Locking plates used as external fixators can serve as an effective and patient-friendly alternative to traditional external fixation in tibial fractures with soft-tissue compromise. This technique provides stable fixation, allows early rehabilitation, and minimizes complications, making it especially valuable in complex or high-risk fracture scenarios.
Dr. Ismail Pandor, Department of Orthopaedics, Krishna Vishwa Vidyapeeth, Karad, Maharashtra, India. E-mail: i.pandor07@gmail.com
Introduction: Treating metadiaphyseal tibial fractures with compromised soft tissues remains a surgical challenge. While traditional external fixators are widely used, locking compression plates (LCPs) applied externally as fixators offer a promising alternative due to their low-profile design and angular stability.
Objectives: The objective is to evaluate clinical outcomes, union rates, complications, and functional recovery in patients treated with locking plate external fixators (LPEFs) for metadiaphyseal tibia fractures.
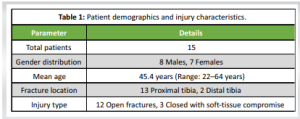
Materials and Methods: This prospective study of 15 adult patients with open or soft-tissue-compromised metadiaphyseal tibia fractures was conducted over 12 months. All patients were managed using LCP as an external fixator. Radiological union, time to weight-bearing, infection rates, reoperation need, and functional outcomes (knee society score [KSS] and the American Orthopaedic Foot and Ankle Society [AOFAS]) were assessed.
Results: The mean time to union was 12.1 weeks, with a union rate of 90%. One superficial infection (6.6%) and one reoperation (6.6%) were noted. The final follow-up revealed excellent functional outcomes: Mean KSS score of 85 ± 5 and AOFAS of 81 ± 4.
Conclusion: LPEF offers a viable fixation method in managing complex tibial fractures with soft-tissue compromise, allowing early mobilization, fewer complications, and excellent functional outcomes. Larger studies are needed to validate its widespread adoption.
Keywords: External fixator, locking plates, tibia fracture.
Tibial metadiaphyseal fractures represent complex injuries frequently resulting from high-energy trauma, including motor vehicle accidents or industrial incidents. The subcutaneous location of the tibia makes it vulnerable to soft-tissue compromise, complicating the management of such fractures [1]. Open fractures, as classified by Gustilo-Anderson, or closed fractures with soft-tissue damage per Tscherne classification, pose significant risks, including infection and non-union. Traditional external fixators such as monolateral or Ilizarov devices remain standard treatment options, especially when internal fixation is contraindicated. However, these devices are bulky, less comfortable, and associated with higher risks of pin tract infections and patient dissatisfaction. Locking compression plates (LCP), used externally as fixators in a technique called supracutaneous plating, offer a promising alternative. First described by Kloen et al., this technique minimizes soft-tissue disruption and provides angular stability with a low-profile design. Biomechanical studies, including those by Ang et al. and Kloen P ET al , support the superior torsional stiffness and comparable axial stability of external LCPs [2,3]. More recent studies by Hadeed et al., Jiang et al., and Zhang et al. further support the safety and efficacy of externalized LCPs in the treatment of open and infected fractures [4-6]. In addition, Patel et al. demonstrated positive outcomes in polytrauma patients using this approach [7], and Mishra et al. emphasized the utility of locking plate external fixator (LPEF) in geriatric populations with osteoporotic bone [8]. Despite clinical promise, widespread use of LPEF is limited by cost, learning curve, and lack of large-scale trials. Our prospective study aims to present clinical outcomes and reinforce the utility of LPEF in managing soft-tissue-compromised tibial fractures.
This prospective interventional study was conducted at the Department of Orthopaedics, Krishna Vishwa Vidyapeeth, Karad, between January 2023 and December 2023. Institutional ethics committee approval and informed consent were obtained from all participants before inclusion.
Sample size
Fifteen patients were included using convenience sampling due to the specific and relatively rare indication for LPEF in the clinical setting.
Inclusion criteria
- Age ≥18 years
- Open (Gustilo Type II/III) or closed (Tscherne Grade II/III) metadiaphyseal tibial fractures
- Soft-tissue compromise contraindicating internal fixation
- Ability to comply with follow-up.
Exclusion criteria
- Skeletally immature patients
- Diaphyseal or intra-articular fractures
- Pathological fractures
- Severe comorbidities affecting healing
- Lost to follow-up.
Surgical technique
The procedure is typically performed under spinal or general anesthesia with the patient in a supine position on a radiolucent table. The affected limb is prepared and draped in a sterile fashion, and tourniquet application may be used depending on the wound status and surgeon preference.
- Wound assessment and debridement:
-
- A thorough examination of the injury is done to assess soft-tissue condition.
- A meticulous debridement of necrotic tissue, debris, and contaminants is performed. In open fractures, this step is critical to reduce infection risk.
- The wound may be extended as necessary to allow comprehensive debridement.
- Fracture reduction:
- Closed or minimally invasive indirect reduction techniques are used.
- Fluoroscopy is employed to assess alignment in both anteroposterior and lateral planes.
