Capitellum and trochlea fracture as a single entity in the coronal plane (mimicking McKee type 4 fractures) with triceps avulsion injury requires careful assessments, appropriate reduction technique, tendon repair, and tailored rehabilitation.
Sharan Mallya, Department of Orthopaedics, All India Institute of Medical Sciences, Guwahati, Assam, India. E-mail: sharanmallya@gmail.com
Introduction: Capitellum fractures are rare, representing only 1% of all elbow injuries. McKee Type 4 capitellum fractures encompass osteochondral shearing fractures of the capitellum, which involve a significant lateral portion of the trochlear ridge and the trochlea. These fractures may be linked with soft tissue and bone injuries surrounding the elbow, such as distal triceps tendon avulsion (DTTA) injuries. To date, only three case reports in the English literature have documented the correlation between Type 4 capitellum and trochlear fractures with DTTA injuries. Orthopedic surgeons should be vigilant for distal triceps and other posterior elbow injuries, which are often easily overlooked in the presence of prominent primary injuries at the front. The recommended method is prompt surgical intervention for these conditions; however, it is crucial to exercise careful judgment when deciding on the treatment and rehabilitation strategies for such cases.
Case Report: We present a distinctive case in which an entire capitellum and trochlea were fractured as a single unit in the coronal plane (mimicking McKee type 4 capitellum fractures), along with a DTTA injury in a female patient in her late 40s. This injury was treated using open reduction and internal fixation with cannulated cancellous screws, along with the repair of the DTTA injury.
Conclusion: This unique report provides a comprehensive overview of the pre-operative evaluations, reduction techniques, tendon repair, and post-operative rehabilitation process for such injuries, which showed a favorable outcome. The described fracture pattern has the potential to be categorized as type 5 fractures.
Keywords: Elbow injury, capitellum fractures, classifications, triceps tendon avulsion, rehabilitation.
Capitellum fractures constitute roughly 3–6% of all distal humerus fractures and 1% of elbow fractures, rendering this type of fracture particularly uncommon [1]. It is typical to find accompanying soft tissue and bone injuries around the elbow; thus, surgeons must proceed with caution when assessing capitellum fractures [2]. The classification system developed by Suenghwan and Morrey [1] is well-established for categorizing capitellum fractures, with the type 4 category introduced by McKee et al. [3] to describe shearing osteochondral coronal fractures of the distal humerus that extend beyond the capitellum, affecting a significant portion of the lateral trochlear ridge and trochlea. Distal triceps tendon avulsion (DTTA) injuries are also rare, accounting for <1% of all upper limb tendon injuries [4,5], and are exceedingly uncommon in conjunction with capitellum fractures. There is a lack of reports concerning the occurrence of McKee type 4 [1,3] capitellar fractures alongside DTTA injuries [6,7], including their management and rehabilitation protocols. This presentation is atypical and may be classified as a Type 5 fracture. This report also examines the existing literature on the mechanisms of injury, classifications, and treatment options for such cases, and provides rehabilitation information.
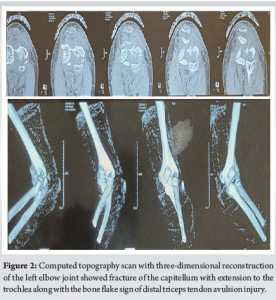
A woman in her late 40s, who is a homemaker by profession, visited the orthopedics outpatient department with complaints of pain, swelling, and an inability to move her left elbow (non-dominant limb) after experiencing an accidental fall onto an outstretched hand with the elbow joint in a semi-flexed position from a height of 2 feet. A clinical examination revealed swelling of the elbow, accompanied by significant tenderness on both the anterior and posterior sides of the elbow joint, as well as a severe limitation of motion at the elbow joint. The three-point bony relationship was preserved. There was a contusion at the tip of the olecranon in the area where the triceps muscle attaches, with no external skin breach, visible bony deformity, or neurovascular deficits. The patient reported no comorbidities or notable medical or surgical history in the past. The X-ray of the elbow joint (Fig. 1) revealed a double arc sign indicative of a capitellum fracture that extends to the trochlea, accompanied by a small bony fragment located proximal to the olecranon process, referred to as the “bone flake” sign, which suggests a DTTA fracture injury. A computed tomography (CT) scan with three-dimensional reconstructions (Fig. 2) validated the diagnosis of a variant of McKee type 4 [1,3] and Dubberley type 2A [8] capitellum fracture with extension to the trochlea, without any comminution or fragmentation, in addition to the DTTA fracture injury. This fracture pattern is distinctive because it has neither been classified nor described in existing literature. Before the surgery, written informed consent was obtained from the patient and her relatives (Figs. 1 and 2).

