Preservation of the proximal femoral stem with fracture stabilization offers a novel approach for managing atypical periprosthetic femoral fractures with stem breakage.
Nicholas Frappa, Jacobs School of Medicine and Biomedical Sciences, Buffalo, NY, USA. E-mail: nmfrappa@buffalo.edu
Introduction: As the number of total hip arthroplasty (THA) procedures continues to increase annually, periprosthetic femoral fractures (PFFs) have become a more common and significant complication. These fractures present a unique challenge due to the presence of the prosthetic implant, which may complicate the healing process. Atypical femur fractures (AFFs) are a subset of fractures that frequently occur with minimal trauma, often in patients who have been on prolonged bisphosphonate therapy. Although PFFs are excluded from the AFF definition, PFFs that otherwise meet the criteria have been termed atypical PFFs (APFFs). While APFFs are a growing area of interest, there is limited literature on their management, particularly when associated with femoral stem breakage. This case report presents the second reported instance of an APFF with femoral stem breakage, but uniquely, it is the first to involve the preservation of the proximal stem with isolated removal of the distal portion.
Case Report: An 88-year-old female with multiple comorbidities, including osteoporosis and a history of bisphosphonate therapy, presented with an APFF of the right femur following a ground-level fall. One year prior, she had undergone uncomplicated THA with a long cylindrical, fully porous-coated femoral stem. Radiographs revealed a transverse fracture at the subtrochanteric region, lateral cortical thickening, and femoral stem breakage. Given the patient’s medical history and the complexity of the fracture, revision surgery was indicated. Surgical intervention included the preservation of the proximal femoral stem and the removal of the distal stem segment, combined with periprosthetic plate fixation and cortical strut allograft for stabilization.
Conclusion: This case highlights the importance of individualized surgical planning in the management of APFFs, particularly those involving stem breakage. By preserving the proximal stem, a less invasive approach was achieved, minimizing surgical morbidity and supporting optimal fracture healing. The case underscores the potential benefit of preserving the femoral stem when appropriate, a strategy not widely explored in current literature. The findings contribute to the ongoing discussion of surgical options for APFFs and offer valuable guidance for future treatment approaches, especially as THA and bisphosphonate use continue to rise.
Keywords: Atypical periprosthetic femoral fracture, bisphosphonate therapy, femoral stem breakage, hip arthroplasty, fracture fixation, osteoporosis, surgical management.
As the number of total hip arthroplasties (THA) continues to increase annually, periprosthetic femoral fractures (PFFs) have become a more common and significant complication [1]. These fractures present a unique challenge due to the presence of the prosthetic implant, which may complicate the mechanical properties of the bone and the healing process, as well as the patient factors that may affect non-surgical and surgical treatment decisions. Atypical femur fractures (AFFs) are a subset of fractures that occur with minimal trauma, often in patients who have been on prolonged bisphosphonate therapy [2,3]. The American Society for Bone and Mineral (ASBMR) Research Task Force 2013 Revised Case Definition defines an AFF as meeting at least four of five criteria: (1) minimal trauma (fall from standing height or less), (2) a transverse fracture originating from the lateral cortex, (3) a complete or incomplete fracture involving the lateral cortex, (4) a non-comminuted or minimally comminuted fracture, and (5) localized periosteal or endosteal thickening of the lateral cortex [3]. While PFFs are excluded from the ASBMR AFF definition, PFFs that otherwise meet the criteria have been termed atypical PFFs (APFFs) [3,4]. While APFFs have become an emerging topic of interest, there is a paucity in the literature regarding their management with only one prior case being documented for APFF with femoral stem breakage [4-8]. We present the second reported case of an APFF with stem breakage, but uniquely, it is the first to involve the isolated removal of the distal portion of the stem. This case report highlights the challenges of managing such fractures and discusses the tailored surgical approach required for this patient, offering a new perspective on surgical management.
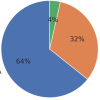
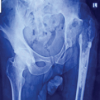
The index patient is an 88-year-old female with a body mass index (BMI) of 21.3 and a history of multiple comorbidities, including hyperlipidemia, hypertension, cerebrovascular accident, chronic kidney disease stage III, diabetes mellitus, and osteoporosis with bisphosphonate therapy. One year prior, she underwent an uncomplicated right total hip arthroplasty (THA) with a long cylindrical, fully porous-coated femoral stem. The prior THA was uncomplicated, and she had no prodromal symptoms. She presented following a ground-level fall, resulting in an APFF of the right femur. Radiographic findings revealed a transverse fracture through the subtrochanteric region of the femur, with breakage of the cylindrical femoral stem (Fig. 1a and b). Interestingly, the fracture also demonstrated lateral cortical thickening, a feature commonly associated with AFFs in patients on bisphosphonate therapy [3]. Although the fracture in this case met all five criteria, the ASBMR definition excludes periprosthetic fractures from the AFF definition [3]; therefore, this case demonstrates an APFF.

The patient’s periprosthetic fracture of the femoral stem, features of an APFF, and associated non-union necessitated surgical intervention. Preoperative screening for Influenza A, Influenza B, and severe acute respiratory syndrome coronavirus 2 was negative. The preoperative white blood cell count was elevated at 15,200 cells/μL, though there were no clinical signs of infection. After explaining the risks and obtaining consent, the patient elected to proceed with revision surgery.
