Inverted or femoral-sided cyclops lesions are a rare but plausible diagnosis in patients presenting with a clunk with loss of terminal extension after ACL repair, even in the absence of MRI evidence. Prompt recognition and intervention are crucial, where removal of the lesion and notchplasty can lead to full recovery of the range of motion.
Dr. James Pate, Department of Orthopedic Surgery, University of Tennessee at Chattanooga, 979 East Third Street, Suite 202 Chattanooga - 37403, Tennessee, United States. E-mail: jpate0104@gmail.com
Introduction: Cyclops lesions are a well-described complication following reconstruction of the anterior cruciate ligament (ACL). These lesions are fibrous nodules that most commonly form anterolateral to the tibial tunnel and impede terminal knee extension. Inverted or femoral-sided cyclops lesions are a rare variant that have been described after ACL reconstruction, but not after repair. This is the first case in the literature to demonstrate an inverted cyclops lesion following ACL repair.
Case Report: The authors present a case of a 60-year-old Caucasian female who developed a femoral-sided cyclops lesion after ACL repair. After initially achieving full range of motion (ROM) post-surgery, the patient later experienced a palpable clunk and extension loss 3-months postoperatively. While magnetic resonance imaging (MRI) was unremarkable, subsequent arthroscopy confirmed the diagnosis, leading to successful lesion excision and notchplasty.
Conclusion: A high index of suspicion for cyclops lesions is critical in patients presenting with a clunk with terminal extension after ACL repair, even in the absence of MRI evidence. Prompt recognition and intervention are crucial, as demonstrated by the removal of the lesion and notchplasty, which led to full recovery of symptoms and ROM of the knee. The authors aim to broaden the limited existing knowledge of inverted cyclops lesions by presenting a detailed case report of a patient after an ACL repair.
Keywords: Anterior cruciate ligament repair, sports, inverted cyclops arthroscopy, knee.
Reconstruction of the anterior cruciate ligament (ACL) is a frequently performed procedure known for its consistent and reliable outcomes. A relatively common cause of loss of extension following ACL reconstruction is a cyclops lesion. It was first described in the literature by Jackson and Schaefer [1], who defined it as localized anterior arthrofibrosis. The lesion itself is characterized by a fibrous nodule with central granulation tissue, most commonly located anterolateral to the tibial tunnel. Early impingement of the nodule on the roof of the intercondylar notch limits knee extension [1,2]. On arthroscopy, the lesion has a head-like appearance with a focal area of reddish-blue discoloration due to venous channels that resemble an eye, hence the name “Cyclops” [3]. When a cyclops lesion is associated with a loss of extension of the knee with or without an audible or palpable clunk in terminal extension, it is termed a “cyclops syndrome.”[1] The incidence of cyclops syndrome has been reported to be between 1% and 10% of all ACL reconstructions [4-6]. The diagnostic modality of choice is imaging through magnetic resonance imaging (MRI). The sensitivity, specificity, and accuracy of revealing a cyclops lesion on MRI are 85.0%, 84.6%, and 84.8%, respectively [7]. While the most common location of the cyclops lesion is anterolateral to the tibial tunnel, there are five documented case reports in the literature of femoral-sided, or inverted, cyclops lesions [8-12]. Currently, there is no existing literature that documents the development of a femoral-sided cyclops lesion following an ACL repair, as opposed to reconstruction [9,11,12] or femoral fracture [8,10]. In this report, we aim to broaden existing knowledge of inverted cyclops lesions by presenting a detailed case report of a patient with an inverted cyclops lesion after an ACL repair.
A 60-year-old Caucasian female sustained a left proximal one-third Sherman type II ACL tear after twisting her left knee while playing with her grandson. MRI demonstrated an acute appearing, complete tear of the proximal 1/3 of the ACL, a small impaction fracture along the posterior margin of the lateral tibial plateau, and a grade 1 medial collateral ligament sprain (Fig. 1). Examination of the left knee was limited due to pain. The patient had 30–100° of motion with a 1+ positive Lachman’s and positive anterior drawer. A thorough discussion regarding ACL reconstruction versus repair was completed, and the patient decided to pursue repair due to age and functional status, with location of tear.
ACL repair was performed 5 weeks after the initial injury. Examination under anesthesia revealed +1 Lachman and positive anterior drawer. The repair was performed using three luggage tag stitches attached to the ACL and anchored into the femoral origin using a suture anchor. An accessory anterior medial superior portal was utilized to anchor the opposite end of the suture anchor into the standard tibial insertion site. This was done in 90° of flexion. Immediate post-operative examination under anesthesia demonstrated stable Lachman, anterior drawer, and dial tests. There were no intraoperative complications. Intraoperative endoscopy images are shown in Fig. 2.