Surgical technique
Following the pre-operative evaluation, considering the fracture configuration and DTTA injury, it was determined that the combination of injuries would be managed through open reduction and internal fixation (ORIF) utilizing cannulated screws, along with the repair of the tendon avulsion injury. The procedure was performed under regional anesthesia with tourniquet support, positioning the patient in lateral decubitus with the left upper arm supported by a padded post, the left elbow flexed at 90°, and the forearm and hand hanging over the side of the post. A posterior midline incision was executed over the skin, centered at the distal triceps and olecranon process. A small medial-based and a large lateral-based full-thickness flap was raised to reveal the triceps, olecranon process, anconeus, radial wrist extensors, and the common extensor origin mass. The extended lateral approach was employed. The origins of the radial wrist extensors and a portion of the brachioradialis were elevated subperiosteally, and an intermuscular interval was developed distally between the extensor carpi radialis brevis and the extensor digitorum communis. The brachialis was then elevated, and a joint arthrotomy was performed along a straight line anterior to the midline of the radial head to preserve the lateral ulnar collateral ligament. The forearm was maintained in a pronated position to prevent injury to the posterior interosseous nerve. The fracture fragment of the capitellum and trochlea was carefully exposed, manipulated to achieve reduction with the elbow extended, and manually compressed using pointed bone reduction forceps while ensuring the soft-tissue attachments were preserved to reduce the risk of avascular necrosis. The elbow was then flexed, and the forearm was pronated to maintain the reduction of the fracture fragment. The reduction was verified under fluoroscopy and was found to be satisfactory. Since the trochlear portion of the fracture was also reduced at the same time, separate exposure was not considered necessary. Under fluoroscopic guidance, two guide wires were inserted into the capitellar fracture fragment from the posteroanterior direction, and one guide wire was placed into the trochlear fracture. A partially threaded cannulated cancellous screw of size 4 mm equipped with washers was utilized in compression mode to compress and reduce the fracture fragments. The alignment of the articular surface and the positioning of the screws were verified using fluoroscopy while the forearm was positioned in neutral, supination, and pronation orientations. The DTTA fracture was addressed utilizing the transosseous suture method. A non-absorbable polyester suture was employed through the triceps tendon via the modified Bunnell technique, followed by the passage of sutures through a transosseous drill hole in the olecranon, which were subsequently tied over a bone bridge (Fig. 3). The complete range of motion of the elbow, including flexion-extension and pronation-supination, was re-evaluated for ligamentous stability, mechanical obstruction, or crepitation. During the procedure, the elbow valgus and varus stress tests for collateral ligaments post-osteosynthesis and triceps repair yielded normal results. The wound was meticulously closed in layers. The stability of the elbow joint and the arc of motion in neutral, supinated, and pronated forearm positions were reassessed once more after the soft-tissue closure. An above-elbow splint was applied at a 60° flexion angle. A daily dosage of 75 mg of oral Indomethacin was prescribed for 3 weeks as a preventive measure against heterotopic bone formation. Skin sutures were removed on the 14th day following the operation (Fig. 3).

