Humeral shaft fractures in late pregnancy are rare and require a staged, multidisciplinary approach to balance maternal recovery with fetal safety.
Dr. Amandeep Bains, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd Phase, M.I.A. 1st Phase, Basni, Jodhpur - 342005, Rajasthan, India. E-mail: bains0679@gmail.com
Introduction: Orthopedic trauma complicates 6–7% of pregnancies and remains a leading cause of non-obstetric maternal and fetal morbidity. While musculoskeletal injuries during pregnancy are not uncommon, fractures requiring surgical intervention in the third trimester are rare and present unique management challenges. Among these, humeral shaft fractures are especially rare, and their management must carefully balance maternal recovery with fetal well-being.
Case Report: We report the case of a 30-year-old primigravida at 38 + 4 weeks of gestation who sustained a left diaphyseal humerus fracture following a motor vehicle collision. Initial management included closed reduction and immobilization in a U-arm slab. Due to signs of fetal distress on cardiotocography and Doppler ultrasound – suggestive of intrauterine hypoxia – an emergency lower segment cesarean section was performed under spinal anesthesia. Four days postpartum, the patient underwent successful open reduction and internal fixation of the humerus using an extra-articular distal humerus plate and lag screws. A combined general anesthesia and supraclavicular brachial plexus block provided effective perioperative pain management. Post-operative recovery was uneventful, with early mobilization and favorable maternal and neonatal outcomes.
Conclusion: This case underscores the importance of a multidisciplinary, staged approach to orthopedic trauma in late pregnancy. Prioritizing timely obstetric intervention followed by delayed fracture fixation allows safe maternal recovery while safeguarding fetal health.
Keywords: Pregnancy, humerus shaft fracture, cesarean delivery, trauma, multidisciplinary care.
Trauma complicates roughly 6–7% of pregnancies and remains a leading non-obstetric cause of maternal and fetal morbidity [1]. Bone fracture management in third-trimester pregnant patients is rare and poorly discussed in the literature [2]. When they do occur, they require a carefully balanced approach that prioritizes both maternal recovery and fetal safety. Among them, humeral shaft fractures are especially rare in late gestation. Management must consider gestational age, type of fracture, anesthesia implications, and perinatal outcomes [3,4]. We report a case involving a 30-year-old primigravida at 38 + 4 weeks of gestation, who sustained a diaphyseal fracture of the humerus following an associated history of a road traffic accident (four-wheeler vs. four-wheeler). The injury was managed through a two-step protocol involving conservative immobilization with a U-arm slab followed by an emergency lower segment cesarean section (LSCS) and subsequent surgical fixation. This report discusses diagnostic, surgical, anesthetic, and perioperative considerations and offers a proposed management pathway for similar cases.
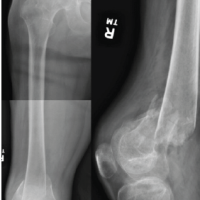
A 30-year-old primigravida at 38 weeks +4 days of gestation presented to the emergency department after a road traffic accident involving a four-wheeler collision. She reported pain and deformity in the left upper limb. The patient had no prior medical comorbidities, and her pregnancy had progressed uneventfully following spontaneous conception. She had adhered to routine antenatal care, including regular intake of iron and calcium supplements, two doses of tetanus vaccination, and standard antenatal screening. She was blood group O-positive and tested negative for Group B Streptococcus. Her menstrual history was unremarkable, with regular cycles occurring every 28–30 days, lasting 3–4 days with average flow. On presentation, the patient was alert, oriented, and hemodynamically stable (blood pressure 100/70 mmHg, heart rate [HR] 98 bpm, RR 18/min, and SpO2 99% on room air via left upper limb). She was afebrile, with no pallor or pedal edema. There was no history of loss of consciousness, ear, nose, throat bleeding, vomiting, or seizures. Local examination of the left upper limb revealed tenderness, swelling, and deformity without any open wounds. Motor and sensory functions were preserved, and radial and ulnar pulses were palpable. Abdominal examination revealed a uterine fundal height