Preserving stump length, avoiding prosthesis socket revision, and the chance of returning to the previous activity level should be achievable treatment goals while treating fractures in lower limb amputees. Load-sharing cephalomedullary nail fixation with full-length internal splinting and a minimally invasive surgical approach is preferred to reduce complications.
Dr. Aakarsh Aggarwal, Department of Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: aakarshaggarwal1@gmail.com
Introduction: Intertrochanteric (IT) fractures are rarely reported in amputation stumps.
Case Report: This report presents the case of an elderly male with a right above-knee amputation who sustained an ipsilateral IT fracture. He had undergone amputation 3 years prior and was mobilizing independently with a prosthetic limb. The current injury occurred due to the rollover of a four-wheeler in which he was traveling. A proximally sized femoral nail was selected for fracture fixation, with the goal of internal splinting across the entire residual femoral length. Postoperatively, the patient resumed use of his previous prosthesis without difficulty.
Conclusion: Treatment goals in such cases should include preservation of stump length, avoidance of prosthesis socket revision, prevention of peri-implant fractures and implant failure, and the use of load-sharing implants in the lower extremity stump. In addition, enabling the patient to return to their prior level of activity should be a key therapeutic objective.
Keywords: Intertrochanteric femur fracture, lower limb amputees, surgical technique, intraoperative planning, implant selection
In the geriatric population, intertrochanteric (IT) fractures are among the most common injuries and represent a significant cause of morbidity and mortality. However, they are rarely encountered in amputation stumps. The combination of advanced age and disuse atrophy of the stump’s bone and musculature increases the risk of fracture, making even trivial trauma sufficient to cause a stump fracture.
The management of residual limb fractures presents unique challenges for surgeons. Altered hip biomechanics in amputees, atypical stump length, osteoporosis from disuse, associated geriatric comorbidities, and occasional phantom limb pain all complicate the clinical picture. Additional difficulties include diagnosis, immobilisation of the residual limb, intraoperative positioning, fracture reduction, choice of fixation method, and post-operative rehabilitation. Nevertheless, advances in lower limb prosthetics have enabled many amputees to remain functionally active. In the modern era, internal fixation is the mainstay of treatment for such fractures, regardless of patient age or activity level, to preserve quality of life. We present the case of a comminuted IT fracture extending into the subtrochanteric region in a high-transfemoral amputee with minimal stump length and associated abdominal and thoracic visceral injuries. After stabilization of the abdominothoracic trauma, the patient underwent closed reduction and internal fixation using a proximal femoral nail (PFN). This report outlines the pre-operative planning, intraoperative technique, and follow-up outcomes.
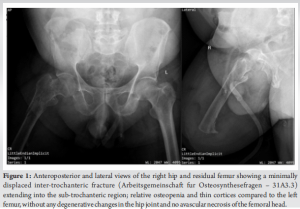
A sexagenarian male with a right-sided above-knee amputation, performed 3 years earlier following a road traffic accident, had been mobilizing independently using an above-knee prosthesis. He sustained another road traffic injury due to the rollover of a four-wheeler vehicle, resulting in trauma to the torso and the amputation stump. He presented to the emergency department with chest and abdominal pain, along with an inability to move his residual right limb. Primary advanced trauma life support protocols were initiated, and the patient was hemodynamically stabilized. He had no known medical comorbidities. Clinical examination revealed swelling and bruising around the right hip and trunk, with no external open injury near the amputation stump. The hip injury was consistent with a dashboard-type mechanism. The amputation scar was well-healed by secondary intention. Contrast-enhanced computed tomography of the abdomen and thorax revealed multiple right-sided rib fractures, a right-sided hemothorax, and a grade II liver injury. Radiographs of the pelvis and residual limb demonstrated an IT fracture extending into the subtrochanteric region (Arbeitsgemeinschaft fur Osteosynthesefragen – 31A3.3), with comminution and osteoporotic bone quality (Fig. 1).
