Nonoperative management can be a viable and successful treatment option for certain periprosthetic humerus fractures, even in the rare setting of humeral stem deformation.
Dr. Edward G McFarland, Division of Shoulder and Elbow Surgery, Department of Orthopaedic Surgery, The Johns Hopkins University, 2360 West Joppa Road, Suite 306, Lutherville, Maryland 21093, USA. E-mail: emcfarl1@jhmi.edu
Introduction: Reverse total shoulder arthroplasty (RTSA) is increasingly performed, with a corresponding rise in associated complications such as periprosthetic fractures. Although implant failure and loosening are well documented, deformation of a humeral stem without loosening has not been previously reported.
Case Report: A 77-year-old woman, 9 years after an RTSA, presented with left shoulder pain after a fall. Initial radiographs revealed a transverse periprosthetic proximal diaphyseal fracture and a deformed humeral component. She was treated nonoperatively with range-of-motion exercises and pain management. One year later, radiographs confirmed fracture healing, and the patient had no pain and had regained full motion.
Conclusion: This is the first reported case of deformation of a humeral stem in a shoulder arthroplasty. Nonoperative management was successful for fracture healing.
Keywords: Trauma, reverse total shoulder arthroplasty, fracture, periprosthetic, humerus, varus, stem, bending.
The number of reverse total shoulder arthroplasty (RTSA) procedures in the United States is projected to reach 300,000 by the end of 2025 and is estimated to increase by another 122% by 2040 [1]. This increase is partly attributable to the procedure’s broadening indications, which include rotator cuff tear arthropathy, massive irreparable rotator cuff tear, proximal humerus fracture, glenoid bone loss, tumor, osteoarthritis, and failed anatomic shoulder arthroplasty [2,3]. However, as the number of RTSAs has grown since 2014, so has the incidence of procedure-associated complications. Complications following RTSA include neurologic injury, bleeding, infection, scapular notching, dislocation, hardware failure, acromial fracture, and periprosthetic fracture [4-6]. Periprosthetic fracture can be a devastating complication with substantial implications for patient outcomes [7,8]. The incidence of such fractures in RTSA is reported to range from 0.7% to 1.4% [9-12]. After a periprosthetic fracture, whether to perform revision surgery or treat the fracture nonoperatively is a challenging decision with important implications for the patient’s functional outcome. We present the case of a 77-year-old female patient who fell 9 years after undergoing RTSA and sustained a left periprosthetic transverse proximal diaphyseal fracture with deformation of the humeral implant stem but no fracture of the implant. She was treated nonoperatively and achieved a satisfactory functional result but had delayed healing of the fracture.
A 77-year-old, otherwise healthy woman presented to the clinic with left shoulder pain after she fell off a small stepping stool at her home and landed directly on her shoulder. Nine years earlier, she had sustained a complex and comminuted proximal humerus fracture, which was treated with open reduction and internal fixation. She subsequently developed a painful greater tuberosity fracture nonunion, which was treated successfully with RTSA with a cemented humeral stem (DJO Encore Reverse Shoulder Prosthesis, Austin, Texas). The patient had no prodromal pain in her arm before the fall, and she self-treated her pain with ice and acetaminophen. Eighteen days after the fall, she presented to the clinic with a complaint of pain in the shoulder with motion, especially while she was getting dressed or rolling over in bed at night. The patient reported no pain at rest in the arm or shoulder, and she had no tingling, numbness, neck pain, or any other injuries related to the fall. Upon physical examination, the patient’s left arm had mild swelling compared to the right but no ecchymosis. There was slight tenderness over her proximal humerus without crepitus or gross motion suggestive of a fracture. There was no tenderness over her joint line, scapula, or clavicle. She was neurovascularly intact with full and equal range of motion in her fingers, wrists, and elbows bilaterally. Radiographs revealed a transverse periprosthetic fracture at the proximal third of the diaphysis, with approximately nine degrees of varus angulation of the humeral component (Fig. 1). Given the stable fracture pattern, intact cement mantle, and minimal symptoms, the decision was made to treat the fracture nonoperatively. The patient was instructed to perform finger, wrist, elbow, and pendulum exercises during the first 3 months. She was prescribed acetaminophen and advised to use ice for pain management. A sling was offered, but she declined because she had had the fracture for several weeks and had only mild discomfort.
