Thorough clinical examination, a high degree of suspicion, and appropriate investigations are of paramount importance in the early diagnosis and treatment of tubercular lesions of flat bones
Dr. Avirup Das, Department of Orthopaedics, St. Stephen’s Hospital, Tis Hazari, Delhi - 110054, India. E-mail: dasavirup11@gmail.com
Introduction: Tuberculosis (TB) is an endemic disease worldwide, especially in the Indian subcontinent. Most common locations for osteoarticular TB are the vertebral column and the hip. TB of flat bones, such as the scapula, is an extremely rare entity.
Case Report: The following case report describes a rare case of TB of the spine of the scapula in a young adult presenting with vague pain over the right scapular region and an osteolytic lesion over the spine of the scapula. After a suspicious magnetic resonance imag-ing scan, the diagnosis was finally confirmed on biopsy and culture. The patient was suc-cessfully managed with a four drug antitubercular regimen.
Conclusion: Diagnosis is often delayed due to a lack of awareness among clinicians and a non specific radiological picture. TB should be a differential diagnosis in isolated scapular pain, particularly in an endemic region, and biopsy may be helpful in cases of doubtful ra-diological presentation.
Keywords: Scapula tuberculosis, osteoarticular tuberculosis, tuberculosis scapular spine, musculoskeletal tuberculosis.
Tuberculosis (TB) is a preventable and usually curable disease. Yet in 2022, TB was the world’s second leading cause of death from a single infectious agent, after coronavirus disease 19 [1]. It caused almost twice as many deaths as human immunodeficiency virus/acquired immunodeficiency syndrome. India accounted for 27% of global TB cases in 2022 [1]. Osteoarticular TB accounts for 1–5% of all TB cases and 15% of extrapulmonary TB cases, of which the most commonly affected part is the spine [2]. Isolated involvement of a flat bone, such as the scapula, without any other primary focus, is extremely rare, and till now, only a handful of cases of scapula TB have been reported. This article focuses on the pitfalls in diagnosing TB in such an unusual site, such as the scapula, and its appropriate management.
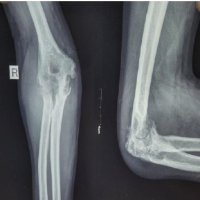
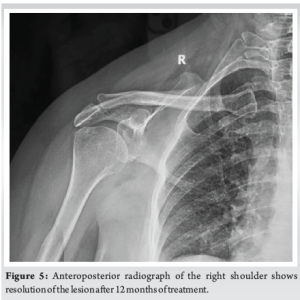
A 20-year-old male presented with pain in the right shoulder region for 2 months. Pain was insidious in onset and dull in nature. Pain was slowly and gradually progressive, aggravating with shoulder movements, but the range of motion was not restricted. He had an occasional lowgrade fever for the past 3 months. There was no history of recent trauma, weight loss, or loss of appetite. There was no past family history of TB. Upon examination, there was no visible fullness over the scapular region. There was tenderness over the spine of the scapula and the adjacent area. No palpable swelling was present. Full range of motion of the shoulder was present, but it was terminally painful. There was no local rise in temperature. There was no hepatosplenomegaly. The plain anteroposterior radiograph of the right scapula revealed a radiolucent, wellfcircumscribed osteolytic lesion at the spine of the scapula with minimal soft tissue involvement (Fig. 1). Other than a raised erythrocyte sedimentation rate (ESR) of 82 mm/h, the rest of the hematological parameters were within normal range. Magnetic resonance imaging (MRI) showed an abnormal marrow signal intensity lesion in the lateral aspect of the spine of the right scapula extending into the proximal acromion process, associated with intraosseous and extraosseous soft tissue, cortical breach, narrow zone of transition, and diffuse surrounding myocutaneous inflammatory changes (Fig. 2). The lesion showed an irregular permeative type of periosteal reaction and a surrounding partially sclerotic rim. A sample was sent from the spine of the scapula for biopsy, and it showed extensive areas of necrosis with numerous discrete epithelioid cell granulomas and Langhan’s giant cells in fibrocollagenous stroma (Fig. 3 and 4). It was consistent with TB, and based on the histopathology report, the patient was treated with four drug antitubercular therapy for 12 months. There was complete resolution both clinically and radiologically at the end of 1.5 years (Fig. 5).
