In post-operative microdiscectomy patients, particularly those with CLL and concurrent viral infections, early recognition and prompt intervention of delayed spontaneous spinal hematoma is crucial to prevent permanent neurological deficits.
Dr. Rahul S Agrawal, Department of Orthopaedics, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India. E-mail: rahuldoctor.spine@gmail.com
Introduction: Spontaneous spinal hemorrhage in dengue fever is extremely rare. We report a case of post-operative microdiscectomy complicated by delayed (>72 h) spontaneous lumbar epidural hematoma leading to cauda equina syndrome, having severe thrombocytopenia with dual viral infection (dengue and chikungunya) in a known case of chronic lymphoid leukemia (CLL). The patient was managed with transfusion of platelets followed by revision surgery with the evacuation of hematoma with lumbar decompression, following which the patient improved gradually. Although cases of symptomatic spinal epidural hematoma and post-viral infection have been reported, post-microdiscectomy together with CLL is not reported in literature.
Case Report: A 62-year-old male with known hypertension and CLL presented with severe low back pain and left anterior thigh radiation, who underwent uneventful microscopic discectomy for L2–L3 disc sequestration. On post-operative day 4, the patient developed cauda equina syndrome with concurrent dengue and chikungunya infections, and magnetic resonance imaging revealed an extradural hematoma at L3–L5 level. After medical optimization with platelet transfusions and steroids, the patient underwent emergency surgical evacuation of the hematoma.
Conclusion: In post-operative microdiscectomy, delayed spontaneous spinal hematoma with cauda equina syndrome having dual viral fever (dengue and chikungunya) with CLL is a rare complication. Failure to recognize can lead to devastating outcomes with permanent neurological impairment. Prompt medical optimization following close clinico-serological monitoring with early surgical evacuation is needed. Early diagnosis with intervention can significantly improve the neurological outcome.
Keywords: Spinal epidural hematoma, dengue fever, chikungunya, microdiscectomy, thrombocytopenia, leukemia.
Symptomatic spinal epidural hematoma (SSEH) post-microdiscectomy is a rare complication of spinal surgery and may require reoperation if it is associated with neurological complications [1]. We present here a case report of post-operative microdiscectomy presenting as delayed spinal epidural hematoma (>72 h) with cauda equina syndrome with thrombocytopenia having chronic lymphoid leukemia as a risk factor and our diagnosis with management of this unique complication which gradually improved patient outcome.
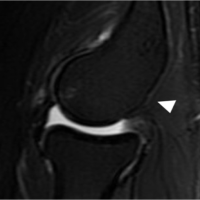
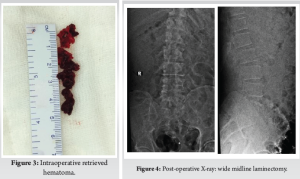
A 62-year-old male presented to the outpatient department with low back pain (visual analog score [VAS] 6/10) with left anterior thigh radiation (VAS 8/10) associated with tingling in a known case of hypertension and chronic lymphoid leukemia (CLL). On neurologic examination, gait was antalgic while the femoral nerve stretch test was positive and straight leg raising test was negative. There was no lower limb power weakness while sensations and deep tendon reflexes were intact. There was no recent history of fever, bleeding diathesis, or anti-coagulant intake. Provisional diagnosis of lumbar radiculopathy was considered. Blood investigations revealed normal platelets (133000) with raised total leukocyte count (TLC) (188810). Lumbar spine anteroposterior and lateral dynamic views had no radiological instability (Fig. 1). while magnetic resonance imaging (MRI) revealed L2–L3 inferior disc sequestration with disc desiccation compressing the exiting L3 nerve root (Fig. 2). The patient was posted for microscopic discectomy and procedure was uneventful and sequestered disc fragments were retrieved with complete decompression of the nerve root. The patient had significant improvement in radiculopathy in post-operative (VAS 1/10) and was comfortably walking the next day. Routine hemogram on post-operative day (POD) 1 showed TLC 133760 while platelets were 94000. On POD 3, the patient had two episodes of fever spikes with body temperature >100 F. On POD 4, the patient had sudden complaints of perineal numbness with bowel and bladder incontinence with right posterior thigh radiation while neurology weakness of right ankle dorsiflexion and extensor halluces longus (EHL) grade 1/5 with hypoesthesia over right L5 dermatome was noted. Blood counts showed thrombocytopenia (89000) with raised TLC (127630). On tropical fever panel test by polymerase chain reaction (PCR) method, the patient tested positive for dengue and chikungunya, while he was negative for plasmodium, rickets, and Salmonella. The patient tested negative for dengue immunoglobulin (Ig)G and IgM antibodies. Blood sugar, serum creatinine, serum electrolytes, serum bilirubin, and aminotransferases were normal while total proteins slightly reduced. Bleeding time, clotting time, and activated partial thromboplastin time (APTT) were raised. Ultrasonographic examination of the abdomen revealed mild hepatosplenomegaly. MRI of the lumbar spine was suggestive of extradural hematoma at L3–L4, L4–L5 vertebral level causing cord compression (Fig. 3). Diagnosis was revised as post-microdiscectomy spontaneous delayed hematoma (>72 h) with cauda equina syndrome and the patient was treated symptomatically for dengue fever. Intravenous methylprednisolone 500 mg was given. Multiple transfusions of single donor platelet are given to raise the platelets above the critical level of 50,000/cu mm and fresh frozen plasma with partial thromboplastin time with kaolin (PTTK)/APTT mixing studies returning near to normal values. For leukemia, the patient was posted after oncologist clearance. The patient was posted on POD 4 for emergency evacuation.