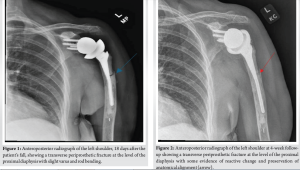
At 4-week follow-up, the patient reported improved arm pain and no longer had pain at night. She had discontinued icing and acetaminophen. Mild tenderness was noted over the mid-humerus fracture site, but she demonstrated satisfactory functional range of motion in abduction and rotation. She was neurologically intact and had full strength. Radiographs indicated reactive changes without displacement but minimal fracture healing (Fig. 2). She was advised to continue the same nonoperative plan and to minimize her strenuous activities. The patient was evaluated 14, 22, and 52 weeks after her injury to monitor for fracture healing and to ensure that no further deformation of the stem occurred. The patient demonstrated progressive improvements in pain and range of motion, returning to her usual activities, including housework and walking with her husband, without pain. At 52 weeks, radiographs confirmed complete fracture healing (Fig. 3), and she was released from our care with no further need for follow-up.
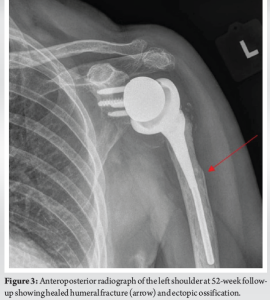
Although periprosthetic humerus fractures are relatively rare, their incidence has increased with the rising popularity of shoulder arthroplasty and the improved long-term durability of implants [13]. This case report illustrates the previously unreported transverse prosthetic fracture of a cemented humeral stem that was accompanied by a deformed humeral stem. Fortunately, the prosthesis remained functional, but the fracture healed over a more prolonged period than expected. Several classification systems exist for periprosthetic humerus fractures, with the Wright and Cofield classification system being the most commonly used [7,11,14,15]. This system categorizes periprosthetic fractures into three types: type A (fracture located near the tip of the humeral stem that extends proximally), type B (fracture located near the tip of the humeral stem that extends distally), and type C (fracture located distal to the humeral stem) [11]. However, the fracture in this case did not fit these categories, as it was transverse and located in the proximal third of the diaphysis. Under the less commonly used Worland classification system, this fracture would be classified as a Worland type B2 fracture, characterized by a transverse break around the stem [15]. Alternatively, it could be classified as a Groh type I fracture [16], occurring proximal to the prosthesis tip, or a Campbell region 3 fracture [7], indicating its location in the proximal diaphysis. Although numerous cases of humeral stem failure in anatomic, reverse, and hemi shoulder arthroplasty prostheses have been reported [17,18], none has involved a retained, bent prosthetic stem. Metal implant deformation has been documented in trauma literature but has been observed only in long bones and not in joint replacements, such as those for the shoulder, elbow, hip, or knee. Willems and Greeven [19] reported a case of a bent humeral nail, but its composition and design differed substantially from a solid titanium shoulder arthroplasty stem. Determining the optimal treatment strategy for a periprosthetic humerus fracture remains a clinical challenge, and strategies can vary widely depending on the fracture pattern and patient characteristics. Tansey et al. [17] conducted a meta-analysis of 20 studies constituting 196 postoperative periprosthetic humerus fractures. Of these, 167 (85%) fractures were treated operatively with open reduction and internal fixation or revision arthroplasty, whereas only 26 (13%) were treated nonoperatively. Worland et al. [15] reported that, among patients treated nonoperatively, the healing rates were 63%, 43%, and 80% in Wright and Cofield A (n = 8), B (n = 14), and C (n = 4) fractures, respectively. Although limited by a small sample size, the authors found that a substantially higher rate of malunion was found to be associated with nonoperative compared with operative treatment (19% vs. 1%). However, there were no differences in non-union rates between operative and nonoperative treatments [15]. A systematic review by Otworowski et al. [20] suggests that stem instability is one of the most important factors influencing the treatment of periprosthetic fractures, with unstable fractures requiring revision arthroplasty. In the present case, we attributed the success of nonoperative treatment to the maintained stability of the humeral stem and the position of the fracture pattern well above the distal stem. Nonoperative management was chosen in the present case because of the apparent stability of the humeral stem, the location of the fracture, and the apparent integrity of the humeral stem. A limitation of the case report was not having a direct comparison between operative and nonoperative management for this extremely rare case. Also, the fracture’s inability to be classified under existing classification systems limits the generalizability of the report. Stem bending has never been evaluated biomechanically, and the lack of advanced imaging restricted the accurate characterization of bone quality, fracture extent, and prosthetic integrity. This was an isolated case in an elderly patient with a stable fracture pattern. However, it is possible that a younger, more active individual would have required a different treatment, such as operative intervention. Functional outcomes were evaluated qualitatively, without validated scoring systems, but follow-up radiographs
demonstrated complete healing of the fracture without CT scanning, which would have exposed the patient to unnecessary radiation. Follow-up was limited to 52 weeks, so late complications remain unknown.
The present case demonstrated an uncommon transverse periprosthetic humerus fracture and deformation of the humeral stem following RTSA. Despite delayed healing of the fracture, nonoperative treatment resulted in a satisfactory outcome. The case underscores the importance of an individualized treatment plan when addressing periprosthetic fractures accompanied by deformation of the humeral stem.