consistent with 36 weeks, a longitudinal lie, cephalic presentation, and a tense, rigid uterus. Irregular uterine contractions (2–3/10 min) were noted, along with reduced fetal movements. Cardiotocography (CTG) showed a baseline fetal HR of 175 bpm, with recurrent late decelerations and reduced beat-to-beat variability (<5 bpm). Doppler studies revealed increased umbilical artery resistance (pulsatility index [PI]: 1.48; S/D ratio: 4.2) and a decreased middle cerebral artery PI (PI: 0.82), resulting in a cerebroplacental ratio of 0.55 – indicative of a brain-sparing effect and consistent with intrauterine hypoxia. A non-stress ultrasound showed normal amniotic fluid volume and a singleton fetus in cephalic presentation with no placental or uterine abnormalities. The cervix was 2 cm dilated but closed. Routine laboratory investigations, including complete blood count, coagulation profile, and crossmatch, were within normal limits. Given the gestational age and maternal stability, a trauma protocol was activated involving obstetrics, orthopedics, anesthesiology, and neonatology teams. Plain radiographs of the right arm (with pelvic shielding) revealed a wedge-type diaphyseal fracture of the humerus (AO type 12B2). Closed reduction under traction was performed, and immobilization was achieved with an upper arm (U) slab(Figure 1). Given signs of fetal compromise – possibly due to placental abruption – the multidisciplinary team recommended conservative orthopedic management until delivery.

Figure 1: Pre-operative radiographs of left arm anteroposterior (a) and lateral (b) view showing a displaced distal 1/3rd shaft humerus fracture (AO type 12B2) with overriding fragments, and clinical images (c and d) showing limb immobilization in a U-slab in a third-trimester pregnant patient.
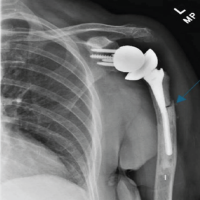
Following American College of Obstetricians and Gynecologists (ACOG) recommendations for fetal monitoring in viable pregnancies requiring surgery, continuous CTG surveillance was carried out. As fetal distress was evident on Doppler and non-stress tests, definitive orthopedic intervention was deferred. Conservative immobilization was maintained with analgesia using paracetamol. However, humeral fractures do not interfere with the mechanics of vaginal delivery, as is often the case with unstable pelvic fractures [5]. The presence of fetal distress in this patient necessitated an emergency cesarean section. At 38 + 4 weeks of gestation, an emergency LSCS was performed under spinal anesthesia. Intraoperatively, the lower uterine segment was well-formed. Amniotic fluid was blood-stained but adequate. The placenta was removed completely with intact membranes. Bilateral fallopian tubes and ovaries appeared normal. The uterus was closed in two layers with hemostasis achieved. Estimated blood loss was 500 mL. A healthy neonate weighing 3005 g was delivered without complications. A neonatal team was on standby, in accordance with standard care for non-obstetric surgery during viable pregnancies [6]. CTG monitoring during and after the procedure remained reassuring. A Kleihauer–Betke test was performed to assess the risk of fetomaternal hemorrhage as per trauma protocol [7]. On post-operative day 4, the patient underwent open reduction and internal fixation (ORIF) of the right humerus using an 8-hole extra-articular distal humerus locking plate with two lag screws. A standard anterolateral approach was used. The fracture site was visualized, and anatomical reduction was achieved without neurovascular compromise. General anesthesia was induced with propofol and fentanyl. In addition, an ultrasound-guided right supraclavicular brachial plexus block with ropivacaine was administered to optimize post-operative pain relief [8]. This combined anesthetic strategy was chosen to minimize intraoperative and post-operative opioid use, particularly to reduce neonatal drug exposure during lactation [9].
The patient had an uneventful post-operative recovery. Early mobilization of the shoulder and elbow was initiated within 36 h (Figure 2).
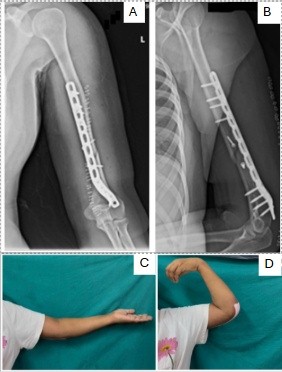
Figure 2: Post-operative radiographs of the left humerus following open reduction and internal fixation, anteroposterior (a) and lateral views (b) showing fracture fixation with distal humerus extra-articular plate and two lag screw, and clinical images showing post-operative range of motion of left elbow extension (c) and flexion (d).