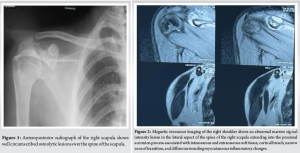
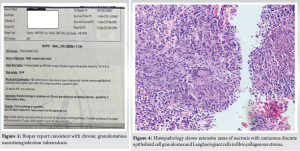
TB of bones and joints is not so uncommon in endemic regions and is associated with significant morbidity. The primary challenge is not the disease pathogenicity itself but the lack of timely diagnosis. After an initial pulmonary infection, TB can involve bones and joints through hematogenous seeding of bacilli. It starts as osteomyelitis in the growth plates of bones, due to its high vascularity, and then spreads to involve the joint [3]. Spine is considered to be the most common site of osteoarticular TB, followed by femur, tibia, and small bones of the hand and feet [4,5,6]. Flat, bone like scapula is a rare site for bony TB. However, in an endemic region such as India, any immunocompetent individual is susceptible to the development of uncommon forms of osteoarticular TB. A patient with scapula TB may present with symptoms of pain over the shoulder, with or without palpable swelling. Initially, tenderness over the affected area can be found. Local rise of temperature and redness are usually not found. Diagnosis is already too late if a discharging sinus is present. The differential diagnosis of these above clinical features includes eosinophilic granuloma, sarcoidosis, metastasis, pyogenic osteomyelitis, and fungal infections [7]. Diagnosis is achieved by being more vigilant toward the symptoms, and the absence of any systemic involvement should also raise suspicion. A thorough clinical examination needs to be done before laboratory and radiological investigations. Markedly raised ESR may assist in diagnosis. Early radiographic images, though not pathognomonic, may show osteolytic lesions with minimal sclerosis with no sequestrum [4,6,8]. MRI, though a useful diagnostic tool, may not be confirmatory, as in this case, MRI showed abnormal marrow signal intensity in the lateral aspect of the spine of the scapula extending to soft tissues and cortical breach. To differentiate TB from other differentials, histopathology is required, which can show epithelioid granuloma as in this case. In the absence of giant sequestrum, most of the osteoarticular TB can be treated with antitubercular therapy alone. An effective multidrug regimen can help in early disease remission [9]. Surgical excision may be required in case of inadequate response to antitubercular treatment for 4–6 weeks or case of giant sequestrum [10]. In the present case, 12 months of antitubercular therapy had completely healed the lesion.
Tubercular osteomyelitis, though rare, is an important differential diagnosis of isolated scapular pain, especially in an endemic region. Lack of awareness, vague clinical picture, and non specific radiography may pose a challenge in diagnosis. Histopathology remains the ultimate diagnostic tool. It is not possible to isolate the bacilli all the time, and treatment has to be started on the basis of the granuloma. If diagnosed early, most of these lesions can be successfully managed by antitubercular therapy alone.
TB of flat bones is a rare entity that requires a high index of suspicion for accurate diagnosis. MRI and Biopsy remain invaluable tools for confirmation of diagnosis.
References
- 1.Global Tuberculosis Report 2023. Available from: https://www.who.int/publications/i/item/9789240083851 [Last accessed on 2024 Jun 18]. [Google Scholar | PubMed]
- 2.Jagtap SA, Sonawane DV, Saraogi AA. Isolated tuberculosis of scapula in a young adult. Int J Mycobacteriol 2013;2:114-7. [Google Scholar | PubMed]
- 3.Iseman MD. A Clinician’s Guide to Tuberculosis. Philadelphia, PA: Lippincott Williams and Wilkins; 2000. p. 162-70. [Google Scholar | PubMed]
- 4.Arriaza BT, Salo W, Aufderheide AC, Holcomb TA. Pre-columbian tuberculosis in Northern Chile: Molecular and skeletal evidence. Am J Phys Anthropol 1995;98:37-45. [Google Scholar | PubMed]
- 5.Sahoo M, Sahai K, Nayak VM. Scapulohumeral tuberculosis diagnosed by fine needle aspiration cytology. Acta Cytol 1998;42:435-6. [Google Scholar | PubMed]
- 6.Lee S, Abramson S. Infections of the musculoskeletal system by M tuberculosis. In: Rom W, Grays S, editors. Tuberculosis. Boston: Little Brown; 1996. p. 635-44. [Google Scholar | PubMed]
- 7.Engin G, Acunas B, Acunas G, Tunaci M. Imaging of extrapulmonary tuberculo-sis. Radiographics 2000;20:471-88. [Google Scholar | PubMed]
- 8.Mathlouthi A, M’Rad SB, Merai S, Friaa T, Mestiri I, Miled BK, et al. Tubercu-losis of the thoracic wall. Presentation of 4 personal cases and review of the lit-erature. Rev Pneumol Clin 1998;54:182-6. [Google Scholar | PubMed]
- 9.Singh A, Chatterjee P, Pai MC, Chacko RT. Tuberculous osteomyelitis of the scapula masquerading as metastasis. J Radiol Case Rep 2009;3:27-31. [Google Scholar | PubMed]
- 10.Khan SS, Zahid M, Sharma B, Hasan A. Tuberculosis of frontal bone: A case re-port. Indian J Tub 2001;48:95-6. [Google Scholar | PubMed]