Tendoachilles xanthoma is known to have a high recurrence rate with subtotal resection and repair. Complete excision of the xanthoma and reconstruction of the defect with ipsilateral flexor hallucis longus tendon transfer is a reliable and effective procedure that offers good functional outcomes without any major complications.
Dr. Deepak Kumar Maley, Department of Orthopaedics, All India Institute of Medical Sciences Bibinagar, Telangana, India. E-mail: maleydeepak@gmail.com
Introduction: Tendoachilles xanthomas are rare and generally asymptomatic swellings of tendoachilles. They are believed to be formed due to defects in lipid metabolism. Sometimes, these swellings become inflamed and become painful. If non-operative management fails, these patients are considered for surgery.
Case Report: A 25-years-old male patient presented with complaints of progressive swellings on the posterior aspect of both heels for the past 5 years. The left leg swelling was painful for the past 6 months. After thorough evaluation, the patient was diagnosed with bilateral tendoachilles xanthoma with gout. Complete excision of the left xanthomatus tendoachilles and reconstruction of the defect with Flexor hallucis longus (FHL) tendon transfer was done. At 3 months, 6 months and 1 year follow-up; the patient was highly satisfied with the procedure, could walk normally, and stands on the tip of the toes.
Conclusion: Complete excision of the xanthoma and reconstruction of the defect is associated with reduced recurrence rates and complete functional restitution. Reconstruction with ipsilateral FHL tendon transfer is a reliable and effective procedure offering a good functional outcome without any complications.
Keywords: Tendon xanthoma, achilles tendon, benign tumor, lipid metabolism.
Tendon xanthomas are benign swellings of tendons, formed due to the accumulation of lipids within the tendons [1]. Tendoachilles and patellar tendons are the common sites to be involved and extensor tendons of the hands, peroneal tendons, and triceps tendons are some less commonly involved [2]. Tendoachilles xanthomas occur due to genetic defects in lipid metabolism and are usually associated with high blood cholesterol levels [3]. In general, tendoachilles xanthomas are bilateral and asymptomatic except for the uncomfortable large swellings that may cause cosmetic and footwear problems. Rarely, these swellings become painful, lead to weakness in plantar flexion and gait abnormalities [2]. Most of these cases are managed non-operatively with analgesics, lipid-lowering drugs, such as statins and physiotherapy/exercises. Cases not responding to medical management are treated surgically with subtotal excision and repair or complete excision of the tendoachilles xanthoma, followed by reconstruction of the defect with tendon or fascial grafts or tendon transfers. Commonly used grafts for reconstruction include semitendinosus tendon, tensor fascia lata, peroneus brevis tendon transfer, and flexor hallucis longus (FHL) tendon transfer [2,4-6]. The authors present a case of bilateral tendoachilles xanthoma with gouty infiltration, with reconstruction with ipsilateral long FHL tendon transfer [7].
A 25-years-old male patient presented with complaints of progressive swellings on the posterior aspect of both heels and distal leg for the past 5 years (Fig. 1). Swellings were insidious in onset and were gradually progressive. The left leg swelling was painful for the past 6 months, associated with weakness of plantar flexion and antalgic gait. On clinical examination, a lobulated swelling of 9 × 15 cm was noted over the posterior aspect of the distal leg and multiple nodular swellings over both heels. Tenderness was present over the left heel. There was no local rise of temperature and there were no scars or sinuses over both heels. The right ankle has a full range of motion (ROM), whereas the left ankle has painful terminal limitation of ROM.
