Biomarkers in polytrauma patients as a clinical guide.
Dr. Pinaki Das, Department of Orthopaedics, Institute of Medical Sciences and SUM Hospital Campus II, Bhubaneswar, Khordha, Odisha, India. E-mail: docpinakidas@outlook.com
Introduction: Damage control orthopaedics (DCO) is a surgical concept that tends to control but not definitely repair the injuries caused to a polytrauma patient after trauma. Early total care (ETC) involves rapid stabilisation of the fracture after optimisation of retrieval conditions. In this study, a prospective randomized investigation will be done to correlate the clinical impression of DCO, ETC with the laboratory values of interleukin-6, Procalcitonin and C-reactive protein (CRP) in diaphyseal femoral fractures of polytrauma patients.
Materials and Methods: During this study period 40 patients with diaphyseal femoral shaft fractures meeting the inclusion criteria presented to our institute. After random allocation, 20 patients underwent surgery with External fixation with the purpose of DCO and other 20 patients underwent antegrade nailing according to ETC.
Results: There was a propensity of higher immuno-inflammatory response in the group subjected to primary stabilization of the femoral fractures than those with external fixation.
Conclusion: The correlation of multiple markers and their significance over time would help the clinician to take a decision for the type of treatment that can be offered to the patient.
Keywords: Early total care, damage control orthopaedics, immuno-markers, procalcitonin, C-reactive protein.
Road traffic accidents (RTAs) have increased exponentially in the past decade. In India, 4,37,396 RTAs were recorded in 2019 by the National Crime Record Bureau, and 1.3% resulted in death. 13.3% of all adult trauma cases are polytrauma cases with increased risk of mortality [1]. Trauma is the leading cause of death in those under 40 years of age [2]. Femur fractures account for around 18.3% of all fractures occurring due to trauma [3]. Diaphyseal femur fractures have an annual incidence of 10/100000 population/year [4]. Appropriate timing of surgery for these fractures, particularly when associated with polytrauma, has been an ongoing debate. The are two widely followed school of thoughts for the treatment of the multiply injured-early total care (ETC) and Damage Control Orthopaedics (DCO). DCO is a surgical concept that tends to control but not definitely repair the injuries caused to a polytrauma patient after trauma. The term “damage control” was initially described in the US Navy as the capacity of the ship to absorb damage and maintain mission integrity. In this modality, the definitive surgical management is usually performed after the normal physiological parameters such as core body temperature, coagulation indices, haemodynamic and respiratory status have come to an accepted base level [5]. In the DCO framework, three stages of management come into play. The first stage is of rapid resuscitation that addresses the imminent dangers such as catastrophic haemorrhage, blocked airway, and compromised ventilation. The second stage consists of resuscitation of the multiply injured in the intensive care setup till their condition is optimized. The final stage involves the definitive management of the fracture proper, once the generalized condition of the patient stabilizes [6]. DCO allows the patients’ condition to improve before enduring the additional trauma due to the surgical procedure. The most common modality used in diaphyseal fractures of the femur is temporary stabilisation with an external fixator [7]. Another prospective management of polytrauma patient is ETC. It involves rapid stabilisation of the fracture after optimization of retrieval conditions [8]. ETC is associated with decreased morbidity and mortality due to reduced incidence of pulmonary complications. It also prevents the abysmal demerits of delayed fracture stabilization such as prolonged immobilization and hospital stay [9]. Upon initial assessment of polytrauma patients after completion of early interventions, patients are put into one of the four categories to guide their further care. The parameters included for categorization are overall injury severity, presence of specific regional injuries, and haemodynamic status. The patients are further divided into the following categories – stable, borderline, unstable, and in extremis [10]. This guides the surgeon in deciding the best course of treatment for individual patients based on their physiological status. The cells of the human body are in constant communication with each other, both in normal physiological conditions as well as after any accidental or surgical trauma. There is a cascade of pro-inflammatory regulatory proteins that are produced and secreted by various cells of the body, mainly the neutrophil, macrophages, and monocytes, that has an important role in immune response to any traumatic event [11]. The development of systemic inflammatory response syndrome and multiple organ dysfunction syndrome directly correlates with the level of these pro-inflammatory markers. Interleukin-6 (IL-6), tumor necrosis factor-alpha, Procalcitonin, C-reactive protein (CRP), lipopolysaccharide-binding protein are some of the cytokine markers usually assessed to know the severity of the clinical condition of the multiply injured [12]. The “first hit” model suggests that the initial intense inflammatory reaction by both the innate and complementary immune system takes place after the primary trauma. Whereas in the “second hit” model, it is believed that the stimulus is usually less intense, but ironically the patient is vulnerable to secondary inflammatory insults that can lead to SIRS or multiorgan failure. The second insults are usually in the form of secondary infection, sepsis, and surgical operation [13]. Several studies have highlighted the issue of ETC to increase the cumulative insult to an already compromised physiological status of the patient.
