This article outlines a novel technique for fixation of periprosthetic humeral shaft fractures about total elbow prosthesis without implant loosening by providing two case examples using posterior limited contact dynamic compression plating with the addition of medial and lateral cortical strut allografts and implant retention. Given the limited published data regarding this topic these cases offer a unique and beneficial fixation method for management of this complex issue.
Dr. Elise Ketelaar, Corewell Health Farmington Hills & Dearborn Orthopedic Surgery Residency, United States. 418 W Maxlow Ave Hazel Park, MI 48030, E-mail: ketelaa3@msu.edu, eliseketelaar22@gmail.com
Introduction: Expanding indications for total elbow arthroplasty in recent years have led to increased occurrence of complications, such as periprosthetic elbow fracture, which can occur in up to 12% of cases. Several management options for periprosthetic elbow fracture have been suggested in literature; however, there is currently no accepted guideline for treatment.
Case Report: We present two cases of periprosthetic humerus fractures without implant loosening multiple years after the index procedures. They were treated with open reduction internal fixation (ORIF) utilizing a plate with medial and lateral cortical strut femoral allografting with implant retention.
Conclusion: Two cases of periprosthetic humerus fractures about total elbow arthroplasties were successfully treated with ORIF with medial and lateral cortical strut augmentation. Treatment for periprosthetic elbow fractures should be tailored to each patient based on factors, such as stability of implant, bone stock, and patient goals.
Keywords: Periprosthetic, humeral shaft fracture, elbow arthroplasty, strut allograft, implant retention
Total elbow arthroplasty (TEA) is an effective procedure that has historically been utilized for the treatment of inflammatory arthropathies, such as rheumatoid arthritis [1,2]. In recent years, indications have expanded to include post-traumatic arthritis, osteoarthritis, acute distal humerus fractures, distal humerus non-unions, and reconstruction after tumor resection [1-7]. Elbow arthroplasty produces good clinical outcomes, including pain relief and functional improvement. TEA is a relatively uncommon arthroplasty procedure when compared to other joints; therefore, available literature is limited regarding management of complications, such as periprosthetic fracture, which occurs in up to 12% of cases [5]. Due to the general lack of high-quality evidence, there is no accepted treatment algorithm for periprosthetic elbow fractures. Present literature depicts several treatment options for periprosthetic fractures of the elbow, which include implant revision, open reduction internal fixation (ORIF), impaction grafting, strut augmentation, angle plate osteosynthesis, and tumor prosthesis [4,8-11]. However, current literature has not outlined the use of medial and lateral cortical strut allografts as a valid treatment option for periprosthetic humeral shaft fractures about total elbow arthroplasty. Management depends on several factors, such as location, implant stability, bone stock, and bone quality [4,8-10]. The purpose of this case report is to describe two cases of periprosthetic humerus fractures about total elbow arthroplasties without implant loosening multiple years after the index procedures. We describe a technique of ORIF utilizing posterior plate placement with medial and lateral cortical strut allografts.
Case 1
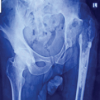
A 73-year-old woman presented with an isolated closed periprosthetic humerus fracture just proximal to the total elbow humeral stem after sustaining a ground-level fall. There was a fracture of the cement mantle and displacement of the humerus. She had undergone a TEA 2 years prior due to a comminuted displaced intra-articular fracture of the left distal humerus.
Case 2
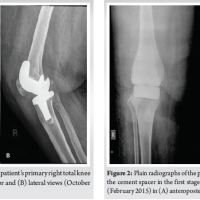
A 65-year-old female with a history of osteoarthritis and degenerative arthritis of the elbow presented with a left periprosthetic humeral fracture following a TEA for a previous distal humerus fracture 4 years prior.
For each patient, no infection or prosthetic loosening had been documented. Options for treatment were discussed. After considering the potential risks and complications, both patients elected to proceed with the surgery.
Technique
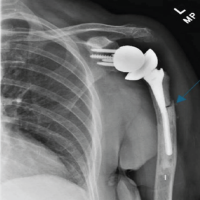
A similar technique was utilized for both cases due to the similar presentation of the periprosthetic humeral shaft fractures without implant loosening. A triceps splitting approach was used. The stability of the implants was tested intraoperatively and found to be well fixed to the distal fragment. In case 1, the cement mantle was fractured proximally and was able to be removed using an osteotome/rongeur. A limited contact dynamic compression plate was placed in the direct posterior position. A femoral strut allograft was split into two pieces longitudinally and placed medial and lateral to the plate and secured in place utilizing multiple cables (Fig. 1). Both patients were allowed to perform active and passive range of motion as tolerated, but were made non-weight-bearing.