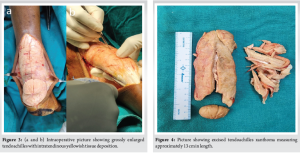
His complete blood picture and lipid profile were within normal limits, erythrocyte sedimentation rate was 20 mm/h, and uric acid level was 12.6 mg/dL. His serum homocysteine levels were elevated (21.38 umoL/L). Radiographs of both ankles showed soft tissue swelling in the region of tendoachilles without any bony involvement. Ultrasonography and magnetic resonance imaging showed well-defined soft tissue lesions along bilateral tendoachilles with well-circumscribed capsulated margins suggestive of tendoachilles xanthoma (Fig. 2). Fine needle aspiration cytology was performed and fluid from the nodular mass on the left heel was sent for biochemical analysis. Features consistent with Achilles tendon Xanthoma with gout were reported on histopathology and biochemical analysis. Patient was initially managed with analgesics, uric acid-lowering drugs, and ankle physiotherapy. As pain did not subside and the patient was uncomfortable while walking, he was planned for complete excision of the left tendoachilles xanthoma and reconstruction with ipsilateral FHL tendon transfer. Intraoperatively, the entire tendoachilles was bulky, nodular, and replaced by yellowish fat-like tissue from the musculotendinous junction to its insertion onto the calcaneum (Fig. 3). Complete excision of tendoachilles was performed (Fig. 4). Reconstruction of the tendoachilles was performed with the ipsilateral FHL tendon transfer with two-incision technique described by wiper (Fig. 5a, b, c, d). Histopathology showed tumor amidst fibromuscular tissue arranged in sheets composed of round to polygonal cells with round to oval nucleus and moderate to abundant amount of vacuolated cytoplasm and numerous multinucleated giant cells. Needle-shaped crystals were also seen. Features were consistent with the diagnosis of tendoachilles xanthoma along with gouty infiltration. Patient was given an above-knee plaster with ankle in 15° of plantar flexion for 8 weeks. Ankle ROM exercises and partial weight bearing were started at 8 weeks. Gradual strengthening exercises and full weight bearing were allowed at 12 weeks. Interim follow-up was done at 6 months, 1 year and at final follow-up after 3 years (before submission of the manuscript) there was no recurrence observed, patient could walk normally and could stand on tip toes on the operated limb (Fig. 6). Patient was so comfortable with the surgery and the outcome that he could manage his activities with the operated limb despite the presence of tendon xanthoma on the contralateral side for which a similar procedure is due.


Tendon xanthomas are formed due to the accumulation of lipid within the tendon substance, leading to increased size and decreased efficiency of the tendons. They are associated with hyperlipidemia and familial hypercholesterolemia. Tendoachilles is the most common tendon to get affected. Usually, tendoachilles xanthomas are asymptomatic, but sometimes these swellings get complicated by inflammation and edema, leading to achillodynia, functional loss, and rarely spontaneous ruptures [8]. Tendoachilles is also a common site for deposition of monosodium urate crystals-gout [9]. Occurrence of gouty crystal deposition in the setting of tendoachilles xanthomas is rare. When present along with tendon xanthoma, gouty crystals affect the structural arrangement of tendon fibers, further affecting the mechanical properties and function of the tendon [10]. Most of the previously published case reports on tendoachilles xanthoma have an elevated blood lipid profile, but the present patient had a normal lipid profile. Management of symptomatic tendoachilles xanthomas is challenging. Initial management is focused at lifestyle modifications, analgesics, physiotherapy exercises, and lipid-lowering drugs [4]. Eruptive xanthomas and tuberous xanthomas respond well with lipid-lowering drugs, but tendinous xanthomas respond slowly, taking years to decrease in size or even do not respond at all [11]. Hence, in non-responding symptomatic cases of tendoachilles xanthomas, surgical management remains the mainstay of treatment. Surgical management is mainly of two types. The first one is subtotal resection of tendoachilles xanthoma and repair of the remaining tendon. The second method is complete resection of the tendoachilles with xanthoma from the musculotendinous junction to insertion onto the calcaneum and reconstruction of the defect with a graft. Subtotal resection of xanthoma and repair of tendoachilles is associated with a high recurrence rate [12]. Complete resection of tendoachilles and reconstruction of the defect with graft is associated with less recurrence rates, but complete functional restitution is difficult due to lower graft strength when compared to normal tendoachilles. Different authors used different grafts for reconstruction of the defect and all yielded satisfactory outcomes. Senthil et al., used the tensor fascia lata from the opposite thigh, Sastri et al., used the ipsilateral peroneus longus tendon transfer, Oliva et al., used the ipsilateral autologous semitendinosis tendon graft, Moroney et al., used the FHL (f tendon in combination with the Bosworth turndown flap, and Sahu et al., used a short FHL graft fixed with a bioabsorbable screw into calcaneum [2,4-6,12]. We used the FHL graft to reconstruct the defect after completely resecting the tumorous tendoachilles akin to Wapner’s method [7]. Use of FHL tendon transfer for irrepairable tendoachilles tears is routinely practiced by us. It is preferred for reconstruction over other described techniques due to the following reasons. (1) It is the strongest available plantar flexor next to the gastrosoleus complex, (2) It fires in phase with the gastrosoleus, and (3) Adequate length of tendon can be obtained and its muscle is stronger compared to other tendon transfers. FHL was used in multiple studies for larger defects of tendoachilles created after debridement in chronic tendoachilles tears and insertional tendinopathies [13-15]. The defect created after resecting complete tendoachilles xanthoma is similar or bigger to a defect generated after debridement in chronic tendoachilles ruptures and chronic insertional tendinopathy. Hence, we preferred the FHL tendon transfer as an optimal treatment method for reconstruction in this case and it has yielded the best possible outcome.