With fetal concerns resolved, the focus shifted to maternal recovery. Post-operative pain was effectively managed using multimodal analgesia, including scheduled paracetamol and a regional nerve block. Breastfeeding was successfully initiated, and sedation and opioid use were minimized to reduce the risk of neonatal respiratory depression [5]. Physiotherapy, including shoulder range-of-motion exercises, was started on post-operative day 2. Prophylactic anticoagulation was resumed 6 h after surgery, as post-operative bleeding remained minimal. By postpartum day 8, the mother and newborn were both stable. The surgical wound was clean, and the dressing was dry. At 6-week follow-up, early radiographic union was evident, and the patient had regained functional range of motion with only mild residual pain managed with non-opioid medications (Fig. 3).
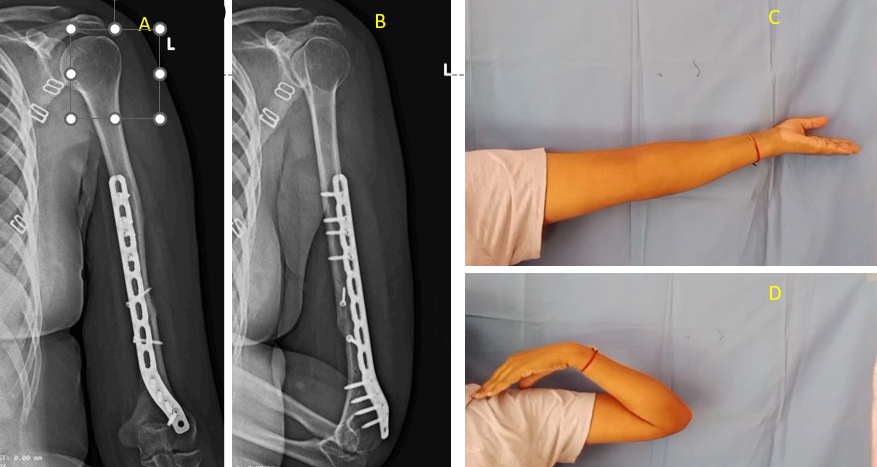
Figure 3: Post-operative radiographic and functional outcomes following open reduction and internal fixation of a humeral shaft fracture. (a) Anteroposterior radiograph and (b) lateral radiograph demonstrating satisfactory fracture union with plate osteosynthesis. (c) Clinical photograph showing complete elbow extension, and (d) complete elbow flexion at follow-up, indicating restoration of functional range of motion.
No complications – such as infection, thromboembolism, or neurovascular injury – were reported. The patient expressed satisfaction with the coordinated, multidisciplinary care and showed good recovery while attending to her newborn.