Management
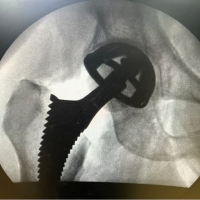
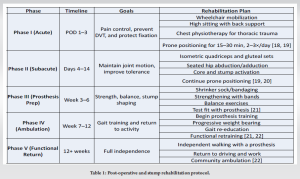
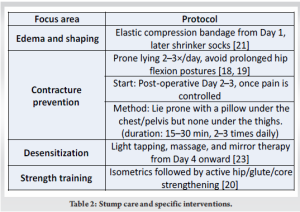
The hemothorax was managed by intercostal chest tube insertion, while the liver injury was treated conservatively under close observation. Due to the chest trauma, the patient was maintained on high-flow oxygen support during his hospital stay. After optimizing the thoracoabdominal condition, surgical fixation using an intramedullary implant was considered the most appropriate approach for managing the IT fracture, given the patient’s age, functional demands, and the elevated risk of stump infection. Following the induction of anesthesia, the patient was transferred to a traction table. A groin post was positioned, and the contralateral limb was placed on the standard lower limb attachment to facilitate intraoperative fluoroscopic imaging. Although the residual limb was short, it was sufficient to be stabilised on the ipsilateral extension of the perineal post. The patient was positioned similarly to the standard setup for antegrade femoral nailing on a traction table to facilitate nail entry, as his residual limb was in a flexed and abducted posture. Adequate reduction and alignment were achieved through manual traction and rotational maneuvers using a 4.5-mm Schanz screw under C-arm guidance, without opening the fracture site. The distance from the tip of the greater trochanter to the distal end of the stump (20 cm) had been preoperatively measured. After confirming this length intraoperatively under image intensification, an appropriately sized PFN (PFN-A, 12 × 200 mm, 130°, Titanium, DePuy Synthes) was selected. A 95-mm helical blade was used as the femoral neck element. Post-operative radiographs confirmed satisfactory fracture fixation (Fig. 2). From the 1st post-operative day, the patient was mobilized in a wheelchair. By the 4th week of follow-up, the stump had matured sufficiently to allow fitting of the previously used prosthesis. The post-operative rehabilitation protocol was followed as mentioned in Tables 1 and 2. At 12 weeks postoperatively, the patient was ambulating without support or pain. By the end of the 3rd month, he resumed using the same prosthetic limb without difficulty and returned to his pre-operative activity level. He was able to resume driving within a short period. His Harris hip score improved from 34 at 1 month, to 49.6 at 3 months, and 75.8 at 6 months follow-up. At the most recent follow-up, there were no signs of soft-tissue infection or wound dehiscence.

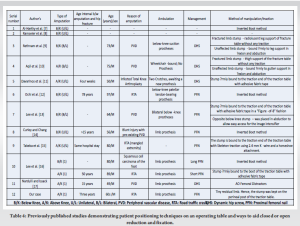
Isolated femoral fractures and their management in above-knee amputees have been described in the literature. While the ideal approach to these injuries was once debated, recent evidence supports internal fixation over conservative management. Earlier studies questioned the utility of surgical intervention or internal fixation in amputation stumps covered by a prosthesis, suggesting that neither surgical scars nor implanted hardware would be well tolerated in such patients [1]. In 1981, Lewallen and Johnson reported that four out of nine patients treated with internal fixation experienced complications. They recommended implant removal after fracture healing in cases where the prosthesis socket could not be accommodated over the stump, and advised conservative treatment whenever feasible, citing the relatively rapid union of fractures in amputation stumps even without fixation [2]. However, more recent studies suggest that fractures in residual limbs behave similarly to those in non-amputated limbs [3]. Although osteoporosis is commonly observed in residual bones following amputation, it does not appear to adversely affect fracture healing. Well-performed surgical dissection and closure in the amputation stump do not generally result in problematic scarring. In addition, advances in prosthetic design – especially the use of easily moldable plastics – and modern fixation techniques have greatly reduced post-operative complications associated with internal fixation [4]. Following a comprehensive review of the literature, closed reduction and internal fixation were selected for this case. The potential advantages included: (1) Early fracture healing and early mobilization, (2) an increased likelihood of returning to the pre-injury level of activity, and (3) reduced risk of complications such as decubitus ulcers, deep vein thrombosis, and pulmonary issues often associated with prolonged immobility. A key consideration in the fixation of fractures in amputation stumps is the selection of the appropriate implant. Load-sharing cephalomedullary nail fixation – such as the PFN – is most suitable for lower extremity fractures. These implants require less soft-tissue dissection than load-bearing surface implants (e.g., plates). Another crucial principle is internal splinting of the entire length of the residual femur. This reduces the risk of future peri-implant or serial fractures and avoids implant protrusion beyond the distal end of the stump [5].
