A double Hoffa fracture, an uncommon coronal plane fracture involving both femoral condyles, can be optimally managed with precise anatomic reduction and rigid internal fixation using cancellous screws, followed by an early, structured mobilization protocol, thereby facilitating favorable functional recovery.
Dr. Vipin Gupta, Central Institute of Orthopedics, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110029, India. E-mail: vipingupta87@gmail.com
Introduction: Hoffa fractures are rare intra-articular fractures of the distal femur in the coronal plane, typically affecting a single femoral condyle. A bicondylar involvement, essentially double Hoffa fractures, is exceedingly uncommon and rarely documented, especially in the absence of metaphyseal comminution.
Case Report: We present the case of a 25-year-old male who sustained an isolated bicondylar Hoffa fracture following a motorcycle accident. Radiographs and computed tomography (CT) imaging confirmed isolated coronal plane fractures of both femoral condyles (AO 33-B3), without metaphyseal comminution or intercondylar extension. The fracture was managed through a single medial parapatellar approach, using 5 cannulated screws and 2 headless Herbert screws. Post-operative rehabilitation involved early mobilization and progressive weight bearing. At 2 years follow-up, the patient demonstrated excellent functional recovery with a full range of motion (0–140°), no extensor lag, and pain-free full weight-bearing.
Conclusion: This case highlights the role of precise anatomical reduction, CT evaluation, and early mobilization in managing complex distal femur fractures. This report adds to the limited literature on bicondylar Hoffa fractures without metaphyseal comminution.
Keywords: Femoral fractures, fractures, intra articular, fracture fixation, internal, knee joint/surgery, wounds and injuries.
Hoffa fractures, first described by Friedrich Busch in 1869 and later detailed by Albert Hoffa in 1904, are intra-articular fractures of the distal femur occurring in the coronal plane, typically involving the lateral femoral condyle. They account for approximately 0.65% of all femoral fractures and 8.7–13% of all distal femoral fractures. The injury mechanism typically involves a direct anteroposterior force applied to a flexed knee, with abduction predisposing to lateral condyle fractures and adduction associated with medial condyle involvement [1]. Although both lateral and medial condyles can be involved, there is a preponderance of lateral Hoffa fracture due to physiological valgus [2]. Cannulated screw fixation is favored for its minimally invasive nature, reduced risk of complications, and ability to provide stable and reliable fracture fixation [3]. Being a rare entity, the Hoffa fracture usually involves only one of the femoral condyles. We present a rare case involving both femoral condyles-essentially a double Hoffa fracture-with both fragments displaced but without metaphyseal comminution or intercondylar involvement. Till now, very few cases have been described in the literature with a similar presentation, highlighting the rarity of this fracture pattern.
Clinical history
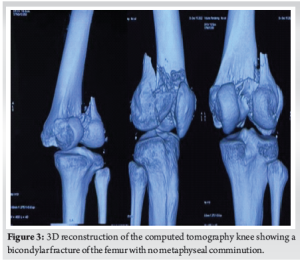
A 25-year-old male presented to the emergency department with a history of a fall from a motorcycle following a road traffic accident. Following initial resuscitation, plain radiographs of the knee were obtained, revealing a distal femur fracture (Fig. 1). Due to the complex nature of the injury and suspected intra-articular involvement, a computed tomography (CT) scan of the knee with 3D reconstruction was performed. It revealed isolated coronal fractures of both femoral condyles, confirming the diagnosis of a double Hoffa fracture (Fig. 2 and 3). Both the fracture fragments were separated, with no bony bridge connecting the two. The fracture was classified as AO 33-B3. After appropriate pre-operative planning and preparation, the patient was taken up for surgery.
Management
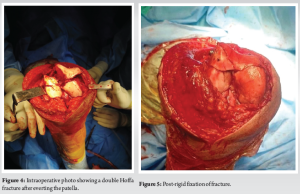
The fracture was approached through a standard medial parapatellar approach to gain access to both Hoffa fragments. The fracture site was exposed by everting the patella laterally and fully flexing the knee (Fig. 4). Anatomical reduction of the fracture fragments was obtained using 2 mm K-wires as joysticks for reduction in the distal fragments. Interfragmentary reduction clamps were deliberately avoided to prevent iatrogenic damage to the cartilage, considering the large degree of shear forces on the fracture fragments. Condylar reconstruction was done using 4 cannulated cancellous screws (7 mm), with 2 screws each passed anteroposteriorly to fix the lateral and medial femoral condyles. One additional screw was passed from lateral to medial to secure a metaphyseal beak fragment on the lateral side. The lateral Hoffa was found to have an additional fracture line, which warranted fixation with two additional headless Herbert screws (Fig. 5 and 6). The fixation construct was found to be stable throughout the knee range of motion (ROM). Post-operatively, static quadriceps strengthening alongside knee ROM exercises was started from the 3rd post-operative day with a hinged knee brace.

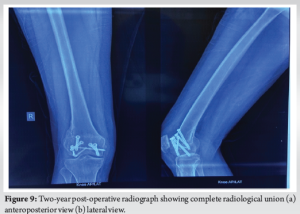
The patient was followed up in the outpatient department at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years. Toe touching weight-bearing was started at 2 weeks and gradually progressive knee ROM was allowed through the hinged knee brace. At 6 weeks, the patient had regained a ROM of 5–90° and weight-bearing to tolerance was encouraged on the affected limb alongside regular physiotherapy sessions. At 3 months, the patient had achieved a ROM of 5–100°, which further improved to 0–120° at 6 months. At 1 year, the ROM was 0–140° with full weight-bearing on the affected limb. At 2 years post-operatively, the X-ray showed complete radiological union and the patient had achieved full ROM, with no extensor lag and was able to bear full weight on the affected limb with little to no pain in the affected limb (Fig. 7 and 8).
