The Role of Teriparatide aided in improving early callus formation and better stability at the fracture site which lead to early mobilisation and better functional outcome.
Dr. P Pradeep, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India. E-mail: jppradeep.dr@gmail.com
Introduction: Teriparatide (TPTD), a recombinant form of the biologically active Parathyroid hormone, has been shown to increase bone mass and prevent fractures by increasing serum calcium levels in response to systemic hypocalcemia. Studies have shown improvements in callus volume and mineralization, bone mineral content, rate of successful union, and strength at fracture sites, and produce a sustained anabolic effect throughout the remodeling phase of fracture healing. The present study was done to evaluate the efficacy of TPTD in hastening fracture healing in elderly patients by clinical, radiological, and biochemical parameters.
Materials and Methods: A prospective case–control study was done on elderly patients (>55 years) with fractures. Pre-operative bone mineral profile assessed. All fractures were surgically fixed. All patients postoperatively on day 5 were started on injection TPTD 20 mcg daily for 8 weeks. Immediate post-operative radiographs and at 4 weeks, 8 weeks (after completion of TPTD), and 16 weeks were taken to assess the radiological Callus Index score. After completion of 8 weeks, a bone mineral profile was done to assess any biochemical changes in response to TPTD usage. Functional assessment was done with a Visual Analog Scale score and a two-minute walk test. All the results were compared with the non-TPTD group.
Results: The use of TPTD showed improvement in bone mineral content and better functional and radiological outcomes compared to the control group.
Conclusion: Both TPTD and Non-TPTD group patients showed fracture healing, but the duration of healing was significantly shorter in the TPTD group. Functional assessment showed better pain control and an increase in the two-minute walk test distances in the TPTD group.
Keywords: Teriparatide, Fracture healing, Early mobilisation, Parathyroid hormone analog, Osteoporosis.
Globally, the incidence of hip fractures among the elderly is estimated to rise from 1.66 million in 1990 to 6.26 million by 2050, there could be [1]. In the older population, fractures at this site frequently contribute to increased mortality and unfavorable outcomes, with 1 1-year mortality rate estimated to be around 30% [2]. Most fracture patients endure limited mobility and difficulty doing daily tasks during their rehabilitation, and the resumption of activities to the pre-fracture functional level even after a year is questionable [3]. The purpose of treatment, regardless of the protocol, is to ease pain, facilitate mobilization, and minimize problems related to pathologies after a fracture. Patients should be followed up after undergoing primary care to monitor fracture healing. Slow healing after a hip fracture is generally connected with unfavorable outcomes [4]. Therefore, there is an imminent need to promote hip fracture healing and functional recovery by swiftly restoring hip function without jeopardizing functional outcomes. While the efficacy of several systemic medicines for functional recovery is debatable, locally applied pharmacologic therapy to speed bone healing has received permission in some nations [5]. One such adjuvant in fracture healing that has been explored in recent times is the novel biologic-Teriparatide (TPTD). TPTD’s contribution to the healing of hip fractures has been investigated by several surgeons [6]. Although TPTD did not reduce the incidence of revision surgery or complications, according to studies, it did improve radiographic signals of fracture healing and early clinical outcomes in hip fractures [7]. Yet the outcomes were inconclusive. As a result, the effect of TPTD on fracture healing is unknown. More research in orthopedic surgery is required to show the effects of TPTD therapy in patients with hip fractures.
Objectives
The present study was carried out to evaluate the efficacy of injection (INJ) TPTD in hastening fracture healing in elderly patients, assessed by clinical, radiological, and biochemical parameters.
The present study was carried out as a prospective case–control study among participants who sustained low-velocity hip proximal femur trochanteric fractures.
Inclusion criteria
- Age above 55 years
- Intertrochanteric/subtrochanteric/peritrochanteric fractures
- Treatment for hip fractures should be surgical fixation of the fracture.