Post-operative rehabilitation
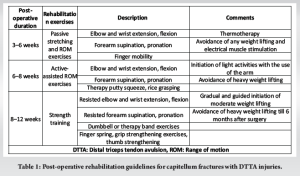
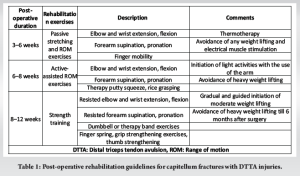
The elbow splint was maintained at a 60° flexion for 4 weeks. Following this period, passive range of motion exercises were initiated, succeeded by assisted active range of motion exercises, to restore complete elbow mobility within the subsequent 4 weeks. Upon receiving radiological confirmation of fracture healing at the 8-week mark, light strengthening exercises commenced, with a gradual increase in intensity. Heavy weight lifting was prohibited until 6 months post-surgery (Table 1).
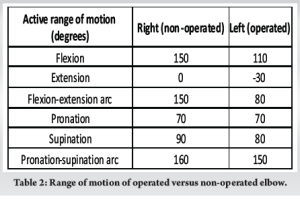
Six months after the surgery, the patient successfully regained a satisfactory range of motion in her left elbow. The comparison of the range of motion between the operated elbow and the normal elbow is illustrated in Table 2 and Fig. 4. The Mayo Elbow Performance Score recorded was 80, indicating a good outcome, while the DASH score was 17.5 at the 6-month mark. Grip strength was measured at 90% on the right side. She was able to return to her prior level of activity and could perform all her daily living activities. There was no indication of varus, valgus, or posterolateral ligamentous instability. The follow-up X-ray (Fig. 5) demonstrates a complete union of the fractures, with no signs of myositis ossificans (Figs. 4 and 5, Table 2).


Fractures of the capitellum are frequently linked with additional injuries to the elbow’s bones and soft tissues. Orthopedic surgeons must remain alert to the possibility of concurrent injuries, as these may be easily missed or disregarded in the presence of significantly apparent primary injuries. Commonly associated injuries include fractures of the radial head, collateral ligament injuries, and elbow dislocations. Less common concomitant injuries consist of Essex-Lopresti injuries, ulnar nerve injuries, and DTTA injuries [8,9]. Although DTTA injuries are uncommon, they can co-occur with capitellar fractures [4]. The mechanism of injury associated with capitellar fractures in conjunction with DTTA injuries is sequential. DTTA injuries occur due to sudden, forceful contractions of the triceps during a fall onto an outstretched hand [4,5]. Capitellum fractures result from direct axial forces transmitted by the radial head when the elbow is either extended or semi-flexed. As the force of the injury escalates, sudden, forceful eccentric contractions of the triceps, aligned with the axis of the medial collateral ligament, combined with flexion forces, may lead to DTTA injuries with a lifting motion in the posterolateral direction [1,7]. This combination of fractures can also arise from high-energy trauma, such as falls from heights or road traffic accidents, particularly in younger patients [1]. DTTA injury may be overlooked in up to 45% of patients during the initial evaluation of their injury [10]. Significant swelling and/or bruising in the posterior area of the elbow, accompanied by a noticeable gap just above the olecranon process, serve as important indicators of DTTA injury, in addition to the inability to actively extend the elbow [4,11]. DTTA fracture can be initially identified through a standard plain lateral X-ray of the elbow joint, where a “bone flake” is observed posterior to the distal humerus and proximal to the olecranon [11,12]. This finding is deemed pathognomonic [6,11]. A palpable gap located posteriorly at the elbow, just above the olecranon, together with the “bone flake” sign on the radiograph, confirms the presence of DTTA injury [4,11]. Zacharia and Roy [13] have established a classification system for traumatic distal triceps tendon injuries, categorizing these injuries clinicoradiologically into four distinct types. Type I involves a palpable soft-tissue gap without any attachment of bone fragments, and X-rays do not reveal any bony fragments; Type II features a palpable soft-tissue gap with or without bone fragment attachment, with X-rays indicating a wafer-thin or comminuted fragment; Type III presents a palpable soft-tissue gap accompanied by a bony fragment that does not reach the articular surface; and Type IV is characterized by an avulsion injury of the olecranon with <25% involvement of its articular surface. In our case, the patient was diagnosed with a Type II injury according to the classification by Zacharia and Roy [13]. A CT scan with 3D reconstructions is considered the gold standard for identifying fractures of the capitellum [1,14]. In cases of triceps tendon ruptures, while the presence of the “bone flake” sign is indicative of an avulsion fracture of the olecranon, further advanced imaging may be utilized to verify the diagnosis [11]. Magnetic resonance imaging (MRI) is regarded as the preferred method of investigation. In addition, ultrasonography can be employed to assess injuries to the triceps tendon [11,13]. In our situation, since both X-ray and CT scan validated the diagnosis of DTTA injury, we did not proceed with MRI. The treatment strategy for Type 4 capitellar fractures accompanied by related injuries must include a detailed assessment of the fracture’s specific characteristics, its complexity, and any associated bone and soft-tissue injuries [14]. Moreover, the patient’s expectations, overall health condition, existing comorbidities, functional requirements, and the necessity for weight-bearing with the upper extremities are also critical factors to consider [14]. Surgical intervention through ORIF is the preferred approach for Type 4 fractures with associated injuries. Alternative treatment options consist of: arthroscopic-assisted reduction and fixation, elbow hemiarthroplasty, total elbow arthroplasty, or non-operative management for frail, elderly patients with comorbidities or in cases of concurrent arthrosis [14]. The management approach for acute DTTA injury involves an early primary repair, ideally performed within 2–3 weeks following the trauma [5,11]. The transosseous suture technique, utilizing a transosseous drill hole, is the most prevalent and widely adopted method for repair. Additional techniques employed include the direct repair method and the suture anchors technique [5,11]. We present a case involving a middle-aged female patient who sustained a capitellum and trochlear fracture alongside a concomitant DTTA injury, a condition that is rarely documented. To date, we have identified only three reports [6-8] that specifically detail cases of simultaneous capitellum fractures associated with triceps avulsion fractures or triceps ruptures. Doleac et al. [6] utilized a dual approach in their case report: an anterolateral method for fracture fixation employing 3 mm cannulated compression screws, alongside a posterior technique utilizing a suture anchor for the repair of triceps avulsion. Kim et al. [7] documented two cases. In the first instance, they implemented an extensive lateral approach, elevating the posterior skin flap for fracture fixation with a 3.5 mm screw and an Acutrak screw, followed by triceps repair using a transosseous technique after the excision of the avulsed fragment. For the second patient, given that the time from injury to presentation was 6 weeks, they opted for the excision of the capitellum and trochlear fragment through a lateral approach. They chose not to address the triceps injury, believing it to be a partial rupture with fibrotic healing, as there were no signs of extension weakness, tenderness, or a palpable gap in the posterior elbow area. Dubberley et al. [8] did not specify the surgical approach, method of fracture fixation, or technique for triceps repair in a single patient who presented with a fracture of the capitellum and trochlea accompanied by triceps rupture. Nevertheless, none of the reports addressed post-operative rehabilitation for these patients, which is essential for optimal outcomes. There is no universal post-operative rehabilitation approach that applies to all such injuries. We believe that the rehabilitation process for these combined injuries should be customized based on various factors: injury patterns, the complexity of associated injuries, the type of surgery and fixation methods, the strength of the surgical repair, and the functional requirements of the patient; this invariably necessitates a well-defined individualized protocol, stringent supervision, and consistent follow-up. A comprehensive multimodal management strategy, coordinated among orthopedics, physical medicine and rehabilitation, and physiotherapy, can yield the best results for the patient. Consequently, in partnership with the multidisciplinary team, we developed a comprehensive post-operative rehabilitation guideline for this patient following surgery, as outlined in Table 1.