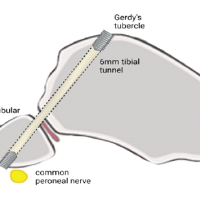
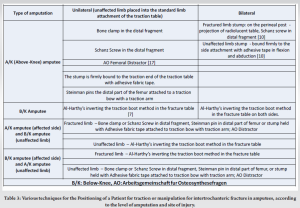
The femoral stump length can be measured preoperatively on radiographs to determine the appropriate type and dimensions of the implant. In our case, the distance from the tip of the greater trochanter to the distal end of the stump was 20 cm, making the 200 mm PFN-A the most suitable implant. A helical blade was used as the femoral neck element, given the pre-existing poor bone quality and the patient’s advanced age. The spiral blade provides superior resistance to cut-out compared to a lag screw in trochanteric fixation [6]. Considering these factors reduces the risk of peri-implant fracture and implant failure, minimizes the need for future prosthesis socket revision, and decreases the likelihood of wound-related complications. Patient positioning presents another technical challenge in the surgical management of these cases. For below-knee amputation stumps, traction can be applied using Al-Harthy’s et al. inverted boot method [7]. However, few studies have detailed positioning techniques on the operating table to assist in closed or open reduction and fixation [8,9,10,11,17] (Supplementary Table 3,4).
Above-knee amputees present unique difficulties, as the stump length is a key factor in achieving stable positioning, effective counter-traction of the contralateral limb, and optimal fluoroscopic imaging during surgery. In bilateral above-knee amputees, the stump on the fractured side can be supported on the thigh rest of the fracture table without a traction component, whereas the unaffected stump can be securely attached to the thigh gutter support in abduction and flexion (Table 3). In unilateral above-knee amputees, the unaffected limb stump can be secured to the standard limb attachment of the traction table. The injured limb may be positioned on the perineal post-projection or the standard extension of the radiolucent table. It can be manipulated using a bone clamp or Schanz screw in the distal fragment, a Steinmann pin in the distal femur, or by securing the stump with adhesive fabric tape connected to a traction bow and traction arm [11]. In our case, where the above-knee amputation was on the same side as the fracture, the unaffected limb was attached to the traction unit to provide counter-traction and facilitate fluoroscopy. The injured residual limb, due to its limited length (20 cm), was simply positioned on the perineal post-projection of the traction Tables 1, 2, and 4. The most critical goal in treating hip fractures in amputees – whether above- or below-knee – is restoring the normal neck-shaft angle of the femur, as this directly supports optimal hip abductor function [4]. Selecting the appropriate fixation method is essential for helping amputees return to their pre-fracture status, which includes effective and comfortable use of a prosthetic limb. Another important consideration is preserving stump length, which significantly influences the physiological cost index and walking speed in transfemoral amputees [4].
Careful planning is essential for managing stump fractures. A thorough discussion of the various treatment options is necessary, and realistic treatment goals should be established after considering the level of amputation, the biomechanical properties of available implants, and the presence of osteopenia in the residual bone. These patients can be effectively managed with osteosynthesis cephalomedullary fixation using a standard operating table or a traction table, requiring only minor modifications in positioning and table attachments – without the need for a specialised operating theatre setup.
When treating fractures in lower limb amputees, therapeutic objectives should include preserving stump length, avoiding prosthesis socket revision, and facilitating a return to the patient’s prior level of activity. For lower extremity stumps, load-sharing cephalomedullary nail fixation is the preferred option. Due to disuse atrophy of the residual limb, the fixation strategy should aim to internally splint the entire length of the fractured bone to reduce the risk of peri-implant fracture. Therefore, the type and size of the implant must be carefully selected to avoid impingement on the stump. A minimally invasive surgical technique is always preferable to minimize soft-tissue disruption.