Exclusion criteria
- Age <55 years
- Drug allergy to TPTD
- Conservatively managed fractures
- Patients already on TPTD INJ as a part of any therapy
- Deranged liver and renal enzymes or suspected malignancy
- Pathological fractures and other fragility fractures
- Metabolic disorders include hypercalcemia, Paget’s disease, and hyperparathyroidism.
Sample size
A total of 50 patients participated in the study, with 25 each in the case and control groups, respectively. Each participant was randomly assigned to cases or controls using a table of random numbers.
Ethical approval and consent
Approval was obtained from the Institutional Ethics Committee before the commencement of the study. Informed consent was obtained from all the participants before data collection.
Clinical management
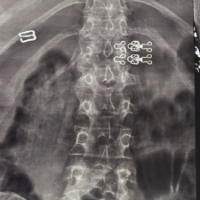
All fractures were surgically fixed by closed reduction and internal fixation with a third-generation proximal femur nail. For the participants in the case group, the patients were started on TPTD 20 mcg subcutaneous INJs daily from the 5th post-operative day, for 8 weeks. All the study participants were started on calcium and Vitamin D supplementation postoperatively.
Data collection
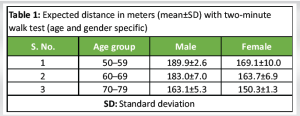
A structured interview schedule was used to collect the demographic data regarding age, gender, and other comorbidities. Pre-operative bone mineral profile, including serum calcium, serum creatinine, serum alkaline phosphatase (ALP), serum Vitamin D total (D2 and D3), serum albumin, serum magnesium, serum parathyroid hormone (PTH) (intact), was assessed for all patients, and the same was repeated at the end of the 8th week. Serial radiographic assessments were carried out at various intervals (immediate post-operative, 1st, 2nd, and 4th month after surgery. The parameters assessed include the Callus Index and disappearance of the fracture line. Observation of the Callus Index and radiographic analysis was performed by three orthopedic surgeons with more than 10 years of experience in orthopedic trauma. Visual Analog Score was carried out at the 2nd and 4th months after surgery to evaluate the pain intensity [8]. The pain score was categorized as 0 (no pain), 1–3 (mild pain), 4–6 (moderate pain), 7–9 (severe pain), and 10 (worst pain possible). Functional assessment was done using the two-minute walk test at the 2nd and 4th months after surgery [9]. The distance walked is assessed using a measuring wheel. Rest breaks were allowed if required by the participant. The average distance based on age, with mean and standard deviation, is given in Table 1.
Data analysis
Data were entered and analyzed using the Statistical Package for the Social Sciences, ver.20 software. Descriptive data were presented as mean with standard deviation. Analytical data between cases and controls was presented using an independent samples “t” test. Analytical data within cases and controls were presented using a paired “t” test. P < 0.05 was considered statistically significant.
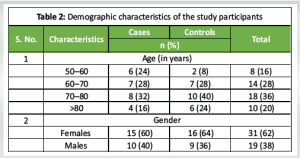
The present study was carried out among 25 participants in the TPTD group and 25 participants in the non-TPTD group. The majority of the cases and controls belonged to the age group of 70–80 years (32% and 40%, respectively). In both groups, the majority of the participants were females (60% in cases and 64% in controls) (Table 2).
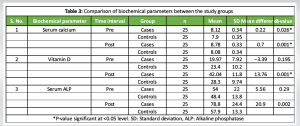
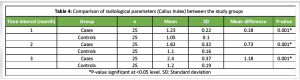
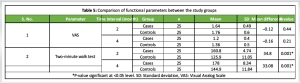
Comparison of biochemical, radiological, and functional parameters between the study groups
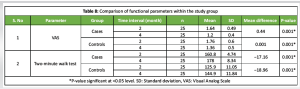
The comparison of biochemical parameters between the study groups is given in Table 3. There was a statistically significant difference in the serum calcium levels between the cases and controls before the surgery (P < 0.05) and post-surgery (P < 0.01). However, a statistically significant difference between the cases and controls was found only post-surgery with respect to Vitamin D levels (P < 0.001) and serum ALP levels (P < 0.001). On comparing the Callus Index between cases and controls, there was a significant difference in the mean Callus Index (P < 0.001) individually at 1st, 2nd, and 4th months (Table 4). Regarding the functional parameters, the mean Visual Analog Scale (VAS) scores were similar between the cases and controls at the 2nd month and at the 4th month. However, the distances covered by the two-minute walk test showed statistically significant differences (P < 0.001) between the cases and controls at the 2nd month (160.8 m and 125.9 m, respectively) and the 4th month (178 m and 144.9 m, respectively (Table 5).
