This case series underscores the potential risk of femoral neck fractures following intra-articular corticosteroid injections in patients with advanced hip osteoarthritis, highlighting the need for further research and attention to clarify the impact of these injections on bone integrity and fracture susceptibility.
Dr. Kyle Andrews, Department of Orthopaedic Surgery, ProMedica Toledo Hospital, 2121 Hughes Drive, Toledo, Ohio, USA. E-mail: kyle.andrews@promedica.org
Introduction: Osteoarthritis (OA) is one of the most common orthopedic conditions in the world. Corticosteroid injections (CSIs) are a common treatment option for these patients, with many different options available to patients. The effects vary based on the individual, with some patients experiencing no relief. CSIs work through a variety of immunosuppressive effects, yet the effects on bone health are still debated. Some studies have shown detrimental effects on bone, ranging from bone degeneration to causing fracture. This case series presents a potential link to femoral neck fracture (FNF) from intra-articular corticosteroids.
Case Report: This series highlights three patients at different ages who underwent intra-articular CSI for known ipsilateral hip OA and subsequently presented with a FNF from a ground-level fall between 4 and 32-days post-procedure. Two of the patients had a right subcapital FNF, while one of the patients demonstrated a left transcervical fracture.
Conclusion: Corticosteroids are known to lead to osteoporosis. This case report underlines the potential association between CSIs and subsequent FNF. More emphasis should be placed on the potential bone effects of intra-articular steroid injections, as the decision should be patient-specific to ensure no increased risk is made. Further research should be conducted to look into this potential link.
Keywords: Steroids, fracture, osteoarthritis, femur, intra-articular, bone.
Osteoarthritis (OA) of the hip is a commonly encountered diagnosis that is seeing an uptick in prevalence due to a population that is not only increasing in age but also in weight [1]. The prevalence of OA is around 240 million, making it one of the most prevalent orthopedic conditions in the world [2]. First-line treatment options include the least invasive options, including activity modification, weight loss, and physical therapy. Pharmacologic adjuncts such as the use of non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroid injections (CSIs) are also an important part of the orthopedic surgeon’s armamentarium to relieve the pain associated with this pathology [3]. Several steroids, including methylprednisolone, betamethasone, and triamcinolone, exist for use in CSI for hip OA. Their mechanism of action provides local immunosuppressive and powerful anti-inflammatory effects, specifically by interrupting the production of inflammatory mediators [4]. The efficacy of CSI in these instances is widely variable – with some patients seeing little to no relief while others report pain alleviation for up to 1 year afterward [5]. In addition to a lack of consensus on the therapeutic efficacy of steroid injections for OA, there is very limited data on the effect of these steroids on bone health. Although a mainstay in treatment, some studies have implicated the use of steroid injections and fractures in osteoporotic patients. Some studies have even pointed out that one of the side effects is rapid degeneration of bone, but not necessarily fractures [6]. This series highlights the cases of three individuals with known, pre-existing hip OA who underwent an intra-articular CSI and subsequently presented with a femoral neck fracture (FNF) within 5 weeks of the aforementioned procedure. The degree of OA, which was determined on radiographs by one (KAA) fellowship-trained orthopedic surgeon, was classified by the Tönnis classification. Tönnis grade 0 represents no signs of OA; grade 1 represents slight joint space narrowing with sclerosis of the femoral head and/or acetabulum; grade 2 represents increasing joint space narrowing, small cysts in the femoral head and/or acetabulum, and some loss of sphericity of the femoral head; grade 3 represents severe joint space narrowing or obliteration of the joint, large cysts, and severe deformity of the femoral head [7].
Case #1
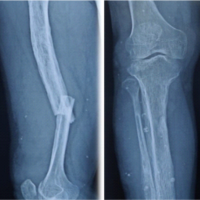
This is the case of a 47-year-old Caucasian female community ambulator with a body mass index (BMI) of 53.1 kg/m2 and past medical history of hypothyroidism and hypertension who presented with a 3-month history of right hip pain with insidious onset. Initial radiographs determined her right hip to have a Tönnis grade of 3. She only had minimal pain relief with the use of NSAIDs and proceeded with an intra-articular injection of the right hip with 80 mg of methylprednisolone acetate and 3 mL of 1% lidocaine. Four days later, she suffered a ground-level fall and was subsequently found to have a right subcapital FNF. She underwent total hip replacement the following day.