Surgical treatment and post-operative care
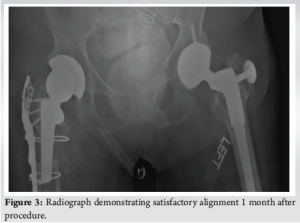
The surgical approach began with an incision on the lateral aspect of the right leg, with careful dissection through the iliotibial band, which was incised longitudinally. A soft vastus approach to the femoral shaft was utilized, reflecting the vastus lateralis in an L-shaped flap. During the procedure, a transverse fracture of the right proximal femur was discovered at the subtrochanteric region, which involved the cylindrical stem. Both the proximal and distal portions of the femoral stem were found to be well-fixed with excellent bone ingrowth. Due to the significant morbidity that would result from removing the proximal portion of the femoral stem, the decision was made to only remove the distal portion. A cylindrical trephine was used to core out the distal segment of the stem, with minimal bone loss. In addition, a 15 mm sliver of bone was removed from the distal portion of the proximal femoral stem, which was intussuscepted into the intramedullary canal of the distal femur. This achieved an excellent apposition of the bony surfaces while maintaining rotational alignment. A long periprosthetic proximal femoral plate with a trochanteric extension was placed along the lateral cortex of the femur to span the fracture site. Subsequently, a cortical strut allograft was applied along the posterior aspect of the femur. Proximal fixation was achieved using multiple circumferential cables, as well as both non-locking and locking screws with compression across the fracture site, provisionally maintained using a clamp. Distal fixation was reinforced with additional bicortical screws and cables. Intraoperative radiographs demonstrated optimal reduction of the fracture, with the femoral stem tip positioned below the fracture site (Fig. 2). The lateral proximal femoral plate spanned the fracture site at over 1.5 times the canal diameter, in accordance with conventional recommendations for bypassing the fracture, ensuring stability and proper alignment. Postoperatively, the patient was made toe-touch weight-bearing on the right leg for the first 6 weeks, with progressive weight bearing as tolerated during the following 6 weeks. Physical therapy continued throughout this period (Fig. 3).

Outcome
Six-month post-operation, the patient reported no discomfort in the right hip and was able to return to her nursing facility. X-rays showed that all hardware was intact and demonstrated good bone healing.
This case report is the first to discuss the preservation of the proximal portion of a long cylindrical, fully porous-coated femoral stem in the setting of an APFF with periprosthetic fracture stabilization through a long periprosthetic proximal femoral plate with a cortical strut allograft. Femoral stem fractures after THA are rare but present significant challenges. The incidence of stem fractures has been reported to range from under 0.1% to 3.4%, with factors such as male sex, younger age, and higher BMI being associated with an increased risk [7]. These risk factors contrast with our patient, who was an elderly female, with a normal BMI, making her case an unusual presentation. Stem fractures can complicate the healing process and require careful decision-making regarding whether to remove or preserve the stem [7]. Lee et al. [8] is the only reported case of surgical management of an APFF though the authors did not exchange either stem component, instead stabilizing the original with plates. This highlights the absence of consensus on how best to approach femoral stem breakage in APFFs, furthering the need for future studies to investigate the optimal surgical strategies for these complex, although rare fractures. This case underscores the growing need to better understand and address the management of APFFs. APFFs have emerged as a significant complication in patients with THA, particularly those on long-term bisphosphonate therapy. Bisphosphonates, while effective in treating osteoporosis, are linked to an increased risk of APFF [6,9-11]. Consequently, the specific challenges of managing APFFs are less frequently studied. While some studies have discussed fracture fixation strategies for AFFs and PFFs, few have provided detailed guidance on managing APFFs. Zhang et al. [12] discussed fracture management of periprosthetic fractures in the setting of cylindrical femoral stems. However, the approaches discussed involved removal of the entirety of the femoral prosthesis, while the proximal stem was preserved in our case in the setting of an APFF. While intramedullary nailing is currently regarded as the first-line surgical treatment for AFFs, this is precluded by the presence of the prosthetic stem in PFFs and APFFs alike [13,14]. A literature review conducted by Troiano et al. [15] discussed surgical management for both complete and incomplete APFFs. They determined that optimal management for APFFs included a long-locked plate with the optional additions of cerclages and structural grafts. However, the study [15] did not provide management strategies in APFFs with stem breakage. By preserving the proximal femoral stem, this is a potentially promising strategy that helps provide the foundation for establishing standardized treatment protocols for APFFs. Recognizing an APFF is crucial, as these fractures are associated with longer healing times and higher complication rates compared to typical fractures [10,11]. As the incidence of THA and bisphosphonate use increases [2,3], the importance of understanding and effectively managing APFFs as their incidence will likely continue to grow. The challenge remains in a balanced fracture stabilization construct with the preservation of the implant and surrounding bone to ensure an optimal healing environment while minimizing complications and morbidity to the patient. In our case, the patient’s baseline functional status was limited to short-distance ambulation in a nursing facility with a rolling walker. Given her advanced age, comorbidities, and functional limitations, the decision to preserve the proximal femoral stem was influenced by the need to minimize surgical morbidity. The preservation of the proximal stem allowed for a less invasive procedure than if both components were removed, which was crucial for her recovery and rehabilitation, considering her limited mobility and overall health status. However, it is important to note that such an approach may not be suitable for younger or more active patients who could potentially tolerate proximal and distal stem removal and revision arthroplasty. The decision-making process in this case was further complicated by the nature of the cylindrical stem, as the extent and location of bone ingrowth played a significant role in determining the feasibility of stem preservation. This unique factor underscores the need for careful consideration of both the patient’s clinical status and the prosthetic stem design when making surgical decisions in cases of APFF with stem breakage.