Protocol flowchart
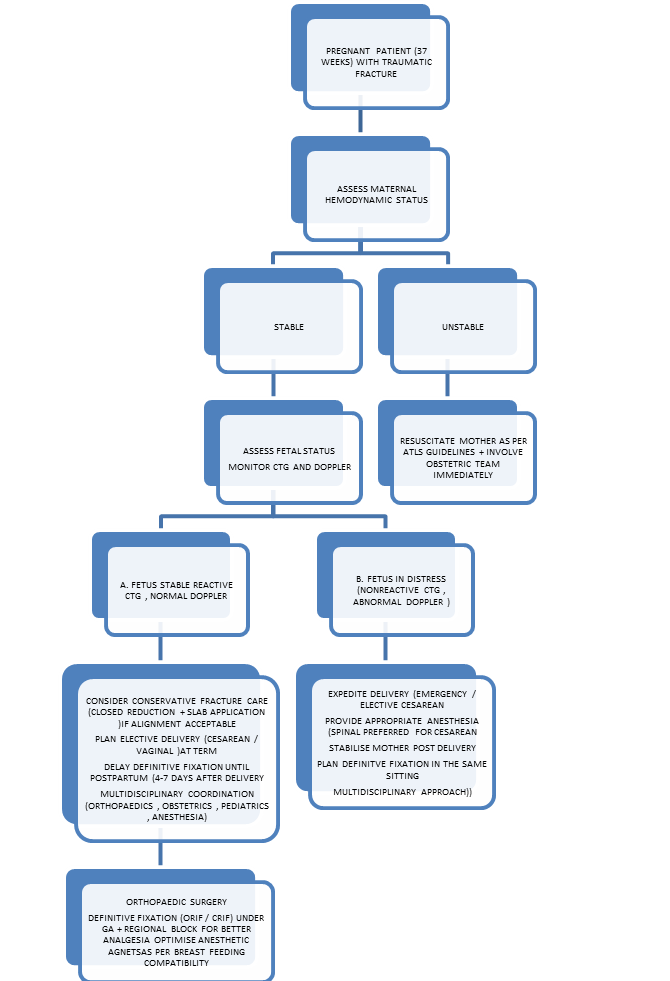
Orthopedic trauma during pregnancy presents complex clinical challenges due to the dual consideration of maternal and fetal outcomes. Although trauma affects 6–7% of pregnancies, fractures requiring surgical intervention in the third trimester are particularly rare . Our case of a diaphyseal humeral fracture at 38 + 4 weeks of gestation highlights a strategic, multidisciplinary approach – initial stabilization, emergent obstetric intervention, and delayed orthopedic fixation – leading to favorable outcomes for both mother and neonate. Trauma severity and gestational age are key factors in determining delivery timing and surgical approach. Mendez-Figueroa et al. and Aiello et al. emphasized that viable pregnancies beyond 34 weeks with non-reassuring fetal status benefit from prompt delivery followed by orthopedic care in a controlled postpartum setting [1,10]. Our approach – prioritizing fetal well-being with emergent cesarean delivery – was consistent with these principles. Multidisciplinary coordination is critical. Similar approaches reported by Purohit et al.and Bozkurt et al. show that staged cesarean delivery followed by definitive fixation is both safe and effective in cases with fetal distress [2,11]. Our case mirrors this strategy, emphasizing the need for structured protocols that align orthopedic timing with obstetric priorities [12]. Moreover, narrative reviews by Ali et al. and Choudhry et al. highlight the importance of institutional trauma pathways, early team communication, and individualized care plans in optimizing outcomes in pregnant trauma patients [4,13]. Timely obstetric evaluation is crucial, as trauma is a leading cause of non-obstetric fetal morbidity and mortality [3]. According to ACOG and Society of Obstetricians and Gynaecologists of Canada guidelines, maternal stabilization takes precedence, followed by fetal assessment if gestation exceeds 23 weeks [5]. In our case, fetal Doppler changes and CTG abnormalities necessitated urgent LSCS, which aligns with these recommendations. Imaging, though often underutilized due to fetal radiation concerns, is considered safe when pelvic shielding is used, especially in extremity injuries [13]. Delaying imaging may compromise orthopedic planning and should be avoided. Several guidelines confirm that radiologic evaluation, when appropriately conducted, carries minimal fetal risk and should not be deferred in trauma cases [3,10,13]. The third trimester presents unique anatomical and physiological challenges, including uterine enlargement, altered drug metabolism, and limited surgical positioning. These considerations informed our decision to delay ORIF by 4 days, allowing uterine involution, improved analgesia, and maternal hemodynamic recovery. Studies suggest this delay period (4–7 days postpartum) is optimal for orthopedic fixation [6,10]. While humeral shaft fractures are often amenable to conservative management with functional bracing or immobilization, certain clinical scenarios – including displaced, unstable fractures; associated neurovascular compromise; or the presence of polytrauma – warrant definitive surgical intervention. In pregnant patients, the decision is further influenced by gestational age and fetal condition. Conservative care may suffice when the fracture is stable and maternal-fetal status is reassuring, as demonstrated in some reported cases [14,15,16 ]. However, surgical fixation becomes essential when conservative measures cannot ensure stability, pain control, or functional recovery, particularly in the postpartum period when early mobilization is crucial for maternal caregiving and rehabilitation responsibilities. Thus, our staged approach balanced the temporary conservative stabilization during fetal compromise with the absolute need for definitive fixation postpartum. Anesthesia choice is pivotal. General anesthesia combined with a supraclavicular brachial plexus block, as used in our case, reduces perioperative opioid use – an important consideration in breastfeeding mothers [8,9,17,18]. In addition, regional blocks minimize systemic side effects and enhance early mobilization. Spinal anesthesia for cesarean delivery is associated with stable maternal hemodynamics and minimal neonatal drug exposure [19]. A review of previously reported upper extremity trauma cases in pregnancy reveals a spectrum of injuries ranging from clavicle, scapular, and humeral fractures to complex bilateral distal radius fractures. Management has varied based on gestational age, injury severity, and fetal condition. Most distal humerus and radius fractures were treated with postpartum ORIF [112021], whereas shaft and clavicular injuries often allowed for conservative treatment [14,15,16]. Notably, bilateral injuries and cases involving pregnancy-associated osteoporosis [22] presented unique challenges. Cases like that of Sharma et al. [16] and Abbas et al. [23] support staged surgical approaches, mirroring the protocol followed in our case (Table 1).