References
- 1. Slocum DB. An Atlas of Amputations. St Louis: CV Mosby; 1949. [Google Scholar] [PubMed]
- 2. Lewallen RP, Johnson EW Jr. Fractures in amputation stumps: Review of treatment of 16 fractures. Mayo Clin Proc 1981;56:22-6. [Google Scholar] [PubMed]
- 3. Freese P. Frakturen an amputationsstümpfen und amputierten gliedemassen [Fractures of amputation stumps and amputated limbs]. Monatsschr Unfallheilkd 1965;68:433-9. [Google Scholar] [PubMed]
- 4. Bowker JH, Rills BM, Ledbetter CA, Hunter GA, Holliday P. Fractures in lower limbs with prior amputation. A study of ninety cases. J Bone Joint Surg 1981;63:915-20. [Google Scholar] [PubMed]
- 5. Nannaparaju M, Annavaram K, Anwar R, Khan WS, Hambidge J. Serial femoral fractures in an amputation stump: A case report. Open Orthop J 2017;11:316-20. [Google Scholar] [PubMed]
- 6. Kantiwal P, Gupta S, Yadav SK, Elhence A. Letter to the editor with reference to “Gin Way Law, Yoke Rung Wong, Antony Gardner and Yau Hong NG. Intramedullary nailing confers an increased risk of medial migration compared to dynamic hip screw fixation in unstable intertrochanteric hip fractures.” Injury 2021;52:3540. [Google Scholar] [PubMed]
- 7. Al-Harthy A, Abed R, Campbell AC. Manipulation of hip fracture in the below-knee amputee. Injury 1997;28:570. [Google Scholar] [PubMed]
- 8. Ramseier LE, Werner CM, Hug T, Preiss S. Suprakondyläre extension einer pertrochantären femurfraktur bei einem patienten mit unterschenkelamputation [Supracondylar traction of a pertrochanteric femur fracture in a patient amputated below the knee]. Unfallchirurg 2005;108:239-40. [Google Scholar] [PubMed]
- 9. Rethnam U, Yesupalan RS, Shoaib A, Ratnam TK. Hip fracture fixation in a patient with below-knee amputation presents a surgical dilemma: A case report. J Med Case Rep 2008;2:296. [Google Scholar] [PubMed]
- 10. Aqil A, Desai A, Dramis A, Hossain S. A simple technique to position patients with bilateral above-knee amputations for operative fixation of intertrochanteric fractures of the femur: A case report. J Med Case Rep 2010;4:390. [Google Scholar] [PubMed]
- 11. Davarinos N, Ellanti P, McCoy G. A simple technique for the positioning of a patient with an above knee amputation for an ipsilateral extracapsular hip fracture fixation. Case Rep Orthop 2013;2013:875656. [Google Scholar] [PubMed]
- 12. Ochi H, Baba T, Hamanaka T, Ozaki Y, Watari T, Homma Y, et al. Safe and effective reduction technique for intertrochanteric fracture with ipsilateral below-knee amputated limb. Case Rep Orthop 2017;2017:2672905. [Google Scholar] [PubMed]
- 13. Lee BH, Ho SW, Kau CY. Surgical fixation of a comminuted inter-trochanteric fracture in a patient with bilateral below knee amputation. Malays Orthop J 2018;12:54-6. [Google Scholar] [PubMed]
- 14. Curley AJ, Chang ES. Operative positioning technique for an intertrochanteric fracture in a patient with an ipsilateral below-the-knee amputation: A case report. JBJS Case Connect 2019;9:e1. [Google Scholar] [PubMed]
- 15. Takeba J, Imai H, Kikuchi S, Matsumoto H, Moriyama N, Nakabayashi Y. A simple method for positioning the traction table during fixation surgery for a displaced femoral trochanteric fracture in a patient following ipsilateral above-the-knee amputation: A case report. J Orthop Case Rep 2020;10:76-9. [Google Scholar] [PubMed]
- 16. Lee SM, Suh KT, Oh YK, Shin WC. Manipulation of intertrochanteric fractures in patients with below- or above-knee amputation using a fracture table: Two case reports. Medicine (Baltimore) 2021;100:e24233. [Google Scholar] [PubMed]
- 17. Nardulli CM, Issack PS. ORIF of an intertrochanteric fracture proximal to an above-knee amputation using two AO femoral distractors. Trauma Case Rep 2023;44:100806. [Google Scholar] [PubMed]
- 18. Smith DG, Horn P, Ehde D, Czerniecki JM, Malchow D, Hansen ST. Postoperative positioning to prevent hip flexion contracture in transfemoral amputees. Arch Phys Med Rehabil 1999;80:521-5. [Google Scholar] [PubMed]
- 19. Pasquina PF, Carvalho AJ, Sheehan TP. Ethics in rehabilitation: Allocation of resources and long-term care. J Am Acad Orthop Surg 2015;23:519-22. [Google Scholar] [PubMed]
- 20. Esquenazi A, Meier RH 3rd. Rehabilitation in Limb Deficiency. 4th ed. Rosemont, IL: American Academy of Physical Medicine and Rehabilitation; 2014. p. 105-26. [Google Scholar] [PubMed]
- 21. Krajbich JI, Pinzur MS, Potter BK, Stevens PM. Atlas of amputations and limb deficiencies. In: Surgical, Prosthetic, and Rehabilitation Principles. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2016. [Google Scholar] [PubMed]
- 22. Dudkiewicz I, Gabrielov R, Seiv-Ner I, Zelig G, Heim M. Evaluation of prosthetic usage in upper limb amputees. Disabil Rehabil 2004;26:60-3. [Google Scholar] [PubMed]
- 23. Ramstrand N, Hermodsson Y. Evaluation of walking ability in individuals with unilateral transfemoral amputation: A comparison of different prosthetic knee joints. Prosthet Orthot Int 2005;29:135-45. [Google Scholar] [PubMed]