APFFs present a unique and evolving challenge in orthopedic surgery, especially in the context of patients with a history of bisphosphonate use. This case underscores the unique presentation and surgical management of a patient with an APFF with stem breakage. By preserving the proximal femoral stem and using a combination of fixation techniques, this patient’s fracture was successfully treated with good 6-month follow-up data.
This case report introduces a novel technique for managing APFFs with femoral stem breakage by preserving the proximal femoral stem. It highlights the potential benefits and challenges of this approach in patients with long-term bisphosphonate therapy.
References
- 1.Sassoon AA, Taylor JM, Jimenez E, Stancil R, Cannady D, De A. Periprosthetic fractures: A rising tide of hip arthroplasty failure noted in the American joint replacement registry and the preventative role of cemented stems. J Arthroplasty 2024;39:S454-8. [Google Scholar | PubMed]
- 2.Lindahl H, Garellick G, Regner H, Herberts P, Malchau H. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am 2006;88:1215-22. [Google Scholar | PubMed]
- 3.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1-23. [Google Scholar | PubMed]
- 4.De Cicco A, Toro G, Oliva F, Tarantino U, Panni AS, Maffulli N. Atypical periprosthetic femoral fractures of the hip: A PRISMA compliant systematic review. Injury 2021;52:2407-14. [Google Scholar | PubMed]
- 5.Mondanelli N, Facchini A, Troiano E, Muratori F, Bottai V, Giannotti S. Periprosthetic atypical femoral fractures exist: A retrospective study at a single institution. Prevalence on 115 periprosthetic femoral fractures around a primary hip stem. J Arthroplasty 2021;36:2189-96. [Google Scholar | PubMed]
- 6.Leclerc JT, Michou L, Vaillancourt F, Pelet S, Simonyan D, Belzile EL. Prevalence and characteristics of atypical periprosthetic femoral fractures. J Bone Miner Res 2019;34:83-92. [Google Scholar | PubMed]
- 7.Turnbull GS, Soete S, Akhtar MA, Ballantyne JA. Risk factors for femoral stem fracture following total hip arthroplasty: A systematic review and meta analysis. Arch Orthop Trauma Surg 2024;144:2421-8. [Google Scholar | PubMed]
- 8.Lee JM, Park CH, Yoo JI, Kim JT, Cha Y. Atypical periprosthetic femoral fracture with stem breakage: A case report. Osteoporos Int 2022;33:2043-7. [Google Scholar | PubMed]
- 9.Ferreira P, Bates P, Daoub A, Dass D. Is bisphosphonate use a risk factor for atypical periprosthetic/peri-implant fractures? a metanalysis of retrospective cohort studies and systematic review of the current evidence. Orthop Traumatol Surg Res 2023;109:103475. [Google Scholar | PubMed]
- 10.Robinson JD, Leighton RK, Trask K, Bogdan Y, Tornetta P 3rd. Periprosthetic atypical femoral fractures in patients on long-term bisphosphonates: A multicenter retrospective review. J Orthop Trauma 2016;30:170-6. [Google Scholar | PubMed]
- 11.MacKenzie SA, Ng RT, Snowden G, Powell-Bowns MF, Duckworth AD, Scott CE. Periprosthetic atypical femoral fractures exist and are associated with duration of bisphosphonate therapy. Bone Joint J 2019;101-B:1285-91. [Google Scholar | PubMed]
- 12.Zhang CF, Yan CH, Ng FY, Chan PK, Chiu KY. Fracture of extensively porous-coated cylindrical femoral stem following revision total hip arthroplasty. Chin Med J (Engl) 2016;129:1374-6. [Google Scholar | PubMed]
- 13.Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: Issues and controversies related to their surgical management. Bone Joint J 2017;99-B:295-302 [Google Scholar | PubMed]
- 14.Toro G, Ojeda-Thies C, Calabro G, Toro G, Moretti A, Guerra GM, et al. Management of atypical femoral fracture: A scoping review and comprehensive algorithm. BMC Muscoskel Disord 2016;17:227. [Google Scholar | PubMed]
- 15.Troiano E, Giacche T, Facchini A, Orlandi NC, Cacioppo M, Saviori M, et al. Surgical and pharmacological management of periprosthetic atypical femoral fractures: A narrative literature review. Geriatr Orthop Surg Rehabil 2022;13:21514593221090392. [Google Scholar | PubMed]