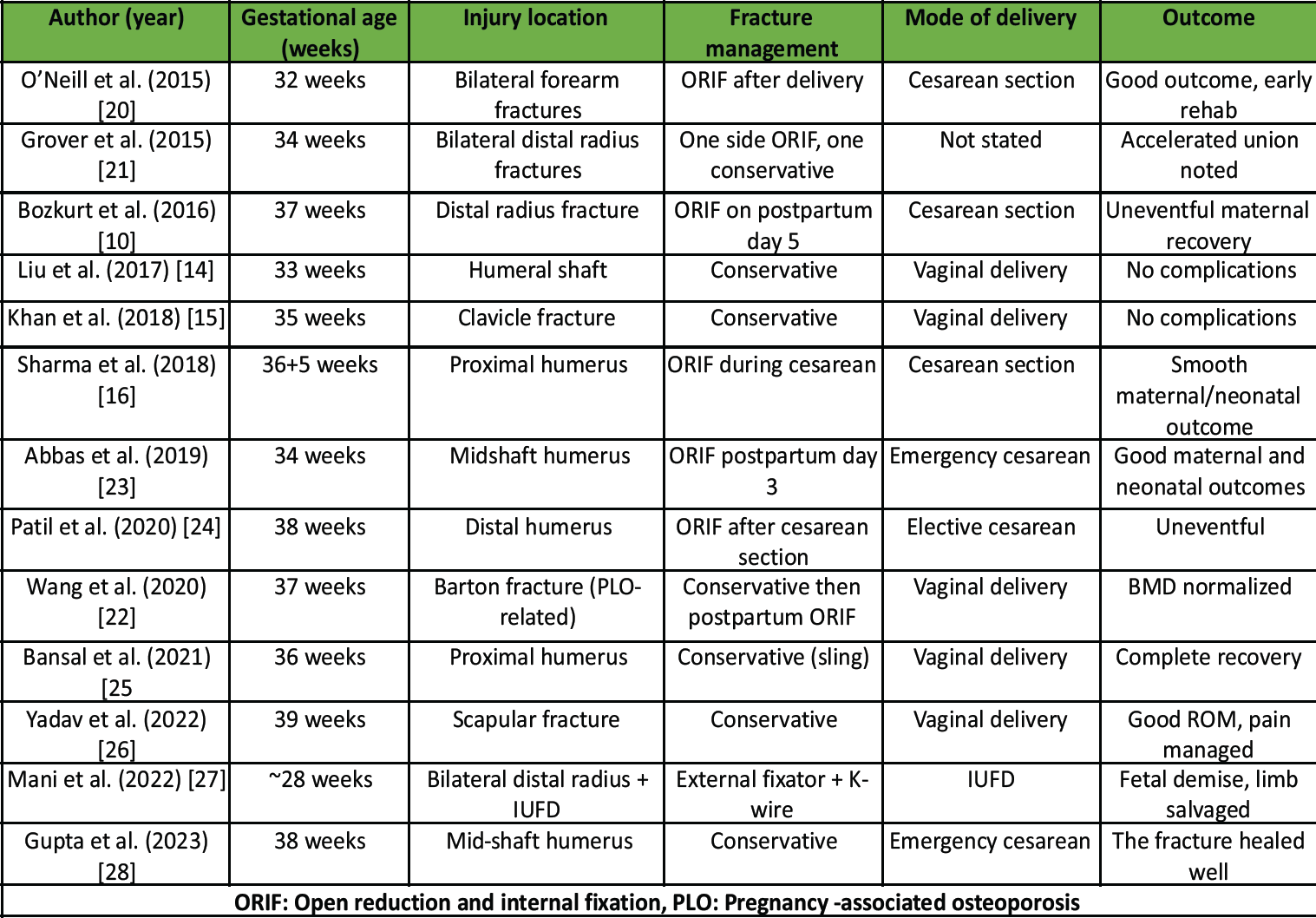
Table 1: Reported cases of upper extremity fractures in pregnant women
Orthopedic trauma in pregnancy requires careful balancing of maternal and fetal priorities. This case highlights that a staged approach – initial stabilization, timely cesarean delivery for fetal distress, and delayed definitive fixation of the humeral fracture – can achieve favorable outcomes. Multidisciplinary coordination between obstetric, orthopedic, anesthesiology, and neonatal teams is critical to ensure both maternal recovery and neonatal safety.
Humeral shaft fractures in late pregnancy are rare but can be safely managed using a staged strategy. Prioritizing fetal well-being with timely cesarean delivery, followed by delayed orthopedic fixation under multidisciplinary care, provides the best maternal and neonatal outcomes.
References
- 1. Mendez-Figueroa H, Dahlke JD, Vrees RA, Rouse DJ. Trauma in pregnancy: An updated systematic review. Am J Obstet Gynecol 2013;209:1-10. [Google Scholar] [PubMed]
- 2. Purohit S, Bhalodia P, Rathod P, Ranjan R, Vishal K. Management of bilateral lower limb fractures in a third-trimester gravida: Case report and review. J Med Sci Health 2016;2:47-50. [Google Scholar] [PubMed]
- 3. Petrone P, Jiménez Morillas P, Axelrad A, Marini CP. Traumatic injuries to the pregnant patient: A critical literature review. Eur J Trauma Emerg Surg 2019;45:383-92. [Google Scholar] [PubMed]
- 4. Choudhry MN, Ahmad Z, Verma R. Management of orthopaedic trauma in pregnancy: A review. J Orthop 2018;15:633-7. [Google Scholar] [PubMed]
- 5. American college of obstetricians and gynecologists. Committee opinion No. 775: nonobstetric surgery during pregnancy. Obstet Gynecol 2019;133:e285-6. [Google Scholar] [PubMed]
- 6. Morshed S, Miclau T 3rd, Bembom O, Cohen M, Knudson MM, Colford JM Jr. Delayed internal fixation of femoral shaft fracture reduces mortality among patients with multisystem trauma. J Bone Joint Surg Am 2009;91:3-13. [Google Scholar] [PubMed]