In this study, a prospective randomized investigation will be done to correlate the clinical impression of DCO and ETC with the laboratory values of IL-6, Procalcitonin and CRP in diaphyseal femoral fractures of polytrauma patients. Furthermore, the level of these pro-inflammatory markers will be correlated with the clinical outcome.
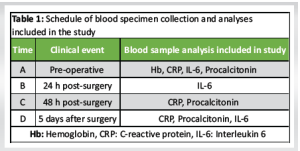
The investigation was designed as a prospective randomized interventional study. Skeletally mature patients with a unilateral diaphyseal fracture of the femur, between 2018 and 2021, admitted to a tertiary care centre, were included in this study. (Ethical Clearance) All the patients included were within the age group of 18–55 years who gave consent for the surgery. The patients included had ISS score >16 with thoracic AIS Score <4 who presented to the emergency and Outpatient Department of the institution. The patients who were critical at the time of presentation, belonging to unstable or in extremis category [10], having Glasgow Coma Scale (GCS) <5, severe hypothermia, systolic blood pressure <90 mm Hg, severe head injury warranting emergency intervention, penetrating chest and abdominal trauma, morbid obesity (body mass index >35 kg/m2), Gustillo Anderson type IIIC wound, bilateral femur fractures, pregnant women, open physeal growth plate and patients with pathological fractures were excluded from the study. Those who were discharged before 7 days after surgery were also excluded from the study. After preliminary resuscitation by advanced trauma life support protocol, patients or their family members were informed about the further surgical plan, including its possible complications, prognosis, etc., and informed consent was taken. Full-length radiograph of the affected thigh in two planes was taken. The patients were also subjected to standard trauma series radiographs that included X-rays of the chest posteroanterior view, pelvis anteroposterior (AP) view, and AP and lateral views of the cervical and lumbosacral spine. According to availability, the patients were temporarily immobilised with Spad traction with Bohler Braun Splint or Thomas Splint, awaiting surgery. The clinical status of the patients and any complications were monitored and documented throughout the course of the hospital stay. As all these patients belonged to polytrauma category according to ISS, immediate airway management, ventilation and bleeding were initially addressed. Intravenous fluids, preferably crystalloid or colloid solution, were administered as required. Catheterization was done routinely to assess the fluid balance. Patients’ demographic details, side of fracture, soft-tissue integrity, mechanism of injury, ISS Score, associated injuries and time from injury to admission were documented. The fracture anatomy was classified based on AO/OTA classification preoperatively. Patients underwent Pre-Anaesthetic check-up before they were posted for surgery. All cases underwent surgery with application of external fixator ( DCO – group A) or femur IMN (ETC–Group B) within 48 h of admission. Patients were randomized to either primary femoral antegrade nailing or damage control with uniplanar external fixation followed by secondary nailing, after they met the inclusion criteria. The two main treatment arms in this study, i.e., DCO and primary intramedullary femoral antegrade nailing, were compared based upon patients’ demographics, intensive care period, development of acute respiratory distress syndrome, and blood parameters such as IL-6, procalcitonin, and CRP post-intervention. At our center, antegrade femoral nail was done as per standard nailing techniques. All the antegrade femoral nails were based on the pyriform fossa entry type. Femur intramedullary nails of size 9–12 mm diameter of stainless steel/titanium variety from Nebula Surgicals (Cat No. 156.13/T156.13) were used in all cases. In cases where external fixation was done, AO type external fixator from Nebular Surgical (Cat No. 202) was used using standard external fixation techniques. The timing of blood collection and the specific tests done are recorded in Table 1.