In select patients with a stable implant and minimal symptoms, non-operative treatment of a periprosthetic fracture, even in the setting of stem deformation, can result in successful healing and functional recovery.
References
- 1. Hachicha H, Chaker M, 1. Palsis JA, Simpson KN, Matthews JH, Traven S, Eichinger JK, Friedman RJ. Current trends in the use of shoulder arthroplasty in the United States. Orthopedics 2018;41:e416-23. [Google Scholar] [PubMed]
- 2. Mizuno N, Denard PJ, Raiss P, Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am 2013;95:1297-304. [Google Scholar] [PubMed]
- 3. Rugg CM, Coughlan MJ, Lansdown DA. Reverse total shoulder arthroplasty: Biomechanics and indications. Curr Rev Musculoskelet Med 2019;12:542-53. [Google Scholar] [PubMed]
- 4. Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2011;19:439-49. [Google Scholar] [PubMed]
- 5. Shah SS, Gaal BT, Roche AM, Namdari S, Grawe BM, Lawler M, et al. The modern reverse shoulder arthroplasty and an updated systematic review for each complication: Part I. JSES Int 2020;4:929-43. [Google Scholar] [PubMed]
- 6. Shah SS, Roche AM, Sullivan SW, Gaal BT, Dalton S, Sharma A, et al. The modern reverse shoulder arthroplasty and an updated systematic review for each complication: Part II. JSES Int 2021;5:121-37. [Google Scholar] [PubMed]
- 7. Campbell JT, Moore RS, Iannotti JP, Norris TR, Williams GR. Periprosthetic humeral fractures: Mechanisms of fracture and treatment options. J Shoulder Elbow Surg 1998;7:406-13. [Google Scholar] [PubMed]
- 8. Novi M, Porcellini G, Donà A, Tarallo L, Micheloni G, Giorgini A, et al. A long-term follow-up of post-operative periprosthetic humeral fracture in shoulder arthroplasty. Geriatr Orthop Surg Rehabil 2021;12. doi:10.1177/21514593211039908. [Google Scholar] [PubMed] [CrossRef]
- 9. Kobayashi EF, Namdari S, Schenker M, Athwal GS, Ahn J. Evaluation and treatment of postoperative periprosthetic humeral fragility fractures. OTA Int 2023;6:e244. [Google Scholar] [PubMed]
- 10. Singh JA, Sperling J, Schleck C, Harmsen W, Cofield R. Periprosthetic fractures associated with primary total shoulder arthroplasty and primary humeral head replacement: A thirty-three-year study. J Bone Joint Surg Am 2012;94:1777-85. [Google Scholar] [PubMed]
- 11. Wright TW, Cofield RH. Humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 1995;77:1340-6. [Google Scholar] [PubMed]
- 12. Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57. [Google Scholar] [PubMed]
- 13. Best MJ, Aziz KT, Wilckens JH, McFarland EG, Srikumaran U. Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2021;30:1159-66. [Google Scholar] [PubMed]
- 14. Groh GI, Groh GM. Complications rates, reoperation rates, and the learning curve in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:388-94. [Google Scholar] [PubMed]
- 15. Worland RL, Kim DY, Arredondo J. Periprosthetic humeral fractures: Management and classification. J Shoulder Elbow Surg 1999;8:590-4. [Google Scholar] [PubMed]
- 16. Groh GI, Heckman MM, Wirth MA, Curtis RJ, Rockwood CA. Treatment of fractures adjacent to humeral prostheses. J Shoulder Elbow Surg 2008;17:85-9. [Google Scholar] [PubMed]
- 17. Tansey PJ, Yetter TR, Somerson JS. Operative and nonoperative treatment of periprosthetic humerus fractures after shoulder arthroplasty: A systematic review and meta-analysis. J Shoulder Elbow Surg 2024;33:e629-36. [Google Scholar] [PubMed]
- 18. Zuckerman JD, Shapiro JA, Moghtaderi S, Kummer FJ. Fatigue failure of a shoulder hemiarthroplasty stem: A case report. J Shoulder Elbow Surg 2003;12:635-6. [Google Scholar] [PubMed]
- 19. Willems SA, Greeven AP. Humeral intramedullary nail bending following trauma: A case report. J Trauma Inj 2023;36:65-9. [Google Scholar] [PubMed]
- 20. Otworowski M, Grzelecki D, Starszak K, Boszczyk A, Piorunek M, Kordasiewicz B. Periprosthetic fractures after shoulder arthroplasty: A systematic review. EFORT Open Rev 2023;8:748-58. [Google Scholar] [PubMed]