Surgical procedure
Midline incision was extended and L3–L5 wide laminectomy with hematoma evacuation was done, and drain was placed in situ. The thecal sac was pulsatile. Intraoperatively drain was also kept in situ to avoid further hematoma if any.
Post-operative course
Post-operative period was uneventful with improvement in constitutional symptoms, right ankle dorsiflexion, and EHL power to grade 3/5. Deep vein thrombosis (DVT) prophylaxis was given in form of DVT pumps until lower limb strengthening exercises were started. Post-operative radiograph confirmed wide laminectomy. (Fig. 4) Foley’s catheter was kept in situ on discharge and removed after 1 month postoperatively. The patient was discharged on day 15 in stable condition with training in limb strengthening exercises and was made to stand bedside. During 6-month follow-up period, the patient showed improvement in power of ankle dorsiflexion and EHL by 3 grade and bowel bladder symptoms improved. Following 1 year, the patient had resumed his daily activities and was walking without support.
Symptomatic spinal epidural hematoma (SSEH) post-microdiscectomy is a rare complication of spinal surgery and may require reoperation if it is associated with neurological complications.[1] Many etiologies have been associated with spinal hematoma such as traumatic, bleeding diathesis, drug-induced anticoagulation, lumbar puncture, epidural anesthesia, spinal surgery, leukemia, and viral infection [2-5]. Even spontaneous spinal hematoma, following dengue fever is a rare complication [6]. The most severe sequelae of dengue fever are dengue hemorrhage and dengue shock syndrome [3]. Neurological manifestations have been reported in 0.5–20% cases while it accounts for <1% of total systemic manifestations [7]. Gulati and Maheshwari previously reported atypical neurological manifestations in the form of encephalitis, Guillain–Barre syndrome, myelitis, thrombosis, intracranial hemorrhage, mono/polyneuropathy, hypokalemia leading to quadriparesis in dengue fever, but delayed spinal hematoma due to dual viral fever is very rare [7]. Kumar et al. also reported intracranial hemorrhage as a complication of spinal epidural hematoma following spine surgery [8]. SSEH is one of the most threatening complications of spine surgery having incidence of 0.52% [9]. SSEH is defined as compression of thecal sac, cauda equine, or nerve roots leading to motor or sensory deficit is a rare and threatening complication of spine surgery [9]. It has been defined as early onset (<72 h) or delayed onset (>72 h) based on post-operative time of onset in which the incidence of delayed is less common [9]. Our case had post-operative microdiscectomy, delayed onset SSEH leading to cauda equina syndrome. Preoperatively, there were no signs of dengue fever clinically as well as on blood parameters while the patient was retrospectively suspected to be in the incubation period. Wang et al. reported risk factors for SSEH such as obesity, multilevel surgery, revision surgery, smoking, and post-operative anticoagulation therapy, however none of these reported factors were seen in the presented case report. [4,10,11]. Malignancy-associated spinal epidural hematoma was reported previously in two cases. Bauduceau et al. reported a case of secondary onset in the blast crisis phase of chronic myeloid leukemia that interrupted medication for 3 years [11]. While there is a scarcity of literature for CLL associated with hematoma, CLL as a risk factor for SSEH cannot be ruled out. In our case, we waited for single donor platelets to rise the platelets above the critical level of 50,000/cu mm and gave fresh frozen plasma with PTTK/APTT mixing returning near-to-normal values. High degree of suspicion is required in perioperative period following spine surgery with relevant investigation to tackle rare complications of delayed SSEH following spine surgery caused by dual viral dengue and chikungunya in patients residing in endemic areas. Prompt medical optimization is needed with close watch on clinicoserological parameters followed by early surgical evacuation if signs of compression are present clinically, further confirmed by MRI imaging. Furthermore, misdiagnosis of dengue-related non-compressive myelopathy can delay the initial line of treatment and surgical evacuation which may lead to irreversible neurodeficit. Further studies are needed about the management of such rare complication.