Post-surgery the patients were monitored as per status. The number of days of ICU stay, complications and interventions required and the total duration of hospital stay was recorded.
Haemoglobin (Hb) was measured using peripheral venous blood sample. The sample was collected in tubes and Vacutainer tubes containing ethylenediaminetetraacetic acid (K2EDTA). Blood was collected for evaluation for IL-6 in an K2EDTA vial and sent for analysis pre-operatively and post-operative day 1, 2, and 5. The tubes were immediately sent to the laboratory to be processed. Serial blood samples were collected as per the schedule given in Table 1. The samples were collected in tubes and vacutainer tubes containing ethylenediamenetetraacetic acid. Data were entered using Microsoft Excel software (Microsoft Office Excel 2010). Continuous variables are presented as means. Categorical and nominal variables are presented as percentages. This study was approved by the Institutional Ethical Review Board.
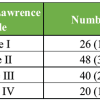
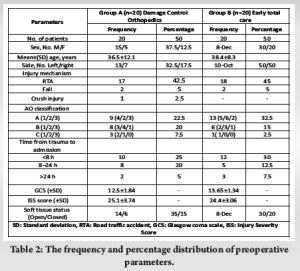
During this study period 40 patients with diaphyseal femoral shaft fractures meeting the inclusion criteria presented to our institute. After random allocation, 20 patients underwent surgery with External fixation with the purpose of DCO, collectively referred as Group A. The other 20 patients were allocated group B. Early absolute care was done in them with antegrade reamed intramedullary femoral nail. The mean age of patients in Group A and Group B was 35.5 years and 38.4 years respectively and did not differ significantly (P = 0.59). There was a male preponderance in both the study groups. Other general data were collected from the patients regarding side of injury, type, mechanism of injury, time since trauma to admission, ISS score, GCS, soft-tissue cover (Table 2). Both treatment groups were comparable in terms of general data preoperatively.
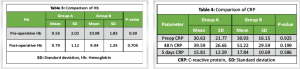
The comparison of pre-operative and post-interventional Hb values was done between both the groups, and it was found that the group subjected to ETC had a drop in mean Hb level, whereas patients treated with DCO had a slight increase (Table 3 and Fig. 1).
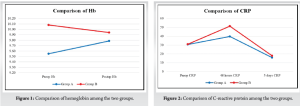
CRP values were analyzed preoperatively, at 48 h and at 5 days. There was an increase in mean CRP values in both the groups at 48 h, but at 5 days of presentation Group B (DCO) had a higher mean CRP level as compared to Group A (Table 4 and Fig. 2).
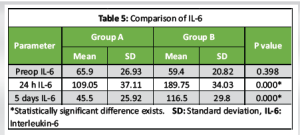
When IL-6 values were put into comparison similar to CRP, there was an increase of mean IL-6 values in both the groups at 48 h, but at 5 days, Group B (DCO) had a significantly higher mean IL-6 level as compared to Group A (P = 0.000) (Table 5 and Fig. 3).
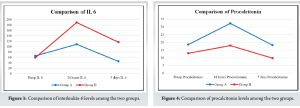
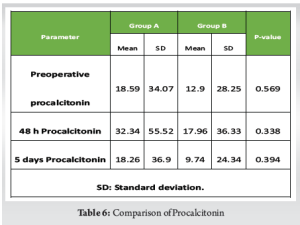
Serum procalcitonin analysis showed an initial increase of mean values in both the groups whereas at 5 days, the ETC group had a lower mean procalcitonin level that did not differ statistically (P = 0.394) (Table 6 and Fig. 4).
