Geriatric acetabular fracture was successfully managed using the modified Stoppa approach with suprapectineal plating, allowing early mobilisation and full weight-bearing by six weeks, improving functional outcome despite osteoporotic bone in elderly.
Dr. Tarun Prashanth, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai - 600116, Tamil Nadu, India. E-mail: tarun10007@gmail.com
Introduction: Geriatric acetabular fractures resulting from low-energy trauma represent an emerging challenge in orthopedic trauma care. This case highlights the successful management of a complex osteoporotic acetabular fracture with medial dome impaction (“Gull sign”) and quadrilateral plate involvement using a modified Stoppa approach with suprapectineal plating, followed by an accelerated rehabilitation protocol. While not the first report of its kind, this case provides critical insights into achieving early weight-bearing in elderly patients, addressing a key gap in current management strategies for these challenging fractures.
Case Report: A 63-year-old male presented with right hip pain and inability to bear weight after a standing-height fall. Imaging revealed a comminuted right acetabular fracture with superomedial dome impaction, quadrilateral plate involvement, and central subluxation. The patient underwent open reduction and internal fixation through a modified Stoppa approach using a suprapectineal plate. Postoperatively, an accelerated rehabilitation protocol was implemented, progressing to full weight-bearing by 6 weeks with radiographic evidence of union.
Conclusion: This case demonstrates that anatomical reduction and stable fixation of complex geriatric acetabular fractures can be achieved through the modified Stoppa approach with suprapectineal plating. More importantly, it establishes the feasibility and safety of an accelerated rehabilitation protocol enabling full weight-bearing by 6 weeks postoperatively. These findings significantly advance the management of osteoporotic acetabular fractures by providing orthopedic surgeons with a replicable treatment strategy that prioritizes early mobilization – a critical factor in reducing complications and improving functional outcomes in elderly patients. The protocol presented here has broad clinical implications for geriatric trauma care and post-operative rehabilitation.
Keywords: Acetabular fractures, osteoporosis, geriatric trauma, fracture fixation, early mobilization.
Acetabular fractures typically result from high-energy trauma in the young population and are classified using the Judet and Letournel system. However, atypical acetabular fractures occur with minimal trauma in the elderly population due to osteoporosis. These atypical fractures do not follow the Judet and Letournel classification. The incidence of acetabular fractures in the elderly population has significantly increased over the last years [1]. The age that defines the elderly population is more than 55 years [2]. These fractures often involve the anterior column, medial wall, or superior dome and may be missed on initial imaging. There is no specific treatment protocol for atypical acetabular fractures in the elderly, because fracture comminution and impaction are more common in the elderly due to osteoporosis [3]. The treatment options include non-operative management, percutaneous fracture fixation, open reduction and internal fixation (ORIF) with or without simultaneous total hip replacement, and delayed total hip replacement. Early recognition, appropriate management, and early mobilization are crucial to good functional outcomes in the elderly.
A 63-year-old male sustained a low velocity injury – a fall from standing height. He was brought to the emergency department with complaints of pain over the right hip and unable to weight bear on the right lower limb since the time of injury. On examination, he was hemodynamically stable. Clinically, he had tenderness over the right hip anterior joint line with restricted right hip movements. The attitude of the right lower limb was externally rotated. Dorsalis pedis and posterior tibial pulses were well palpable and equal to those of the contralateral limb. There were no signs of neurological deficit.
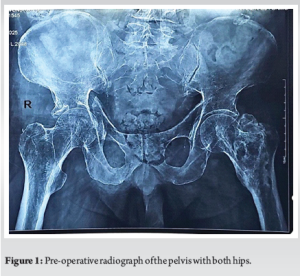
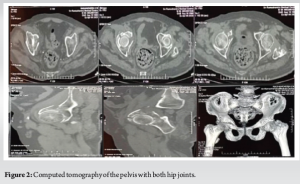
As a first investigation of choice, X-ray of the pelvis with both hips was taken, which revealed a right acetabular fracture with superomedial dome impaction (Gull sign) [4-6], quadrilateral plate involvement and central dislocation with break in the iliopectineal line (Fig. 1). Computed tomography (CT) of the pelvis with both hip joints was taken to get a better anatomy of the fracture pattern and to know the amount of comminution and for pre-operative planning (Fig. 2).