- Reduction is maintained using temporary external aids such as K-wires, reduction clamps, or manual traction.
- Plate selection and preparation:
- A long LCP appropriate for the fracture location (proximal, midshaft, or distal tibia) is selected.
- The plate should allow placement of at least 3–4 locking screws on either side of the fracture.
- The plate is contoured if needed and held 1.5–2 cm away from the skin surface.
- Application of the plate:
-
- The plate is placed on the anteromedial aspect of the tibia, parallel to the bone surface but outside the soft-tissue envelope.
- Provisional fixation is achieved using percutaneously inserted K-wires through the outer plate holes to maintain alignment and position.
- Screw insertion:
- Locking screws are inserted through the plate into the bone using stab incisions.
- Each screw is drilled and measured for length, ensuring bicortical purchase.
- A minimum of 3 screws are placed on each side of the fracture to ensure stability.
- Screw trajectory is carefully planned to avoid neurovascular structures and to maintain an appropriate screw-bone angle.
- Final assessment:
-
- Fluoroscopic confirmation is done to verify fracture alignment, screw placement, and construct stability.
- Wounds are irrigated and dressed. No deep sutures are typically required due to the minimally invasive nature.
- Post-operative protocol:
-
- Early mobilization of the ankle and knee is encouraged from day 1 post-operative.
- Non-weight-bearing ambulation is started by day 2 or 3.
- Pin site and screw track cleaning is performed daily to reduce the risk of superficial infections.
- Progressive weight-bearing is initiated once a bridging callus is seen on radiographs (typically around 8–10 weeks).
- Plate removal is performed in an outpatient setting once complete union is achieved.
- Follow-up and monitoring:
-
- Patients are reviewed every 6 weeks with clinical and radiological assessment.
- Final evaluation includes calculation of functional outcome scores (knee society score [KSS] or the American Orthopaedic Foot and Ankle Society [AOFAS]).
This surgical technique emphasizes soft-tissue preservation, mechanical stability, and early functional rehabilitation–key factors in managing complex tibial injuries with externalized internal fixation systems.
Outcome measure
- Union rate (radiographic consolidation across 3 cortices)
- Time to union (weeks)
- Infection rate (superficial or deep)
- Reoperation rate
- Functional outcome:
- Proximal tibia: KSS
- Distal tibia: AOFAS score.
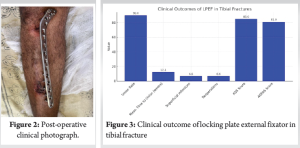
Case illustration
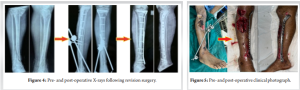
This is shown in Fig. 1 and 2.

A total of 15 patients were included in the study, comprising 8 males and 7 females, with a mean age of 45.4 years (range: 22–64 years). Majority of the fractures were located in the proximal tibia (13 cases), while the remaining 2 involved the distal tibia. Of the injuries, 12 were open fractures, and 3 were closed fractures with significant soft-tissue compromise as mentioned in Table 1 (Fig. 3). In our prospective study of 15 patients managed with locking plate external fixation for metadiaphyseal tibial fractures, favorable clinical outcomes were observed across key parameters. Union was achieved in 90% of cases, with a mean time to union of 12.1 weeks, indicating a relatively swift healing process. Only one patient (6.6%) experienced a superficial infection, which was effectively managed with conservative measures. Reoperation was required in one patient (6.6%) due to loss of alignment, which was successfully corrected with revision surgery. Functional outcomes were promising with an average KSS of 85 ± 5 for proximal tibial fractures and an AOFAS score of 81 ± 4 for distal tibial fractures, reflecting good joint function, mobility, and overall patient satisfaction. These results suggest that locking plate external fixation is not only a safe and biologically favorable option but also facilitates early rehabilitation and functional recovery in patients with soft-tissue-compromised tibial fractures. Patients began partial weight-bearing at 10 weeks, on average. One patient required realignment due to early fracture collapse, which was corrected with revision plating.
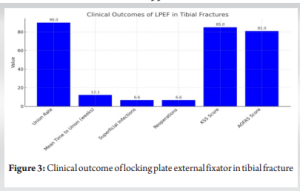
The results of this prospective study reaffirm the growing body of evidence that locking plates used as external fixators (LPEF) offer a reliable and often superior alternative in the management of complex tibial fractures. With a union rate of 90% and an average time to union of 12.1 weeks, our outcomes suggest that LPEF enables rapid consolidation and effective healing. Low complication rates–6.6% for both superficial infection and reoperation–further emphasize its safety in soft-tissue-compromised injuries. Biomechanically, LCPs provide angular stability through fixed-angle screw-plate constructs, promoting even stress distribution and resisting angular collapse. This configuration allows early mobilization and weight-bearing, key advantages over conventional monolateral or ring fixators. Several studies, including those by Ang et al. and Kloen P et al., have demonstrated the superior torsional stiffness and equivalent axial stiffness of externalized LCPs compared to traditional fixators [2,3]. Our findings are consistent with previously published clinical results. Panda and Panda, Gupta and Parimala, and Zhang and Ebrahim have reported similarly favorable union rates and functional recovery using LPEF, particularly in cases involving open fractures and infected non-unions [9-11]. Zhang et al. also emphasized the mechanical benefits of using femoral LCPs externally due to their increased rigidity, an approach we adopted in selected patients.
