Intramedullary nailing in extra-articular proximal tibial fractures facilitates shorter hospital stay, faster fracture union, and earlier full weight bearing, while maintaining comparable complication rates and functional outcomes to minimally invasive proximal plating.
Dr. Ahmed Sajid, Department of General Medicine, Pakistan Institute of Medical Sciences, Islamabad, Pakistan. Email: sandhilah.ahmad@gmail.com
Background: Extra-articular fractures of the proximal tibia are extremely difficult to treat. These fractures can be treated with intramedullary nailing (IMN), closed reduction, and minimally invasive plating.
Objective: The objective of this study was to compare the efficacy of proximal plating versus IMN in the treatment of extra-articular proximal tibial fractures.
Materials and Methods: The present randomized prospective clinical study was carried out at the department of orthopedics, Isra University Hospital, Hyderabad, from May 2024 to December 2024 on 62 individuals with fracture of the proximal tibia who underwent proximal tibial plating (PTP) or IMN after taking permission from the ethical board of the institute. Computer-assisted prospective randomization was used to assign participants to groups. Participants in Group A received IMN treatment, whereas those in Group B received PTP. Data were analyzed through the Statistical Package for the Social Sciences version 24. The significance threshold that was used was P < 0.05. Age, sex, hospitalization, infection rate, fracture union duration, and fracture angulation were all compared between the two groups. The interval data (age, operative time, fracture union time, and knee movement) were subjected to a paired-sample t-test.
Results: A total of 48 cases were studied, which were divided into two groups. Significantly shorter stay at hospital after surgery (value of P = 0.035), time for union, and time to full bearing of weight (P = 0.004) were experienced by the IMN group as compared to Group B. However, neither technique clearly outperformed the other groups with regard to operative time (P = 0.082), rate of infection (P = 0.738), knee range of motion (P = 0.462), or degrees of malunion or non-union.
Conclusion: The current study concluded that there was no noteworthy difference between the two techniques in relation to surgical duration, rate of infection, and frequency of malunion and non-union. However, IMN is better than minimally invasive plating in terms of the duration of hospital stay, speed of union, and early full weight bearing.
Keywords: Proximal plating, intramedullary nailing, extra-articular proximal tibial fracture.
About 5–10% of the total tibial fractures are extra-articular fractures of the proximal tibia, which are commonly caused by trauma at high velocities. They result in complicated tissue damage that affects the bone and soft tissues around it, including fracture blister and compartment syndrome [1]. Conservatively treating these fractures with casts results in prolonged immobilization of the knee and ankle, which frequently causes non-union, rotational deformity, or stiffness of the surrounding joints, all of which lower the patients’ quality of life. Therefore, surgery is usually necessary as the final treatment for these fractures. These fractures are still among the most controversial ones, and the management of them is still up for debate among surgeons. Intramedullary (IM) nails, half-pin external fixations, hybrid external fixations, plate fixations, or a combination of these surgical procedures are among the several approaches adopted [2]. In recent times, lower limb fractures, particularly proximal and distal tibial fractures, have successfully been treated using closed reduction combined with minimally invasive plating and IM nailing (IMN) [3,4]. To treat proximal tibia fractures, the surgical objective should be to minimize soft-tissue problems while restoring the knee’s alignment, rotation, length, articular margin, and knee motion. The gold standard for treating tibial shaft fractures is IMN of proximal tibia fractures. In the treatment of proximal tibia fractures, it is recognized as a difficult procedure. The metaphyseal hypertrophy and extended lever arm make nailing and fracture reduction technically challenging operations [5,6]. As a result, some writers support the treatment of proximal tibia fractures using plate osteosynthesis [7,8]. The main objective of this study was to compare the outcomes of minimally invasive plating and tibial nailing, particularly focusing on union time, infection, and weight-bearing ability, in line with recent comparative series which show advantage for IMN in union time and lower infection [4,6].