The management of acetabular fractures poses a significant dilemma in choosing between operative and non-operative treatment modalities. In our case, considering the age, bone quality, comminution of the fracture, need for anatomical fixation, and early mobilization, we opted for ORIF. The patient was taken to surgery within 48 h of injury after obtaining anesthesia fitness. Under spinal and epidural anesthesia, the patient was positioned in the supine position, using modified Stoppa’s approach, and the patient underwent ORIF with a 12-hole suprapectineal plate and appropriate screws. Intraoperatively, the impacted fragment and central dislocation were reduced and fixed with this special suprapectineal plate, which also buttresses the quadrilateral plate. Intraoperatively, the reduction was found to be satisfactory under C-Arm guidance. Post-operative X-ray was done on post-operative day 2, which showed excellent reduction (Fig. 3).

Post-operatively, from day 1, the patient was started on chest physiotherapy, incentive spirometry, and ankle pumping exercises. The patient was started on chemical deep vein thrombosis prophylaxis from post-operative day 2. The patient was started on in-bed mobilization and knee range of motion exercises for the first 2 weeks, and then started on non-weight-bearing mobilization of the right lower limb till the 6th week. After a 6-week post-operative period, the patient was started on full weight-bearing mobilization on the right side following postoperative 6-week X-ray evaluation (Fig. 4). There were signs of radiological union, and hence full weight-bearing mobilization on the right side was started after 6 weeks post-operative. There was no evidence of neurological deficit.

The age distribution of acetabular fracture patients has shifted dramatically: while these injuries predominantly affected young males from the 1960s to 1990s, the 1990s saw a sharp rise in geriatric acetabular fracture cases [7,8]. The majority of geriatric acetabular fractures are osteoporotic fractures following low-energy trauma [4,9]. The most common mechanism involves a low-energy fall from standing height with the hip in extension and neutral rotation [10,11]. Most commonly, anterior structures of the acetabulum (anterior column, anterior wall, and medial wall) are involved in the geriatric population, and due to poor bone quality, there is an increase in the rate of comminution and articular impaction [4-6]. The Judet and Letournel classification is the gold standard for categorizing acetabular fractures, dividing them into elementary and associated patterns. However, this system was designed for traumatic fractures in normal bone and often fails to adequately describe atypical acetabular fractures, which occur due to insufficiency, pathological bone conditions, or stress mechanisms.
The goal of treatment in the elderly population should include pain relief, early mobilization, and return to independent activities of daily living [12]. Radiographic evaluation includes a standard anteroposterior view of the pelvis along with iliac and obturator oblique views of the pelvis. Fracture of the acetabulum in elderly patients may be missed easily [13]. A CT scan was helpful in diagnosing bone comminution and impaction, which was not visible on plain radiograph [3].
The available treatment options include conservative management, percutaneous fixation (closed or open reduction), ORIF, combined osteosynthesis and total hip arthroplasty (THA), acute THA without osteosynthesis, and delayed THA [12]. Conservative management with skeletal traction and bed rest can be opted for the elderly with low functional demand, multiple comorbidities, and fractures with minimal displacement <5 mm in weight-bearing dome and in posterior wall fractures involving <50% articular surface [14]. It can lead to devastating complications such as pulmonary and urinary infections, thromboembolic disease, and a recumbency ulcer if bedridden for more than 10 days. Hence, early and safe mobilization is a priority if opted for conservative management. Minimally invasive fracture fixation with percutaneous screws has the advantage of less blood loss, less chance of infection, and quicker recovery. Still, the procedure is technically demanding, and the learning curve is steep [15]. ORIF of the acetabular fracture in the elderly can achieve anatomical reduction but yields suboptimal results due to poor bone quality [16]. The Gull sign has been considered to be a predictor of poor results in the elderly [4-6]. Fracture of the quadrilateral plate is also common in the elderly, which is managed by buttress plating using the modified Stoppa approach. The modified Stoppa approach provides good access to the acetabulum from inside the pelvis for reduction and fixation of the quadrilateral plate as well as the impacted superomedial portion of the acetabulum [9]. This makes the Modified Stoppa approach a preferable approach for anterior acetabular fracture fixation in elderly patients. Combined osteosynthesis and total hip replacement is a complex surgical procedure that requires an advanced skillset [17]. Osteosynthesis is done to restore the anatomy and thus create a stable bed for subsequent acetabular cup implantation. Increased blood loss, increased surgical time, and increased physiological stress to the patient are the downsides of combined osteosynthetic and total hip replacement. Acute THA after acetabular fracture is indicated in subchondral impaction on either the acetabulum or femoral head side, femoral head fracture, severe intra-articular comminution, and pre-injury symptomatic hip arthritis [18]. Delayed THA is indicated in patients who develop post-traumatic arthritis after either osteosynthetic or non-operatively managed fractures of the acetabulum.
Rehabilitation is critical for elderly acetabular fracture patients, reducing morbidity and restoring mobility. Early mobilization significantly enhances outcomes. However, there are no standard guidelines for rehabilitation after an acetabular fracture in elderly patients.