LPEF’s low-profile configuration significantly enhances patient comfort, improves hygiene at the implant site, and reduces soft-tissue disruption. It does not cross soft tissues, thereby reducing risks of tethering, skin irritation, and deep pin tract infections–common with conventional external fixators. These design advantages result in better compliance with post-operative care and improved overall satisfaction [4,5]. Another major advantage is the ease of hardware removal, often performed under local anesthesia in outpatient settings, thus reducing cost and avoiding hospital admission. Its applicability in polytrauma scenarios and utility in staged protocols make it a flexible tool for orthopedic trauma surgeons [6,7]. However, limitations must be acknowledged. LPEF systems are generally more expensive than traditional rods and pins, posing a challenge in resource-limited settings. In addition, they require a steeper learning curve due to the technical demands of percutaneous screw placement and plate contouring. Training and surgical familiarity are essential for achieving optimal outcomes. Our experience also supports the role of LPEF in salvage procedures. One patient initially treated with a conventional external fixator developed malalignment and soft-tissue breakdown. Successful revision with LPEF led to satisfactory alignment and uneventful healing–highlighting its value as a rescue technique as shown in Fig. 4 and 5. While our study has limitations, including a small sample size and lack of a comparative control group, the consistency of favorable outcomes across multiple variables suggests that LPEF may reduce the need for staged internal fixation, accelerate rehabilitation, and lower the complication burden in appropriately selected cases. Further multicenter randomized studies are warranted to establish LPEF as a mainstream strategy for managing high-risk tibial fractures.
Locking plate external fixation is an effective, biologically favorable, and technically reproducible method for managing metadiaphyseal tibial fractures in the setting of soft tissue compromise. It ensures reliable union, early mobilization, and low complication rates. The technique may redefine external fixation protocols in orthopedic trauma care, particularly for open or complex fractures. Further large-scale comparative and biomechanical studies are warranted to establish LPEF as a standard of care.
Locking plate external fixation (LPEF) offers a safe, low-profile, and biologically friendly alternative to conventional external fixation in metadiaphyseal tibial fractures with soft-tissue compromise. It facilitates early mobilization, improves patient comfort, and demonstrates excellent union and functional outcomes with minimal complications.
References
- 1. Rockwood CA, Green DP, Bucholz RW, Heckman JD, Court-Brown CM. Rockwood and Green’s Fractures in Adults. 8th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2015. [Google Scholar] [PubMed]
- 2. Kloen P, Doty SB, Gordon E, Helfet DL. Supracutaneous plating: An overview of techniques and outcomes. J Orthop Trauma 2012;26:234-9. [Google Scholar] [PubMed]
- 3. Ang BF, Chen JY, Yeo NE, Chua D, Chou SM, Lo NN, et al. Externalised locking compression plate as an alternative for unstable fractures. Bone Joint Res 2017;6:216-23. [Google Scholar] [PubMed]
- 4. Hadeed A, Garrigues GE, Belk JW, Werner BC. Clinical outcomes of externalized locking plate fixation in open and infected tibial fractures: A systematic review. J Orthop Trauma 2023;37:45-52. [Google Scholar] [PubMed]
- 5. Jiang L, Zhou Y, Wang H, Li Y, Liu C, Zhu Y. Efficacy of locking plates as external fixators for tibial fractures with severe soft tissue injury: A prospective cohort study. Int Orthop 2022;46:987-94. [Google Scholar] [PubMed]
- 6. Zhang Y, Zhang M, Tang X, Wang H, Xie Y, Li L. Supracutaneous locked plating for unstable tibial fractures: A multicentric evaluation. Injury 2021;52:2874-81. [Google Scholar] [PubMed]
- 7. Patel R, Mehta A, Desai N, Shah H. Externalized plating in polytrauma patients with lower limb fractures: A viable alternative. Eur J Orthop Surg Traumatol 2020;30:1259-65. [Google Scholar] [PubMed]
- 8. Mishra P, Goyal M, Agarwal A, Sharma V. Locking plates as external fixators in elderly patients with compromised soft tissues. Geriatr Orthop Surg Rehabil 2023. [Google Scholar] [PubMed]
- 9. Gupta SV, Parimala SP. Locking compression plates as external fixators in open tibial fractures: A case series. Indian J Orthop 2016;50:34-40. [Google Scholar] [PubMed]
- 10. Panda SS, Panda D. Supracutaneous plating in open tibial fractures: A salvage procedure. Int J Med Res Health Sci 2016;5:62-7. [Google Scholar] [PubMed]
- 11. Zhang J, Ebrahim NA. Use of externalized locking compression plates in complex tibial fractures: A retrospective review. Orthop Surg 2019;11:183-9. [Google Scholar] [PubMed]