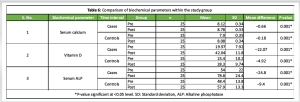
Comparison of biochemical, radiological, and functional parameters within the study groups
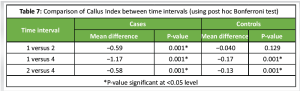
On comparing the biochemical parameters within the study group, there was a statistically significant difference in the mean values of serum calcium, Vitamin D levels, and serum ALP levels between pre- and post-surgery for both cases and controls (P < 0.001) (Table 6). On comparing the Callus Index between the cases and controls over the period, among the cases, a statistically significant difference was observed in the Callus Index between the 1st and 2nd months, 2nd and 4th months, and 1st and 4th months (P < 0.001). However, among the controls, a statistically significant difference was observed in the Callus Index only between the 1st and 4th months, and the 2nd and 4th months (P < 0.001) (Table 7). On comparing the functional parameters within the study groups, the mean difference in the VAS and two-minute walk test scores was statistically significant between the 2nd and 4th months for both the cases and controls (P < 0.001) (Table 8).
The care of hip fractures has emerged as a significant health concern due to an ageing worldwide population. To minimize surgery complications and improve patient outcomes, post-operative patient management must be optimized. Recently, there has been an increase in interest in the effects of osteoanabolic medications (TPTD) on the speed of fracture healing. In contrast to antiresorptive drugs, direct stimulation of bone creation may not only increase bone strength but also hasten the healing of fractures. In studies on animals, TPTD showed promise for enhancing bone implant contact, fracture healing efficiency, and fracture callus mechanical properties. TPTD has been shown in case studies and clinical trials to support rapid fracture healing [10]. The present study included elderly patients (>55 years) who sustained proximal femur fractures. The septuagenarian population was more prone to proximal femur fractures according to the present study, with 32% in the TPTD group and 40% in the non-TPTD group in this age group. Furthermore, females were more prone to sustaining proximal femur fractures, with around 60% in the TPTD group and 64% in the non-TPTD group. This may be due to the increased risk of osteoporosis in this group of postmenopausal senile patients. Similar findings were present in the study done by Huang et al. [11], with advancing age comes an increased chance of falling, and because elderly patients are frequently frail and have poor bone quality, their likelihood of suffering a hip fracture even after a low-energy fall is also raised.
Biochemical effects
The present study showed a significant increase in serum calcium level between the TPTD and non-TPTD groups over a 2-month span. Both groups showed a significant rise in calcium at 2-month follow-up, but the mean increase in calcium was better with the TPTD group. This was mainly due to the effect of TPTD on calcium homeostasis and increased renal reabsorption. Calcium also had a direct correlation with serum albumin level . At physiological pH, about 45% of albumin is bound to calcium. Hence, in elderly patients, a higher prevalence of hypoalbuminemia may predispose to hypocalcemia. With regards to Vitamin D levels, the TPTD group showed an increase of 22.07, and the non-TPTD group showed an increase of only 4.92. This increase was statistically significant (P = −0.001) and showed the effect of TPTD to increase serum total Vitamin D levels. Serum ALP is a marker of bone turnover. The TPTD group showed a drastic increase in serum ALP levels, but they were within the normal range. There was no abnormal increase in ALP levels, warranting any suspicion of malignancy. According to studies, gains in bone mass as measured by bone matrix outpace those in mineralization. The removal of older bone with relatively high mineralization after TPTD treatment and the formation of new bone with relatively low mineralization are likely the causes of this substantially bigger increase in bone matrix compared to mineralization. The rise in freshly generated, lower mineral density bone matrix was caused by the PTH’s stimulation of skeletal remodeling [12,13].