Tendoachilles xanthoma is known to have a high recurrence rate with subtotal resection and repair. Complete excision of the xanthoma and reconstruction of the defect is associated with reduced recurrence rates. Reconstruction of the defect after complete excision of tendoachilles xanthoma is a challenging task. Reconstruction with ipsilateral FHL tendon transfer is a reliable and effective procedure that offers good functional outcomes without any major complications.
This case report offers key insights into the clinical features, imaging characteristics, and management of tendoachilles xanthomas. It highlights the importance of complete excision and Reconstruction of the defect with ipsilateral flexor hallucis longus tendon transfer in the management of this rarely symptomatic condition.
References
- 1. Brodsky JW, Beischer AD, Anat D, East C, Soltero E, Tint GS, et al. Cerebrotendinous xanthomatosis: A rare cause of bilateral Achilles tendon swelling and ataxia. A case report. J Bone Joint Surg Am 2006;88:1340-4. [Google Scholar] [PubMed]
- 2. Oliva F, Marsilio E, Mastrodonato F, Migliorini F, Maffulli N. Minimally invasive excision and reconstruction of Achilles tendon xanthoma using free autologous semitendinosus tendon transfer: A surgical technique. J Orthop Surg Res 2023;18:274. [Google Scholar] [PubMed]
- 3. Appuhamy GA, Munasinghe BM, Soysa LM, Nelson D, Ranmini PG, Pavithra WT, et al. A rare case of bilateral Achilles tendon xanthomas in a teenager, successfully treated with tendon sparing technique. Case Rep Orthop 2021;2021:1932763. [Google Scholar] [PubMed]
- 4. Senthil L, Jambu N, Chittaranjan S. Treatment of large recurrent bilateral xanthomatosis of Achilles tendon- a case report. J Orthop Case Rep 2015;5:11-4. [Google Scholar] [PubMed]
- 5. Sastri V, Ravindranath VS, Metikala S, Kumar M. Bilateral xanthomas of tendoachilles in a patient of cerebrotendinous xanthomatosis – a rare case report and review of literature. J Orthop Case Rep 2014;4:40-3. [Google Scholar] [PubMed]
- 6. Sahu NK, Nanda SN, Tripathy M, Samant S, Tripathy SK, Gachhayat AK. Xanthoma of tendoachilles: Management and follow-up. Case Rep Orthop Res 2021;4:166-72. [Google Scholar] [PubMed]
- 7. Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle 1993;14:443-9. [Google Scholar] [PubMed]
- 8. Tsouli SG, Kiortsis DN, Argyropoulou MI, Mikhailidis DP, Elisaf MS. Pathogenesis, detection and treatment of Achilles tendon xanthomas. Eur J Clin Invest 2005;35:236-44. [Google Scholar] [PubMed]
- 9. Mallinson PI, Reagan AC, Coupal T, Munk PL, Ouellette H, Nicolaou S. The distribution of urate deposition within the extremities in gout: A review of 148 dual-energy CT cases. Skeletal Radiol 2014;43:277-81. [Google Scholar] [PubMed]
- 10. Chhana A, Callon KE, Dray M, Pool B, Naot D, Gamble GD, et al. Interactions between tenocytes and monosodium urate monohydrate crystals: Implications for tendon involvement in gout. Ann Rheum Dis 2014;73:1737-41. [Google Scholar] [PubMed]
- 11. Shenoy C, Shenoy MM, Rao GK. Dyslipidemia in dermatological disorders. N Am J Med Sci 2015;7:421-8. [Google Scholar] [PubMed]
- 12. Moroney PJ, Besse JL. Resection of bilateral massive Achilles tendon xanthomata with reconstruction using a flexor hallucis longus tendon transfer and Bosworth turndown flap: A case report and literature review. Foot Ankle Surg. 2012 Sep;18(3):e25-8. doi: 10.1016/j.fas.2012.03.004. Epub 2012 May 11. PMID: 22857971. [Google Scholar] [PubMed] [CrossRef]
- 13. Martin RL, Manning CM, Carcia CR, Conti SF. An outcome study of chronic Achilles tendinosis after excision of the Achilles tendon and flexor hallucis longus tendon transfer. Foot Ankle Int 2005;26:691-7. [Google Scholar] [PubMed]
- 14. Wegrzyn J, Luciani JF, Philippot R, Brunet-Guedj E, Moyen B, Besse JL. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop 2010;34:1187-92. [Google Scholar] [PubMed]
- 15. Rahm S, Spross C, Gerber F, Farshad M, Buck FM, Espinosa N. Operative treatment of chronic irreparable Achilles tendon ruptures with large flexor hallucis longus tendon transfers. Foot Ankle Int 2013;34:1100-10. [Google Scholar] [PubMed]