Case #2
This is the case of a 76-year-old Caucasian female community ambulator with a BMI of 21.6 kg/m2 and past medical history of osteoporosis who presented with a 2-year history of left hip pain with insidious onset. Initial radiographs determined her left hip to have a Tönnis grade of 2. She attempted physical therapy and the use of NSAIDs with minimal improvement in her pain. She underwent an intra-articular injection of her left hip with 80 mg of triamcinolone acetonide. Thirty-two days later, she suffered a ground-level fall and was subsequently found to have a left transcervical FNF. She underwent total hip replacement thereafter.
Case #3
This is the case of a 70-year-old Caucasian male community ambulator with a BMI of 25.1 kg/m2 and past medical history of chronic obstructive pulmonary disease and benign prostatic hyperplasia who presented with a 1-month history of right hip pain that began acutely with no inciting traumatic event. Initial radiographs determined his right hip to have a Tönnis grade of 3. He attempted the use of NSAIDs but only had minimal pain relief. His discomfort led him to use a cane to ambulate. He underwent an intra-articular injection of his right hip with 80 mg of triamcinolone acetonide and 1% lidocaine. Eight days later, he presented with a right subcapital FNF from a ground-level fall. He underwent total hip replacement.
Many papers have reported on the association between CSI and FNF this potential link, but the data still remains scarce [2-14]. Through a variety of mechanisms, corticosteroids are known to lead to osteoporosis. Glucocorticoids affect the signaling pathway for the differentiation of osteoblasts by limiting specific proteins such as bone morphogenic protein and peroxisome proliferator-activated receptor-γ2. At normal doses, they are associated with osteoblast turnover and autophagy, while high doses have been shown to cause apoptosis of said cells [13]. The opposite, however, is seen with osteoclasts, as corticosteroids increase the differentiation of these cells in a dose-dependent manner. They also decrease calcium absorption in the bowel while increasing the renal excretion. Although these effects are known to occur through systemic or oral steroids as opposed to injections, it is unknown how much of a reduced effect, if any, is seen through a concentrated, localized injection such as in the presented cases. It is well-documented that progressive hip OA alters the biomechanics of the lower extremity. As loss of cartilage increases, impingement and decreased range of motion of the femoral head within the acetabulum ensue [15]. Although they can often temporarily improve symptoms of OA, CSIs are known to have deleterious effects on cartilage at higher doses [16]. These effects, however, have not been demonstrated clinically in patients receiving injections, as many already have some form of cartilage and/or bone loss before experiencing a fracture, making it difficult to discern whether any injection actually has an impact on future fracture risk. Although many patients opt for multiple CSIs to find relief from hip OA symptoms, it is unclear whether or not advisory should be given regarding an increased chance of fracture in the future. Each member of this cohort only received one injection before their traumatic injury. It is unlikely that the time from injection to injury played such an integral role in compromising bony and soft tissue integrity, as the duration between injection and fracture was quite limited. There are some limitations that prevent us from concluding that steroids itself are the cause of these fractures. For one, arthritis itself was present in all individuals studied, and when severe, this could lead to non-mobile joints, making them more prone to fracture [17]. Especially in the setting of osteoporosis, this becomes even more likely as a potential explanation. Steroids also affect the patient’s pain sensation, which could’ve further affected their knowledge of their limited mobility and resulted in riskier movements, eventually leading to fracture. Although outside of the scope of this case series, it is fair to ponder if repeated CSI provide more harm than good. Some studies have suggested that repeated CSI can increase the rate at which OA occurs; however, other works believe that this may be a coincidental as opposed to a causal finding [16]. Each patient in this case series did receive a steroid injection before presenting with a fracture, but it is impossible to conclude that the steroids directly led to the fractures.
This study demonstrates the potential link between intra-articular steroid injections and FNF s through a series of patient cases. It has been shown in prior research that CSIs do have an effect on bone turnover, increasing the likelihood of osteoporosis. Steroids have also been linked to cartilage loss, which could also cause eventual bone fracture. Although it cannot be determined that these injections directly impacted the patient’s fracture risk, it is still something that should be considered. Given the paucity of literature highlighting CSI and FNF, the authors present this case series as a potential cautionary tale for practitioners and patients alike, as the likelihood that there is some correlation should not be completely ignored. Future in vivo and cadaveric studies could assist in clarifying any potential relation between the two entities.