- 7. Weinstein L. The Kleihauer-Betke test: Clinical indications and technical considerations. Obstet Gynecol Clin North Am 1991;18:285-302. [Google Scholar] [PubMed]
- 8. Choi S, McCartney CJ. Evidence for the use of peripheral nerve blocks for postoperative pain relief. Curr Opin Anaesthesiol 2016;29:592-7. [Google Scholar] [PubMed]
- 9. Kang R, Jeong JS, Yoo JC, Lee JH, Park BY. The effect of supraclavicular nerve block combined with general anesthesia on postoperative analgesia and opioid consumption in shoulder surgery: A randomized controlled trial. PLoS One 2015;10:e0137312. [Google Scholar] [PubMed]
- 10. Aiello VD, Mastrocola LE, Savoini M, Andreacchio A. Management of orthopaedic injuries in pregnant patients: A review of current practice. J Orthop Traumatol 2018;19:12. [Google Scholar] [PubMed]
- 11. Bozkurt M, Tokgozoglu AM, Ozdemir H, Cicek E, Bulut T, Turanli S. Distal radius fracture in late pregnancy. Orthop Traumatol Surg Res. 2016;102(6):829-31. [Google Scholar] [PubMed]
- 12. Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am 2006;88:2343-7. [Google Scholar] [PubMed]
- 13. Ali U, Rauf S, Ahmed R, Ahmad M. Orthopedic trauma in pregnancy: A narrative review. Pak J Med Sci 2022;38:690-4. [Google Scholar] [PubMed]
- 14. Liu H, Zhang Z, Wang Y, Li Y, Chen W, Wu Z. Humeral fracture in third trimester: a case report. Chin J Traumatol. 2017;20(3):176-8. [Google Scholar] [PubMed]
- 15. Khan N, Sharma A, Choudhury A, Gupta R, Meena S, Kumar V. Clavicle fracture in pregnancy: a conservative success. BMJ Case Rep. 2018;2018:bcr2018224953. [Google Scholar] [PubMed]
- 16. Sharma R, Singh V, Gupta N, Sharma A. Proximal humerus fracture during cesarean: a case report. Int J Reprod Contracept Obstet Gynecol. 2018;7(12):5047-9. [Google Scholar] [PubMed]
- 17. Cobb B, Liu R, Valentine E, Onuoha O. Breastfeeding after anesthesia: A review for anesthesia providers regarding the transfer of medications into breast milk. Anesth Analg 2015;120:100-10. [Google Scholar] [PubMed]