Atypical acetabular fractures in the elderly, typically resulting from low-energy trauma in osteoporotic bone, present distinct management challenges. These fractures often deviate from classic Judet-Letournel classifications and exhibit high rates of comminution and impaction (e.g., the “Gull sign”). Successful treatment hinges on three pillars: prioritizing early mobilization, implementing individualized surgical approaches (such as ORIF via the modified Stoppa or THA in severe cases), and integrating multidisciplinary care to mitigate complications (including thromboembolism and elevated mortality). While standardized rehabilitation protocols remain lacking, focused rehabilitation is essential for functional recovery. The overarching goals are pain control, anatomical restoration where feasible, and, critically, the rapid restoration of patient independence.
Geriatric acetabular fractures with osteoporotic bone and atypical fracture patterns demands a strategic approach. The modified Stoppa approach with suprapectineal plating ensures stable fixation, enabling safe early mobilisation. Prioritizing early weight-bearing significantly reduces morbidity and accelerates functional recovery in elderly patients.
References
- 1.Fritz A, Gericke L, Hoch A, Josten C, Osterhoff G. Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury 2020;51:352-6. [Google Scholar | PubMed]
- 2.Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged >55 years: A systematic review of the literature. Bone Joint J 2014;96-B:157-63. [Google Scholar | PubMed]
- 3.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: An epidemiological and radiological study. J Bone Joint Surg Br 2010;92:250-7. [Google Scholar | PubMed]
- 4.Pagenkopf E, Grose A, Partal G, Helfet DL. Acetabular fractures in the elderly: Treatment recommendations. HSS J 2006;2:161-71. [Google Scholar | PubMed]
- 5.Li YL, Tang YY. Displaced acetabular fractures in the elderly: Results after open reduction and internal fixation. Injury 2014;45:1908-13. [Google Scholar | PubMed]
- 6.Anglen JO, Burd TA, Hendricks KJ, Harrison P. The “gull sign”: A harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma 2003;17:625-34. [Google Scholar | PubMed]
- 7.Hoellen IP, Mentzel M, Bischoff M, Kinzl L. Acetabular fractures in the elderly - primary endoprosthesis. Orthopade 1997;26:348-53. [Google Scholar | PubMed]
- 8.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, et al. Changes in the treatment of acetabular fractures over 15 years: Analysis of 1266 cases treated by the German pelvic multicentre study group (DAO/DGU). Injury 2010;41:839-51. [Google Scholar | PubMed]
- 9.Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury 2011;42:1130-4. [Google Scholar | PubMed]
- 10.Cornell CN. Management of acetabular fractures in the elderly patient. HSS J 2005;1:25-30. [Google Scholar | PubMed]
- 11.Rommens PM, Herteleer M, Handrich K, Boudissa M, Wagner D, Hopf JC. Medial buttressing of the quadrilateral surface in acetabular and periprosthetic acetabular fractures. PLoS One 2020;15:e0243592. [Google Scholar | PubMed]
- 12.Folsch C, Alwani MM, Jurow V, Stiletto R. Surgical treatment of acetabulum fractures in the elderly. Osteosynthesis or endoprosthesis. Unfallchirurg 2015;118:146-54. [Google Scholar | PubMed]
- 13.Tornkvist H, Schatzker J. Acetabular fractures in the elderly: An easily missed diagnosis. J Orthop Trauma 1993;7:233-5. [Google Scholar | PubMed]
- 14.Torngren TR, Szatkowski JP, Perez EA. Geriatric orthopaedics: Acetabular fractures in the elderly. Curr Orthop Pract 2011;22:392-9. [Google Scholar | PubMed]
- 15.Ernstberger H, Pieroh P, Höch A, Josten C, Herath SC, Osterhoff G, et al. Minimally displaced acetabulum fractures in geriatric patients: A comparison of open, percutaneous and non-operative treatment from the German pelvic injury register data. Eur J Trauma Emerg Surg 2021;47:1763-71. [Google Scholar | PubMed]
- 16.Tosounidis TH, Giannoudis PV. What is new in acetabular fracture fixation? Injury 2015;46:2089-92. [Google Scholar | PubMed]
- 17.Manson TT. Open reduction and internal fixation plus total hip arthroplasty for the acute treatment of older patients with acetabular fracture: Surgical techniques. Orthop Clin North Am 2020;51:13-26. [Google Scholar | PubMed]
- 18.Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: Two to twelve-year results. J Bone Joint Surg Am 2002;84:1-9. [Google Scholar | PubMed]