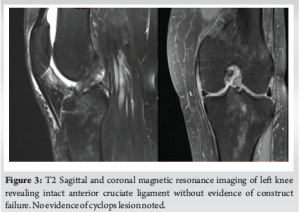
The patient continued to show improvement at both the 2-week and 6-week, follow-up visits. She progressed well with therapy, achieving a full range of motion (ROM) of her knee without limitations or instability. However, approximately 3 months postoperatively, she developed a palpable, audible clunking sensation with terminal extension of the knee. Examination was unremarkable with the exception of an audible clunk from 20° flexion to terminal extension. An MRI was repeated, demonstrating an intact ACL without evidence of construct failure (Fig. 3). Due to timing being 3 months post-operative with audible clunking, a cyclops lesion was suspected. The decision was made to proceed with surgery for manipulation under anesthesia and arthroscopic assessment with possible cyclops resection.
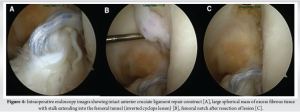
Examination under anesthesia demonstrated full extension with palpable clunk, 130° of flexion, a 1+ Lachman’s and a negative pivot shift. Intraoperatively, all compartments were intact, and the ACL appeared well-healed with the internal brace in place (Fig. 4a). A large spherical mass of excess fibrous tissue was discovered in the roof of the femoral intercondylar notch – the inverted cyclops lesion (Fig. 4b). The lesion clearly engaged with the anterior tibia with terminal extension and was suspected to be responsible for the patient’s clunking sensation. A notchplasty was performed following debridement of the lesion (Fig. 4c). The patient reported immediate resolution of her symptoms when awaking in the recovery unit. At 6 months following excision of the lesion and 10 months after index ACL repair, the patient had full terminal extension without pain or clicking and full flexion to 130°. She returned to the normal progression of activities with physical therapy.
The cyclops lesion was first described by Jackson and Schaefer in 1990 [1]. They defined it as the fibrous nodule of granulation tissue that maturated in a way similar to a healing scar and occasionally developed cartilaginous or bony tissue that formed anterolateral to the tibial tunnel entrance [1]. The origin of the cyclops lesion was initially attributed to bone and cartilage residues from tunnel drilling. Over time, additional theories emerged, suggesting that factors such as compressive loading, microtrauma, micromotion, partial injury to the ACL graft, and irritation from impingement could also contribute [1,2,8,12]. It is now widely accepted that the origin of the cyclops lesion is multifactorial [2]. A femoral-sided cyclops lesion has been described in five other case reports [8-12]. Hart et al. were the first to describe this unique anatomic variant of the cyclops lesion in 2004. They detailed a case of an adolescent who developed an inverted cyclops lesion following a femoral physeal fracture [8]. This lesion was removed, and the patient recovered with full active extension. In their 2009 study, Rubin et al. described a case of extension loss due to an inverted cyclops lesion following ACL reconstruction in a manual laborer, who developed an extension deficit during physical therapy 3 months post-surgery [12]. MRI revealed a fibrous nodule impinging on the femoral notch, which was successfully removed arthroscopically, providing immediate symptom relief. Similarly, Kambhampati and Ware reported a 35-year-old woman who, after ACL reconstruction with a hamstring graft, developed a fixed flexion deformity due to an inverted cyclops lesion; arthroscopic excision and notchplasty led to significant improvement in her knee function [9]. Another case by Kambhampati and Shanmugasundaram involved a 40-year-old man with chronic knee stiffness and an inverted cyclops lesion, resulting from a motor vehicle accident [10]. After excision of the lesion, as well as heterotopic bone, knee ROM improved significantly to 0–120°. Only one case in the literature describes an inverted cyclops lesion without loss of terminal knee extension, involving an 18-year-old woman who developed knee pain and swelling 20 months after ACL reconstruction but returned to normal activities following arthroscopic removal of the fibrous lesion [11]. This case stands out as the first to describe an inverted cyclops lesion following ACL repair. Unlike other reports, the patient’s post-operative MRI failed to demonstrate the presence of the cyclops lesion. This underscores the importance of a high index of suspicion for this lesion in a patient presenting with an audible or palpable clunk following ACL repair. The average time between ACL reconstruction and excision of a cyclops lesion is 16 weeks, with a range of 8–36 weeks [1]. This patient’s case, occurring at 12 weeks, falls within this timeframe. Similar to patients with a traditional cyclops lesion, our patient experienced a loss of terminal knee extension. Following removal of the lesion and notchplasty, our patient regained the full range of movement of the knee. Various strategies have been recommended in the literature to reduce the incidence of cyclops lesions. These include utilizing minimally invasive surgical techniques, ensuring proper tunnel positioning to prevent impingement, minimizing debris creation and thoroughly clearing debris after tunnel placement, early post-operative mobilization, and performing notchplasty [10,13,14]. There are some inherent limitations to this case report. Although the sensitivity of MRI for diagnosis tibial sided cyclops is reported above, there are no studies in the literature assessing MRI sensitivity for diagnosis femoral sided cyclops. This potentially restricts the utility of imaging guidance in diagnosis. While arthroscopic appearance guided diagnosis, the lesion was not histologically analyzed to confirm fibrous cyclops tissue. In addition, the case report does not include comparative outcomes between ACL repair and reconstruction in the context of cyclops lesion formation, as this is the first report of cyclops lesion formation after ACL repair in the literature. Finally, the Level V (expert opinion/case report) evidence presented is inherently limited in strength and lacks the methodological rigor of higher-level clinical studies or trials.
