J Surg Pathol 2019;27:193-202. [Google Scholar | PubMed]
- 4.Bovée JV, Broek LJ, Boer WI, Hogendoorn PC. Expression of growth factors and their receptors in adamantinoma of long bones and the implication for its histogenesis. J Pathol 1998;184:24-30. [Google Scholar | PubMed]
- 5.Hatori M, Watanabe M, Hosaka M, Sasano H, Narita M, Kokubun S. A classic adamantinoma arising from osteofibrous dysplasia-like adamantinoma in the lower leg: A case report and review of the literature. Tohoku J Exp Med 2006;209:53-9. [Google Scholar | PubMed]
- 6.Czerniak B, Rojas-Corona RR, Dorfman HD. Morphologic diversity of long bone adamantinoma. The concept of differentiated (regressing) adamantinoma and its relationship to osteofibrous dysplasia. Cancer 1989;64:2319-34. [Google Scholar | PubMed]
- 7.Izquierdo FM, Ramos LR, Sánchez-Herráez S, Hernández T, De Álava E, Hazelbag HM. Dedifferentiated classic adamantinoma of the tibia: A report of a case with eventual complete revertant mesenchymal phenotype. Am J Surg Pathol 2010;34:1388-92. [Google Scholar | PubMed]
- 8.Nouri H, Jaafoura H, Bouaziz M, Ouertatani M, Abid L, Meherzi MH, et al. Dedifferentiated adamantinoma associated with fibrous dysplasia. Orthop Traumatol Surg Res 2011;97:770-5. [Google Scholar | PubMed]
- 9.Hazelbag HM, Laforga JB, Roels HJ, Hogendoorn PC. Dedifferentiated adamantinoma with revertant mesenchymal phenotype. Am J Surg Pathol 2003;27:1530-7. [Google Scholar | PubMed]
- 10.Smyth SL, Siddiqi A, Athanasou N, Whitwell D, Majd HS. Adamantinoma: A review of the current literature. J Bone Oncol 2023;41:100489. [Google Scholar | PubMed]