Radiological effects
Callus Index showed a significant appearance in the TPTD group. Callus formation was found at a very early stage in the treatment. TPTD substantially increased the unusually abundant callus formation around the fracture site at 4 weeks. Moreover, this callus formation continued for 16 weeks and led to the healing of the fracture. Abundant callus formation was found circumferentially around the cortex with a “cloud-like” appearance. Remodeling of the TPTD-induced callus formation was found to be part of the normal fracture healing process. Comparing the two groups, the TPTD group showed early callus formation, which was evident in the comparison between 1st-month and 2nd-month radiographs. In a 2-month span, the TPTD group showed a mean Callus Index at every follow-up that was better with the TPTD group than the non-TPTD group. Kim et al. showed that the mean time to radiographically defined union was 14.8 weeks (standard deviation [SD] 7.1) and 12.1 weeks (SD 6.4) in non-TPTD and TPTD groups, respectively (P = 0.002) [14]. Huang et al. studied the overall varus collapse in non-TPTD versus TPTD versus bisphosphonate group and reported that with regard to radiographic analyses, there were significant differences in overall varus collapse (5° ± 2° vs. 2° ± 1° vs. 2° ± 1 ±, P < 0.0001 [11].
Functional effects
Visual analog scores analyzed between both groups showed similar results, with a decrease in pain in both groups at the end of 2 months. There was complete resolution of pain at the end of 4 months. Kim et al. reported that VAS (pain) was significantly better in PTH-treated groups at 6 months after surgery (P = 0.008) [14]. Huang et al. reported that the mean duration of analgesic use after surgery in the non-TPTD, TPTD group, and bisphosphonate group was 24.3, 15.1, and 16.1 weeks, respectively (P < 0.001) [11]. A two-minute walk test was assessed at 2-month and 4-month follow-up in both TPTD and non-TPTD groups. A two-minute walk test at 2-month follow-up was significantly better with the TPTD group compared to the non-TPTD group. This was very much helpful for the early mobilization of the patient and better outcomes. Early mobilization following hip fracture repair is thought to be an imperative part of post-operative management. Bed rest has been associated with undesirable cardiovascular, pulmonary, and urinary effects, reduced muscle tone, loss of bone mineral density, and negative psychological effects. Specifically, early mobilization has been associated with a reduction in post-operative complications such as thromboembolism, pneumonia, wound breakdown, pressure ulcers, and delirium [15]. There were no complications in the TPTD group. However, in the non-TPTD group, two patients had helical blade back out at 1 month and 6 weeks, respectively, but both fractures went on to heal at 12 weeks. One patient had a screw cut out at 6 months, and one patient had a symptomatic versus collapse of the fracture at 1 month, who needed a reoperation in the form of bipolar hemiarthroplasty of the hip. Kim et al. reported that a total of 17 complications (28%) were encountered in the non-TPTD group and six complications (11%) in the TPTD group [14]. Huang et al. studied the overall versus collapse in non-TPTD versus TPTD versus bisphosphonate groups and reported that with regard to radiographic analyses, there were significant differences in overall versus collapse (P < 0.001) [11].
Both TPTD and non-TPTD group patients showed signs of healing, but the duration of healing was shorter for the TPTD group patients. Functional assessments showed better pain scores and increased distances in the two-minute walk test, which proves the effectiveness of TPTD in early mobilization and post-operative rehabilitation. Serum calcium and Vitamin D levels showed a significant increase in both groups, with the mean values higher in the TPTD group, indicating the role of TPTD in restoring homeostasis and bone health. A better and earlier Callus Index at serial follow-up was observed in the TPTD group, which helped in improving the stability at the fracture site and led to early mobilization and better functional outcome. Complications were not observed in the TPTD group compared to the non-TPTD group, which had 4 complications (16%). This suggests that TPTD can be used as an ideal augmentation and is effective in promoting fracture healing along with regular Osseos supplements. A further in-depth study may prove the TPTD’s isolated role in enhancing fracture healing.