A high index of suspicion for cyclops lesions is critical in patients presenting with a clunk with terminal extension after ACL repair, even in the absence of MRI evidence. Prompt recognition and intervention are crucial, as demonstrated in our case, where removal of the lesion and notchplasty led to the patient regaining the full range of knee movement. This case adds to the growing body of literature on inverted cyclops lesions and emphasizes the need for clinical vigilance in the post-operative care of ACL repair patients.
ACL repair is becoming an increasing popular procedure utilized by orthopedic surgeons throughout the world. Femoral-sided cyclops lesions are a rare anatomic variant of the well-described tibial cyclops lesion, which can be unremarkable on MRI scans. Early recognition and intervention can lead to full recovery of symptoms and knee ROM.
References
- 1. Jackson DW, Schaefer RK. Cyclops syndrome: Loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy 1990;6:171-8. [Google Scholar] [PubMed]
- 2. Tonin M, Saciri V, Veselko M, Rotter A. Progressive loss of knee extension after injury. Cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med 2001;29:545-9. [Google Scholar] [PubMed]
- 3. Dhanda S, Sanghvi D, Pardiwala D. Case series: Cyclops lesion – extension loss after ACL reconstruction. Indian J Radiol Imaging 2010;20:208-10. [Google Scholar] [PubMed]
- 4. Kambhampati SB, Gollamudi S, Shanmugasundaram S, Josyula VV. Cyclops lesions of the knee: A narrative review of the literature. Orthop J Sports Med 2020;8(8):2325967120945671. [Google Scholar] [PubMed]
- 5. Noailles T, Chalopin A, Boissard M, Lopes R, Bouguennec N, Hardy A. Incidence and risk factors for cyclops syndrome after anterior cruciate ligament reconstruction: A systematic literature review. Orthop Traumatol Surg Res 2019;105:1401-5. [Google Scholar] [PubMed]
- 6. Moran TE, Taleghani ER, Ruland JR, Ignozzi AJ, Hart J, Diduch DR. An analysis of the incidence, risk factors, and timing of development of cyclops lesions after anterior cruciate ligament reconstruction. Knee 2023;40:1-7. [Google Scholar] [PubMed]
- 7. Bradley DM, Bergman AG, Dillingham MF. MR imaging of cyclops lesions. AJR Am J Roentgenol 2000;174:719-26. [Google Scholar] [PubMed]
- 8. Hart AJ, Eastwood DM, Dowd GS. Fixed flexion deformity of the knee following femoral physeal fracture: The inverted cyclops lesion. Injury 2004;35:1330-3. [Google Scholar] [PubMed]
- 9. Kambhampati S, Ware H. Inverted cyclops lesion after anterior cruciate ligament reconstruction. Ann R Coll Surg Engl 2012;94:e99-100. [Google Scholar] [PubMed]
- 10. Kambhampati SB, Shanmugasundaram S. Inverted cyclops lesion of the knee associated with a supracondylar femoral nail: A case report. Cureus 2019;11:e5902. [Google Scholar] [PubMed]
- 11. Pyrko P, Strauss EJ, Struhl S. Inverted cyclops lesion without extension block: A case report and literature review. Bull Hosp Jt Dis (2013) 2015;73:61-4. [Google Scholar] [PubMed]
- 12. Rubin LE, Yeh PC, Medvecky MJ. Extension loss secondary to femoral-sided inverted cyclops lesion after anterior cruciate ligament reconstruction. J Knee Surg 2009;22:360-3. [Google Scholar] [PubMed]
- 13. Delincé P, Krallis P, Descamps PY, Fabeck L, Hardy D. Different aspects of the cyclops lesion following anterior cruciate ligament reconstruction: A multifactorial etiopathogenesis. Arthroscopy 1998;14:869-76. [Google Scholar] [PubMed]
- 14. Balcarek P, Sawallich T, Walde TA, Ferlemann KG, Wachowski M, Stürmer KM, et al. Einfluss des zyklops-syndroms nach vorderer kreuzbandplastik auf das klinische ergebnis [Influence of cyclops syndrome after anterior cruciate ligament reconstruction on the functional outcome]. Sportverletz Sportschaden 2008;22:220-4. [Google Scholar] [PubMed]