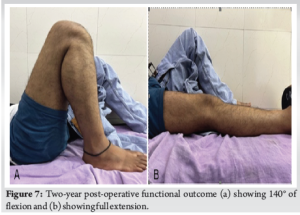

The mechanism involved in a double Hoffa fracture typically involves an axial load on a flexed knee, resulting in shear forces sufficient to split both femoral condyles in the coronal plane. The exact mechanism causing a simultaneous fracture in both the femoral condyles is largely unknown. The most probable mechanism can be assumed to be a posterior and upward-directed force without any varus or valgus component, in a flexed knee [4]. CT imaging is essential for accurate classification and planning, as conventional radiographs may not reveal the exact fracture pattern, especially if the fracture is undisplaced. Given the unique fracture morphology in our patient – a true double Hoffa fracture without metaphyseal comminution or intercondylar extension – an individualized approach was necessary. Ul Haq et al., described the management of a similar case of a conjoint bicondylar Hoffa fracture, where both the femoral condyles were joined by a bridge of intact bone, fixed with cancellous screws, leading to a favorable outcome [4]. Zeebregts et al. and Papadopoulos et al., also described similar cases treated through separate medial and lateral approaches, fixed with 6.5 mm cannulated screws [5,6]. In contrast, our approach through a single medial parapatellar exposure facilitated adequate visualization of both fractured condyles and reduced soft tissue damage. Furthermore, a direct midline approach allowed us to put screws perpendicular to the fracture line, in accordance with principles of fracture fixation. Agarwal et al., managed such bicondylar coronal fractures with cortical lag screws and plating [7]. However, given the absence of metaphyseal comminution in our case, plating was not deemed necessary. Dua and Shamshery also reported a similar bicondylar Hoffa fracture managed successfully using a Swashbuckler approach, and five 6.5 mm cannulated screws for fixation of the Hoffa fragments, augmented with a condylar buttress plate on the lateral aspect [8]. Similarly, Giotikas et al., used a dual plating technique in the presence of metaphyseal comminution – a feature not seen in our patient [9]. Our decision to use multiple screws on both sides was guided by the presence of subtle comminution and the need for rigid fixation to allow early mobilization. The functional outcome in our patient was remarkably favorable, emphasizing the importance of anatomical reduction, rigid fixation, and early rehabilitation [10]. The ability to regain full ROM without extensor lag by 6 months reflects both the stability of fixation and the biological healing potential in young adults. (Fig. 9).
This case highlights two aspects: Bicondylar non-conjoint involvement of the distal femur and favorable early functional outcome despite fracture complexity. The successful outcome demonstrates that appropriate surgical technique with stable fixation can achieve favorable results in complex fracture patterns, contributing valuable insights to the limited literature on double Hoffa fractures.
Double Hoffa fractures are rare. Whenever suspected, a CT with 3D reconstruction must be done to elicit the fracture pattern. In the absence of metaphyseal involvement, this fracture can be managed with cannulated cancellous screws alone, using a single incision approach. Early rehabilitation and mobilization are crucial for a good recovery.
References
- 1.Kurahatti A, Seenappa H, Shanthappa AH, Nagakumar JS. The functional and radiological outcome of Hoffa’s fracture treated with cannulated cancellous screws. Cureus 2022;14:e23829. [Google Scholar | PubMed]
- 2.Holmes SM, Bomback D, Baumgaertner MR. Coronal fractures of the femoral condyle: A brief report of five cases. J Orthop Trauma 2004;18:316-9. [Google Scholar | PubMed]
- 3.Huang C, Fu Z, Wang Q, You R, Zhao F. Treatment of the Hoffa fracture of the lateral femoral condyle with cannulated screws in combination with an anti-gliding steel plate, a retrospective observational study. BMC Surg 2022;22:354. [Google Scholar | PubMed]
- 4.Ul Haq R, Modi P, Dhammi I, Jain AK, Mishra P. Conjoint bicondylar Hoffa fracture in an adult. Indian J Orthop 2013;47:302-6. [Google Scholar | PubMed]
- 5.Zeebregts CJ, Zimmerman KW, Ten Duis HJ. Operative treatment of a unilateral bicondylar fracture of the femur. Acta Chir Belg 2000;100:104-6. [Google Scholar | PubMed]
- 6.Papadopoulos AX, Panagopoulos A, Karageorgos A, Tyllianakis M. Operative treatment of unilateral bicondylar Hoffa fractures. J Orthop Trauma 2004;18:119-22. [Google Scholar | PubMed]
- 7.Agarwal S, Giannoudis PV, Smith RM. Cruciate fracture of the distal femur: The double Hoffa fracture. Injury 2004;35:828-30. [Google Scholar | PubMed]
- 8.Dua A, Shamshery PK. Bicondylar Hoffa fracture: Open reduction internal fixation using the swashbuckler approach. J Knee Surg 2010;23:21-4. [Google Scholar | PubMed]
- 9.Giotikas D, Nabergoj M, Krkovic M. Surgical management of complex intra-articular distal femoral and bicondylar Hoffa fracture. Ann R Coll Surg Engl 2016;98:e168-70. [Google Scholar | PubMed]
- 10.Singh R, Singh RB, Mahendra M. Functional outcome of isolated hoffa fractures treated with cannulated cancellous screw. Malays Orthop J 2017;11:20-4. [Google Scholar | PubMed]