Case 1 follow-up
At 6 weeks post-operatively, the patient’s incision was nicely healed with minimal swelling. Range of motion was 15° short of full extension, with flexion up to 130°. There was no restriction of pronation or supination. Anteroposterior and lateral X-ray views showed good alignment and no signs of hardware failure. Unfortunately, the patient was unable to complete subsequent follow-up due to death from unrelated reasons. See Fig. 2-4.


Case 2 follow-up
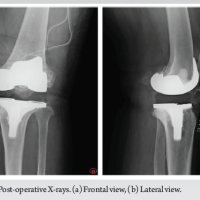
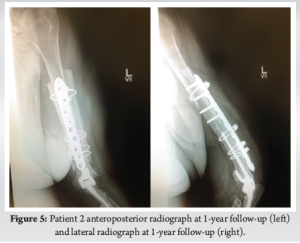
At 5 months, the patient’s incision was healed nicely. They were able to achieve 20° short of full extension and flex up to 120°. Pronation and supination were near the full range of motion. Sensation was intact with 5/5 strength in wrist, finger, and thumb extension. Anteroposterior and lateral X-rays showed proper consolidation of the fracture. At 1-year follow-up, the patient was able to use her arm and did not note any new problems. The left arm showed well-healed incisions with a similar functional range of motion. Anteroposterior and lateral X-rays confirmed proper consolidation of the fracture (Fig 5).
TEA has become increasingly common in recent years due to expanding indications [1,2]. As previously mentioned, these include: post-traumatic osteoarthritis, acute distal humerus fractures, distal humerus non-unions, and reconstruction after tumor resection [1-7]. Expanding indications for TEA has resulted in an increased prevalence of this procedure, leading to increased need for revision surgeries [2,3]. Up to 13.5% of total elbow arthroplasties require revision at some point [5]. Many complications leading to implant failure have been documented, the most recognized of which include implant loosening, periprosthetic fracture, implant failure, infection, triceps repair failure, and nerve palsy. Aseptic loosening may account for up to 38% of revisions, deep infection 19%, and periprosthetic fractures 12%. While aseptic loosening rates are lower for linked prostheses, there is no difference in infection and periprosthetic fractures between linked and unlinked prosthesis [5]. Data indicates that the majority of periprosthetic fractures occur in the setting of pre-existing loosening and the majority of prosthesis is loose at the time of revision [12]. Periprosthetic fractures around total elbow arthroplasties provide many unique challenges. Patients who experience periprosthetic fractures typically have poor bone quality, resulting in challenging management options. The elbow is a non-weight-bearing joint; therefore, principles of the hip and knee are not directly applicable. This is due to the fact that the elbow undergoes relatively more torsional load; thus, prioritizing torsional stability is essential in TEA. Many techniques for revision of periprosthetic fractures of the elbow have been proposed, depending on factors, such as bone quality, remaining bone stock, location of fracture, and stability of the prosthesis [4,8-10,12,13]. Strut allografts are useful particularly in the upper extremity where bone stock is limited [13]. Sanchez-Sotelo et al. [9], 2002 describe 11 periprosthetic fractures around a loose humeral component treated with revision arthroplasty and strut allograft augmentation, which resulted in high union rates and implant survival. Admittedly, these studies had 4 out of 14 patients demonstrate non-union, persistent loosening, or recurrent fracture, leaving room for improvement [9]. Alternatively, angle plate stable osteosynthesis may be utilized with or without evidence of prosthetic loosening, which was demonstrated in Fang et al., 2017 [10]. In cases of insufficient bone stock, strut augmentation with osteosynthesis may be the best option [11]. Finally, tumor prosthesis can be utilized as a last resort [9]. Our cases demonstrated two displaced periprosthetic distal third humeral shaft fractures without loosening. Due to the stability of the implants, treatment included ORIF utilizing a limited contact dynamic compression plate in the posterior position with medial and lateral cortical strut allograft augmentation and implant retention. No revision of either prosthesis was performed. Although one of the patients had limited follow-up, both achieved a functional range of motion without hardware failure.