The effect of temporizing intervention strategies for optimum outcome in critically injured polytrauma patients has been satisfying for a considerable amount of time [14]. However, there are conflicts in the available literature regarding initial surgical stabilization or its avoidance should a secondary insult be avoided [8]. There are limited studies in the literature to study the effect of early external fixation versus ETC on the level of inflammatory markers in polytrauma patients. Hans Cristoph Pape conducted a prospective randomized trial in 2003 and concluded that a sustained inflammatory response was measured after primary (<24 h) intramedullary femoral instrumentation, but not after initial external fixation or after secondary conversion to an intramedullary implant [15]. In a longitudinal, prospective, and observational study by Husebye et al. in 2012 could not demonstrate any major IMN-related impact on inflammatory markers or cardiopulmonary function parameters [16]. The current study is one of its kind to evaluate the effect of DCO and ETC over serum inflammatory markers, taking into consideration easily evaluated CRP, IL-6, and procalcitonin levels. To negate the possibility of bias among the two interventional arms, double blinding was done where both the investigator and the patients were unaware as to which group a particular patient was being assigned to. The results can be summarized as there was a propensity of higher immunoimflammatory response in the group subjected to primary stabilization of the femoral fractures than those with external fixation. As our exclusion criteria did not include patients with severe multiorgan injury, so results obtained were more homogenous. In contrary to other studies conducted, the parameters that were chosen for this particular study were more inclusive and responsive to the interventions that were carried out [17]. Trauma-induced suppression of a responsive circulating and stationary immune system causes altered immunoglobulin secretion, B-cell response, and cytokine release. This has been validated by multiple past studies [18]. At various post-traumatic time intervals, different levels of cytokine responses can be recorded, leading to a disparity of the levels of immunomarkers [19]. The IL-6 levels in the present study were in a comparable level to which is associated with SIRS [20]. IL-6 level increase has been generally associated in invasive orthopedic procedures. Pape et al. [15] investigated patients with femoral shaft fractures and found that venous IL-6 peak levels 24 h after IMN and when the femoral fracture was initially stabilized with external fixation and secondarily converted to an intramedullary implant, no IL-6 increase was observed. Although patients in the external fixation group exhibited higher levels of head trauma than those who underwent intramedullary nailing, patients in stable condition who received external fixation had a longer duration on a ventilator than those who received intramedullary nailing, even after controlling for differences in initial injury severity. Hence, external fixation should not be recommended for patients in stable condition as it produces no added benefits in terms of clinical complications and seems to delay clinical recovery. Another factor that might have played a role in documenting a more reliable immunological marker variance is the number of patients included in the study. This would have led to significant statistical differences. One patient among the study participants who underwent external fixation developed pneumonia 7 days postoperatively. No morbidity was reported. Three patients had an incidence of pin tract infection, which was managed conservatively and appropriate pin tract dressing.
The existing evidence of all relevant serum markers has been evaluated in this study. To be worthy of being called as an ideal marker, predicting the outcome accurately, is unfortunately not available. As multiple complex molecular mechanisms play a role in a polytrauma patient, a single marker cannot always predict the outcome. Hence, the correlation of multiple markers and their significance over time would help the clinician to take a decision for the type of treatment that can be offered to the patient. Further studies in this area are warranted, and new diagnostic modalities would definitely help to provide more accurate and innovative treatment protocols to the multiple injured patients.
The approach to management of polytrauma patients is constantly evolving, with drastic change seen over the last decades. The aim to stabilize the major fractures as early as physiologically safe is a concept built on the symbiosis of both Early Total Care and Damage Control Orthopaedics. As understanding of physiological parameters increase, their use in adapting patient specific treatment protocols is being studied.