Teriparatide may shorten healing time, reduce pain, and improve functional recovery, making it a valuable adjunct in complex or slow healing fractures.
References
- 1. Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop 2011;45:15-22. [Google Scholar] [PubMed]
- 2. George J, Sharma V, Farooque K, Mittal S, Trikha V, Malhotra R. Injury mechanisms of hip fractures in India. Hip Pelvis 2021;33:62-70. [Google Scholar] [PubMed]
- 3. Cohn MR, Cong GT, Nwachukwu BU, Patt ML, Desai P, Zambrana L, et al. Factors associated with early functional outcome after hip fracture surgery. Geriatr Orthop Surg Rehabil 2016;7:3-8. [Google Scholar] [PubMed]
- 4. Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: Effects on function and mortality. Arch Intern Med 2006;166:766-71. [Google Scholar] [PubMed]
- 5. Rothe R, Hauser S, Neuber C, Laube M, Schulze S, Rammelt S, et al. Adjuvant drug-assisted bone healing: Advances and challenges in drug delivery approaches. Pharmaceutics 2020;12:428. [Google Scholar] [PubMed]
- 6. Kim K, Won YY, Lee SW, Seo KD. The effect of teriparatide on the hip: A literature review. Hip Pelvis 2021;33:45-52. [Google Scholar] [PubMed]
- 7. Díez-Pérez A, Marin F, Eriksen EF, Kendler DL, Krege JH, Delgado-Rodríguez M. Effects of teriparatide on hip and upper limb fractures in patients with osteoporosis: A systematic review and meta-analysis. Bone 2019;120:1-8. [Google Scholar] [PubMed]
- 8. Brokelman RB, Haverkamp D, Van Loon C, Hol A, Van Kampen A, Veth R. The validation of the visual analogue scale for patient satisfaction after total hip arthroplasty. Eur Orthop Traumatol 2012;3:101-5. [Google Scholar] [PubMed]
- 9. Bohannon RW. Normative reference values for the two-minute walk test derived by meta-analysis. J Phys Ther Sci 2017;29:2224-7. [Google Scholar] [PubMed]
- 10. Babu S, Sandiford NA, Vrahas M. Use of teriparatide to improve fracture healing: What is the evidence? World J Orthop 2015;6:457-61. [Google Scholar] [PubMed]
- 11. Huang TW, Chuang PY, Lin SJ, Lee CY, Huang KC, Shih HN, et al. Teriparatide improves fracture healing and early functional recovery in treatment of osteoporotic intertrochanteric fractures. Medicine (Baltimore) 2016;95:e3626. [Google Scholar] [PubMed]
- 12. Paschalis EP, Krege JH, Gamsjaeger S, Eriksen EF, Burr DB, Disch DP, et al. Teriparatide treatment increases mineral content and volume in cortical and trabecular bone of iliac crest: A comparison of infrared imaging with X-Ray-based bone assessment techniques. J Bone Miner Res 2018;33:2230-5. [Google Scholar] [PubMed]
- 13. Guelman R, Sánchez A, Varsavsky M, Brun LR, García ML, Sarli M, et al. Effect of teriparatide on bone mineral density and bone markers in real-life: Argentine experience. Int J Endocrinol 2023;2023:9355672. [Google Scholar] [PubMed]
- 14. Kim SJ, Park HS, Lee DW, Lee JW. Short-term daily teriparatide improve postoperative functional outcome and fracture healing in unstable intertrochanteric fractures. Injury 2019;50:1364-70. [Google Scholar] [PubMed]
- 15. Kenyon-Smith T, Nguyen E, Oberai T, Jarsma R. Early mobilization post-hip fracture surgery. Geriatr Orthop Surg Rehabil 2019;10:2151459319826431 . [Google Scholar] [PubMed]