In this paper, the authors reported on the presentation of two cases of periprosthetic humerus fractures about total elbow arthroplasties without implant loosening, which were successfully treated with ORIF with medial and lateral cortical strut augmentation. This case report illustrates that without the presence of implant loosening, periprosthetic elbow fractures can be managed with ORIF and cortical strut augmentation without the need for implant revision. This case report further demonstrates the importance of tailoring treatment of periprosthetic elbow fractures to fit each individual patient based on factors, such as location of fracture, stability of the implant, quality of bone stock, and patient goals.
Present literature depicts several management options for periprosthetic elbow fracture; however, to date, there is no case report available depicting the use of medial and lateral cortical strut allografting with retention of implants. This case report demonstrates a novel treatment option for the management of periprosthetic elbow fracture, with successful consolidation of the fractures and improved functionality for both patients.
References
- 1. Zhou H, Orvets ND, Merlin G, Shaw J, Dines JS, Price MD, et al. Total elbow arthroplasty in the United States: Evaluation of cost, patient demographics, and complication rates. Orthop Rev (Pavia) 2016;8:6113. [Google Scholar] [PubMed]
- 2. Macken AA, Prkic A, Kodde IF, Lans J, Chen NC, Eygendaal D. Global trends in indications for total elbow arthroplasty: A systematic review of national registries. EFORT Open Rev 2020;5:215-20. [Google Scholar] [PubMed]
- 3. Sanchez-Sotelo J. Total elbow arthroplasty. Open Orthop J 2011;5:115-23. [Google Scholar] [PubMed]
- 4. Kim JM, Mudgal CS, Konopka JF, Jupiter JB. Complications of total elbow arthroplasty. J Am Acad Orthop Surg 2011;19:328-39. [Google Scholar] [PubMed]
- 5. Prkic A, Welsink C, The B, Van Den Bekerom MP, Eygendaal D. Why does total elbow arthroplasty fail today? A systematic review of recent literature. Arch Orthop Trauma Surg 2017;137:761-9. [Google Scholar] [PubMed]
- 6. Jenkins PJ, Watts AC, Norwood T, Duckworth AD, Rymaszewski LA, McEachan JE. Total elbow replacement: Outcome of 1,146 arthroplasties from the scottish arthroplasty project. Acta Orthop 2013;84:119-23. [Google Scholar] [PubMed]
- 7. Triplet JJ, Kurowicki J, Momoh E, Law TY, Niedzielak T, Levy JC. Trends in total elbow arthroplasty in the Medicare population: A nationwide study of records from 2005 to 2012. J Shoulder Elbow Surg 2016;25:1848-53. [Google Scholar] [PubMed]
- 8. Dehghan N, Chehade M, McKee MD. Current perspectives in the treatment of periprosthetic upper extremity fractures. J Orthop Trauma 2011;25 Suppl 2:S71-6. [Google Scholar] [PubMed]
- 9. Sanchez-Sotelo J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after total elbow arthroplasty: Treatment with implant revision and strut allograft augmentation. J Bone Joint Surg Am 2002;84:1642-50. [Google Scholar] [PubMed]
- 10. Fang C, Yan CH, Yee D, Lau TW, Wong TM, Leung F. Restoration of humeral bone stock two years after internal fixation of a periprosthetic fracture with a loose stem: A report of two cases. JBJS Case Connect 2017;7:e17. [Google Scholar] [PubMed]
- 11. Chalidis B, Dimitriou C, Papadopoulos P, Petsatodis G, Giannoudis PV. Total elbow arthroplasty for the treatment of insufficient distal humeral fractures. A retrospective clinical study and review of the literature. Injury 2009;40:582-90. [Google Scholar] [PubMed]
- 12. Choo A, Ramsey ML. Total elbow arthroplasty: Current options. J Am Acad Orthop Surg 2013;21:427-37. [Google Scholar] [PubMed]
- 13. Fritsche CC, Deml O, Grossstuck R, Hofmann GO. [Short- and medium-term results of total elbow arthroplasty after trauma]. Z Orthop Unfall 2015;153:267-76. [Google Scholar] [PubMed]