- 18. Bae K, Kim YJ, Lim HW, Kang MS, Kim HJ, Koh WU, et al. Evaluating the clinical utility of brachial plexus block for reducing opioid exposure in pediatric elbow fracture surgery: A retrospective cohort study. Medicina (Kaunas) 2024;60:483. [Google Scholar] [PubMed]
- 19. Santos AC, Pedersen H, Finster M. Spinal anesthesia for cesarean section: Maternal hemodynamic and neonatal effects. Anesth Analg 1984;63:665-70. [Google Scholar] [PubMed]
- 20. O’Neill CJ, Kiely P, Condon F, Quinlan W. Bilateral forearm fractures in a pregnant patient: a case report. J Orthop Case Rep. 2015;5(3):43-5. [Google Scholar] [PubMed]
- 21. Ravikumar TV, Rahul P, Grover A, Samorekar B. Bilateral distal radius fracture in third trimester of pregnancy with accelerated union: a rare case report. J Clin Diagn Res. 2015;9(4):RD01-RD02. [Google Scholar] [PubMed]
- 22. Wang G, Bai X. Barton fracture of the distal radius in pregnancy and lactation-associated osteoporosis: a case report and literature review. Case Rep Womens Health. 2020;27:e00208. [Google Scholar] [PubMed]
- 23. Abbas M, Sahu RL, Ranjan R, Kumar A, Meena S, Gupta A. Midshaft humerus fracture and LSCS: a case report. J Clin Orthop Trauma. 2019;10(3):590-3. [Google Scholar] [PubMed]
- 24. Patil S, Kulkarni V, Desai S, Bhosale P. Delayed distal humerus fixation post LSCS. J Obstet Trauma Surg. 2020;2(1):17-21. [Google Scholar] [PubMed]
- 25. Bansal S, Meena S, Agarwal A, Kumar V. Conservative treatment of proximal humerus fracture in late pregnancy: a case report. Int J Orthop Sci. 2021;7(2):347-9. [Google Scholar] [PubMed]
- 26. Yadav V, Gupta R, Kumar S. Scapular fracture in term pregnancy: a rare case. J Obstet Emerg Med. 2022;12(2):91-3. [Google Scholar] [PubMed]
- 27. Mani KCK, Yadav S, Panigrahi R, Acharya D. Bilateral distal radius fractures with seven-month pregnancy during COVID-19 lockdown in Nepal: a case report. Trauma Int. 2022;8(1):29-32. [Google Scholar] [PubMed]
- 28. Gupta R, Meena S, Sharma A, Kumar V. Humeral fracture in pregnancy: conservative post LSCS management. J Orthop Case Rep. 2023;13(2):45-7. [Google Scholar] [PubMed]