In post-operative microdiscectomy, delayed spontaneous spinal hematoma with cauda equina syndrome having dual viral fever (dengue and chikungunya) with CLL is a rare complication. Failure to recognize can lead to poor outcomes with permanent neurological impairment. Prompt medical optimization following close clinic-serological monitoring with early surgical evacuation is needed. Early diagnosis with intervention can significantly improve the neurological outcome.
Early recognition of delayed spontaneous spinal hematoma in post-operative period is crucial, as delayed diagnosis can result in permanent neurological damage. Optimal outcomes depend on prompt medical management with close clinical and serological monitoring, followed by timely surgical evacuation of the hematoma.
References
- 1.Chen Q, Zhong X, Liu W, Wong C, He Q, Chen Y. Incidence of postoperative symptomatic spinal epidural hematoma requiring surgical evacuation: A systematic review and meta-analysis. Eur Spine J 2022;31:3274-85. [Google Scholar | PubMed]
- 2.Awad JN, Kebaish KM, Donigan J, Cohen DB, Kostuik JP. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br 2005;87:1248-52. [Google Scholar | PubMed]
- 3.Maheshwari V, Kumar S, Kumar A, Kumar A. Spontaneous subdural hematoma of dorsal spine secondary to dengue fever: A rare case report with review of literature. Asian J Neurosurg 2019;14:550-2. [Google Scholar | PubMed]
- 4.Nojiri H, Kim S, Tsuji T, Uta S. Spontaneous spinal epidural hematoma as the initial presentation of leukemia. Eur Spine J 2009;18 (Suppl 2):220-3. [Google Scholar | PubMed]
- 5.Lee JI, Hong SC, Shin HJ, Eoh W, Byun HS, Kim JH. Traumatic spinal subdural hematoma: Rapid resolution after repeated lumbar spinal puncture and drainage. J Trauma 1996;40:654-5. [Google Scholar | PubMed]
- 6.Jha S, Ansari MK. Dengue infection causing acute hypokalemic quadriparesis. Neurol India 2010;58:592-4. [Google Scholar | PubMed]
- 7.Gulati S, Maheshwari A. Atypical manifestations of dengue. Trop Med Int Health 2007;12:1087-95. [Google Scholar | PubMed]
- 8.Kumar J, Kumar A, Gupta S, Jain D. Dengue hemorrhagic fever: An unusual cause of intracranial hemorrhage. BMJ Case Rep 2009;2009:bcr2006100909. [Google Scholar | PubMed]
- 9.Chen Q, Zhong X, Liu W, Wong C, He Q, Chen Y. Incidence of postoperative symptomatic spinal epidural hematoma requiring surgical evacuation: A systematic review and meta analysis. Eur Spine J 2022;31:3274-85. [Google Scholar | PubMed]
- 10.Wang L, Wang H, Zeng Y, Zhong W, Chen Z, Li W. Delayed onset postoperative spinal epidural hematoma after lumbar spinal surgery: Incidence, risk factors, and clinical outcomes. Biomed Res Int 2020;2020:8827962. [Google Scholar | PubMed]
- 11.Bauduceau O, De Revel T, Fogelman J, Amadou S, Souleau B, Nedellec G. Spontaneous hematoma of the iliac psoas muscle in chronic myeloid leukemia. A case report. Ann Med Interne [Paris] 2003;154:183-6. [Google Scholar | PubMed]