References
- 1.Clement N, Regina DL, Kundavarum PP. A retrospective study on the profile and outcome of polytrauma in the emergency department. Curr Med Issues 2018;16:56-9. [Google Scholar | PubMed]
- 2.World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar | PubMed]
- 3.Kalsotra N, Mahajan V, Kalsotra G, Sharma S, Raina P, Gupta A. Epidemiology of polytrauma in a tertiary care centre. J Evol Med Dent Sci 2016;5:3021. [Google Scholar | PubMed]
- 4.Weiss RJ, Montgomery SM, Al Dabbagh Z, Jansson KA. National data of 6409 Swedish inpatients with femoral shaft fractures: Stable incidence between 1998 and 2004. Injury 2009;40:304-8. [Google Scholar | PubMed]
- 5.Shapiro MB, Jenkins DH, Schwab CW, Rotondo MF. Damage control: Collective review. J Trauma 2000;49:969-78. [Google Scholar | PubMed]
- 6.Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg Am 2000;82:781-8. [Google Scholar | PubMed]
- 7.Pape HC, Rixen D, Morley J, Husebye EE, Mueller M, Dumont C, et al. Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg 2007;246:491-9. [Google Scholar | PubMed]
- 8.Bone LB, Johnson KD, Weigelt J, Scheinberg R. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am 1989;71:336-40. [Google Scholar | PubMed]
- 9.Riska EB, Von Bonsdorff H, Hakkinen S, Jaroma H, Kiviluoto O, Paavilainen T. Primary operative fixation of long bone fractures in patients with multiple injuries. J Trauma 1977;17:111-21. [Google Scholar | PubMed]
- 10.Giannoudis PV. Surgical priorities in damage control in polytrauma. J Bone Joint Surg Br 2003;85:478-83. [Google Scholar | PubMed]
- 11.Granger DN, Kubes P. The microcirculation and inflammation: Modulation of leukocyte-endothelial cell adhesion. J Leukoc Biol 1994;55:662-75. [Google Scholar | PubMed]
- 12.Giannoudis PV, Pape HC, Cohen AP, Kretteck C, Smith RM. Systemic effects of femoral nailing: From Küntscher to the immune reactivity era. Clin Orthop Relat Res 2002;404:378-86. [Google Scholar | PubMed]
- 13.Cipolle MD, Pasquale MD, Cerra FB. Secondary organ dysfunction. From clinical perspectives to molecular mediators. Crit Care Clin 1993;9:261-98. [Google Scholar | PubMed]
- 14.Rotondo MF, Schwab CW, McGonigal MD, Phillips GR 3rd, Fruchterman TM, Kauder DR, et al. ‘Damage control’: An approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993;35:375-82. [Google Scholar | PubMed]
- 15.Pape HC, Grimme K, Van Griensven M, Sott AH, Giannoudis P, Morley J, et al. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: Prospective randomized analysis by the EPOFF study group. J Trauma 2003;55:7-13. [Google Scholar | PubMed]
- 16.Husebye EE, Lyberg T, Opdahl H, Aspelin T, Støen RO, Madsen JE, et al. Intramedullary nailing of femoral shaft fractures in polytraumatized patients. A longitudinal, prospective and observational study of the procedure-related impact on cardiopulmonary- and inflammatory responses. Scand J Trauma, Resusc Emerg Med 2012;20:2. [Google Scholar | PubMed]
- 17.Pape HC, Remmers D, Grotz M, Schedel I, Von Glinski S, Oberbeck R, et al. Levels of antibodies to endotoxin and cytokine release in patients with severe trauma: Does posttraumatic dysergy contribute to organ failure? J Trauma 1999;46:907-13. [Google Scholar | PubMed]
- 18.Brooks K, Yuan D, Uhr J, Krammer PH, Vitetta ES. Lymphokine-induced IgM secretion by clones of neoplastic B cells. Nature 1983;302:825-6. [Google Scholar | PubMed]
- 19.Pape HC, Van Griensven M, Rice J, Gänsslen A, Hildebrand F, Zech S, et al. Major secondary surgery in blunt trauma patients and perioperative cytokine liberation: Determination of the clinical relevance of biochemical markers. J Trauma 2001;50:989-1000. [Google Scholar | PubMed]
- 20.Giannoudis PV, Harwood PJ, Loughenbury P, Van Griensven M, Krettek C, Pape HC. Correlation between IL-6 levels and the systemic inflammatory response score: Can an IL-6 cutoff predict a SIRS state? J Trauma 2008;65:646-52. [Google Scholar | PubMed]