This case series presents a potential association between intra-articular corticosteroid injections (CSI) and femoral neck fractures (FNF) in patients with advanced hip OA. Intra-articular steroid injections are commonly utilized in the management of hip OA to alleviate pain and improve function; however, the impact of these injections on bone health, particularly in terms of fracture risk, remains inadequately studied. This report details three cases in which patients with severe hip OA received CSI and subsequently experienced FNFs within a short time frame. Although causality cannot be definitively established, these cases raise important concerns regarding the safety of CSI, especially in patients with significant joint degeneration or osteoporosis. Given the paucity of literature on this topic, this case series provides valuable insight into a potential complication of CSI that warrants further investigation. The findings serve as a cautionary note for clinicians in considering the long-term effects of corticosteroid use on bone integrity in OA management, making this report relevant to those involved in the care of patients with hip OA.
References
- 1.Badley EM, Wilfong JM, Yip C, Millstone DB, Perruccio AV. The contribution of age and obesity to the number of painful joint sites in individuals reporting osteoarthritis: A population-based study. Rheumatology (Oxford) 2020;59:3350-7. [Google Scholar | PubMed]
- 2.Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage 2022;30:184-95. [Google Scholar | PubMed]
- 3.Nicholas E, Cheng J, Moley PJ. Non-operative treatment options for osteoarthritis in the hip. HSS J 2023;19:486-93. [Google Scholar | PubMed]
- 4.Choueiri M, Chevalier X, Eymard F. Intraarticular corticosteroids for hip osteoarthritis: A review. Cartilage 2021;13:122S-31S. [Google Scholar | PubMed]
- 5.Rampal S, Jaiman A, Tokgöz MA, Arumugam G, Sivananthan S, Singh RS, et al. A review of the efficacy of intraarticular hip injection for patients with hip osteoarthritis: To inject or not to inject in hip osteoarthritis? Jt Dis Relat Surg 2022;33:255-62. [Google Scholar | PubMed]
- 6.Sanguino RA, Sood V, Santiago KA, Cheng J, Casey E, Mintz D, et al. Prevalence of rapidly progressive osteoarthritis of the hip following intra-articular steroid injections. PM R 2023;15:259-64. [Google Scholar | PubMed]
- 7.Kovalenko B, Bremjit P, Fernando N. Classifications in brief: Tönnis classification of hip osteoarthritis. Clin Orthop Relat Res 2018;476:1680-4. [Google Scholar | PubMed]
- 8.Sytsma TT, Thomas S, Fischer KM, Greenlund LS. Corticosteroid injections and risk of fracture. JAMA Netw Open 2024;7:e2414316. [Google Scholar | PubMed]
- 9.Guermazi A, Hunter DJ, Kloppenburg M. Debate: Intra-articular steroid injections for osteoarthritis – Harmful or helpful? Osteoarthr Imaging 2023;3:100163. [Google Scholar | PubMed]
- 10.Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 2014;5:351-61. [Google Scholar | PubMed]
- 11.Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A. Intra-articular corticosteroid injections in the hip and knee: Perhaps not as safe as we thought? Radiology 2019;293:656-63. [Google Scholar | PubMed]
- 12.Hsieh BJ, Shen D, Chan TC, Cho YT, Tang CH, Chu CY. Higher cumulative dose of topical corticosteroids is associated with osteoporosis and major osteoporotic fracture: A nationwide case-control study. J Eur Acad Dermatol Venereol 2024;38:1347-56. [Google Scholar | PubMed]
- 13.Kobza AO, Herman D, Papaioannou A, Lau AN, Adachi JD. Understanding and managing corticosteroid-induced osteoporosis. Open Access Rheumatol 2021;13:177-90. [Google Scholar | PubMed]
- 14.Carreon LY, Ong KL, Lau E, Kurtz SM, Glassman SD. Risk of osteoporotic fracture after steroid injections in patients with Medicare. Am J Orthop (Belle Mead NJ) 2017;46:E293-300. [Google Scholar | PubMed]
- 15.Porta M, Pau M, Leban B, Deidda M, Sorrentino M, Arippa F, et al. Lower limb kinematics in individuals with hip osteoarthritis during gait: A focus on adaptative strategies and interlimb symmetry. Bioengineering (Basel) 2021;8:47. [Google Scholar | PubMed]
- 16.Streck LE, Braun S, Spilo K, Boettner CS, Brenneis M, Boettner F. How safe are intra-articular corticosteroid injections to the hip? BMC Musculoskelet Disord 2023;24:665. [Google Scholar | PubMed]
- 17.Wright NC, Lisse JR, Walitt BT, Eaton CB, Chen Z, Women’s Health Initiative Investigators. Arthritis increases the risk for fractures–Results from the Women’s health initiative. J Rheumatol 2011;38:1680-8. [Google Scholar | PubMed]