Capitellum fractures accompanied by a DTTA injury are uncommon. The avulsion of the triceps tendon may be easily missed, necessitating thorough clinical and radiological evaluations to accurately diagnose these injuries. This report presents a rare fracture pattern involving the capitellum and trochlea bones that resembles a McKee type 4 capitellar fracture, which was treated surgically with ORIF along with tendon repair. Careful pre-operative evaluations, intraoperative reduction techniques, methods for repairing the tendon avulsion, and a customized post-operative rehabilitation protocol are essential to achieve a favorable outcome in these distinctive cases.
The surgeons must recognize the simultaneous occurrence of Capitellum and trochlea fractures as a single entity in the coronal plane, accompanied by distal triceps avulsion injury. A thorough clinical evaluation, supplemented by radiological imaging, is essential in these instances, along with appropriate reduction methods and tendon repair. The customised rehabilitation protocol serves as the backbone of the management.
References
- 1.Suenghwan J, Morrey BF. Distal humerus fractures: Isolated fracture of the capitellum. In: Morrey BF, Sanchez-Sotelo J, Morrey ME, editors. Morrey’s the Elbow and its Disorders. 5th ed. Philadelphia, PA: Elsevier; 2018. p. 458-65. [Google Scholar | PubMed]
- 2.Carroll MJ, Athwal GS, King GJ, Faber KJ. Capitellar and trochlear fractures. Hand Clin 2015;31:615-30. [Google Scholar | PubMed]
- 3.McKee MD, Jupiter JB, Bamberger HB. Coronal shear fractures of the distal end of the humerus. J Bone Joint Surg Am 1996;78:49-54. [Google Scholar | PubMed]
- 4.Canbora K, Ozyurek S, Gumussuyu G, Kose O. Triceps tendon avulsion and associated injuries of the elbow. BMJ Case Rep 2013;2013:bcr2013009460. [Google Scholar | PubMed]
- 5.Alnaji O, Erdogan S, Shanmugaraj A, AlQahtani S, Prada C, Leroux T, et al. The surgical management of distal triceps tendon ruptures: A systematic review. J Shoulder Elbow Surg 2022;31:217-24. [Google Scholar | PubMed]
- 6.Doleac P, Hamza A, Deghrar A, Ohl X. Triceps avulsion associated with capitellum fracture: An unusual lesional combination in the elbow. Trauma Case Rep 2018;15:26-31. [Google Scholar | PubMed]
- 7.Kim JY, Lee JS, Kim MK. Fractures of the capitellum concomitant with avulsion fractures of the triceps tendon. J Hand Surg Am 2013;38:495-7. [Google Scholar | PubMed]
- 8.Dubberley JH, Faber KJ, Macdermid JC, Patterson SD, King GJ. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am 2006;88:46-54. [Google Scholar | PubMed]
- 9.Fram BR, Seigerman DA, Ilyas AM. Coronal shear fractures of the distal humerus: A review of diagnosis, treatment, and outcomes. Hand (N Y) 2021;16:577-85. [Google Scholar | PubMed]
- 10.Van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am 2003;85:1961-7. [Google Scholar | PubMed]
- 11.Walker CM, Noonan TJ. Distal triceps tendon injuries. Clin Sports Med 2020;39:673-85. [Google Scholar | PubMed]
- 12.Chamseddine A, Jawish RM, Zein HK. Avulsion of the distal triceps tendon with fracture of the radial head. Eur J Orthop Surg Traumatol 2011;21:607-10. [Google Scholar | PubMed]
- 13.Zacharia B, Roy A. A clinicoradiological classification and a treatment algorithm for traumatic triceps tendon avulsion in adults. Chin J Traumatol 2021;24:266-72. [Google Scholar | PubMed]
- 14.Chen N, Ring D. Distal humerus fractures: Shear Fractures of the Humeral Articular Surface. In: Morrey BF, Sanchez-Sotelo J, Morrey ME, editors. Morrey’s the Elbow and its Disorders. 5th ed. Philadelphia, PA: Elsevier; 2018. p. 458-65. [Google Scholar | PubMed]