The present randomized prospective clinical study was carried out at the Department of Orthopedics, Isra University Hospital, Hyderabad, from May 2024 to December 2024 on 62 individuals with fracture of the proximal tibia who underwent proximal tibial plating (PTP) or IMN after taking permission from the ethical board of the institute. Fourteen individuals who were lost to follow-up were excluded, and 48 individuals were enrolled in the final results investigation. This study included participants who were skeletally mature and had closed proximal tibial metaphyseal fractures. The proximal tibia is defined as the region between the articular surface and 1.5 times its medial to lateral breadth [1]. Individuals with pathological fractures, injuries in the same/opposite lower limb, tibial shaft fractures, or meta-diaphyseal fractures of the tibia with an intra-articular extension were excluded. Computer-assisted prospective randomization was used to assign participants to groups using opaque envelopes with sequential numbers. A nurse who was oblivious to the allocation opened envelopes within the surgery room. Participants in Group A received IMN treatment, whereas those in Group B received PTP. To do IMN in Group A, an entry site was created immediately medial toward the lateral intercondylar apex of the tibial plateau using a medial parapatellar method. A reduction unicortical plate, momentary blocking screws, a reduction clamp, or a universal fixator have been utilized for reduction, with the exception of the reduction unicortical plate employed in combination with a reamed IM tibial nail. After the fracture was repaired, these devices were taken out. The IM nail had four multilevel, multiplanar, and multidirectional screws in addition to a proximal Herzog band. Participants in Group B received treatment through a curvilinear incision across the lateral portion of the proximal tibia utilizing minimally invasive PTP. Axial traction or the use of a reduction clamp or distractor was used to accomplish indirect reduction. After that, a locking compression plate was used to establish internal fixation. The fracture was plated employing a minimally invasive method, and at least three screws were inserted on each side. Following surgery, individuals in both groups received 3 days of intravenous third-generation cephalosporin antibiotics. Activities were started on the 1st day after surgery to strengthen the ankle pumps and isometric quadriceps. On the 2nd day after surgery, active and aided knee bending was performed. Depending on the construct’s stability, partial weight-bearing was permitted as early as the second post-operative day; however, full weight-bearing was only permitted upon full clinical and radiological union. At 2 and 6 weeks, 3 and 6 months, and 1 year after surgery, all patients were monitored. To evaluate the precision of reduction and ultimate alignment, radiographs taken immediately after surgery and at the end of the follow-up period were compared. Measurements were made for sagittal (procurvatum and recurvatum) and coronal (varus and valgus) plane abnormalities by employing the method outlined by Freedman and Johnson. By calculating the angle among the lines drawn at 90° to the proximal and distal tibial articular surfaces in anterior-posterior view, varus/valgus malformation was assessed. The procurvatum/recurvatum was measured identically in lateral view, and the posterior slope was taken. A malformation of any plane was referred to as malreduction. Clinical evaluations of rotating arrangement, suet, and knee range of motion were conducted. If three or more cortices were unremitting on two radiographic pictures, the fracture was deemed unified. Three consecutive months of X-rays were considered to be non-union if they did not show significant recovery. Data were analyzed through the Statistical Package for the Social Sciences version 24. The significance threshold that was used was P < 0.05. Age, gender, hospitalization, rate of infections, time for union of fracture, and motion range of the knee were all compared between the two groups. The groups were compared in terms of the parameters. The interval data (surgery duration, age, duration in hospital, fracture union time, and motion of the knee) were subjected to a t-test.
Of the 62 participants in the study, 12 (six in the plating and six in the IMN group) failed to appear for follow-up, and, hence, 48 cases were analyzed. Both groups had similar pre-operative features, such as age, gender, classification, injury type, and duration between injury and surgical procedure, as presented in Table 1. The IM nailing (IMN) group experienced a considerably shorter post-operative stay in the hospital, time to full weight bearing, and duration of union than the PTP group, as presented in Table 1. Three of the participants in the PTP group experienced infections at the surgery site; two of them were treated with debridement, and the third required implant removal because of infection. Three of the participants in the IMN group experienced delayed union, for which the distal screw was removed during dynamization. Two of the nailing group’s patients developed non-union, requiring fibular osteotomy and replacement of nailing with bone grafting. Two of the participants in the proximal plating category experienced non-union; in this instance, bone grafting was performed, ultimately resulting in fracture repair. In the X-rays taken immediately after surgery and 1 year later, the tibia’s alignment as determined by an independent observer did not significantly differ, indicating that no further loss of reduction occurred. The results showed no statistically significant variance between the groups (P = 0.296), but the mean post-operative coronal plane angulation was 2.7~ (range zero to seven) in the IMN group, and in the PTP group, it was 2.1~ (range zero to eight). A tendency toward varus is present in both of these. The IMN and PTP groups had mean levels of post-operative in the sagittal plane of 2.6~ (range 0–8}, SD = 1.82) and 2.2~ (range 0–9}, SD = 1.98), respectively. Both groups have a tendency toward procurvatum; however, there was no noteworthy variance between them (P = 0.415). There were five individuals (22.7%) with malalignment in the IMM group (two participants had varus and three had anterior apex defect) and six individuals (15%) in the PTP group (three participants had procurvatum, and three had varus). P = 0.46 indicates that the average range of motion for groups A and B was 119.7~ (with a range 90–150, SD were 19.18) and 115.2~ (with a range 80–150, SD was 17.28). Eight of the participants (33.6%) in A and two individuals (9%) in B group complained of infrequent pain in the anterior knee and when kneeling on the floor (P = 0.097).
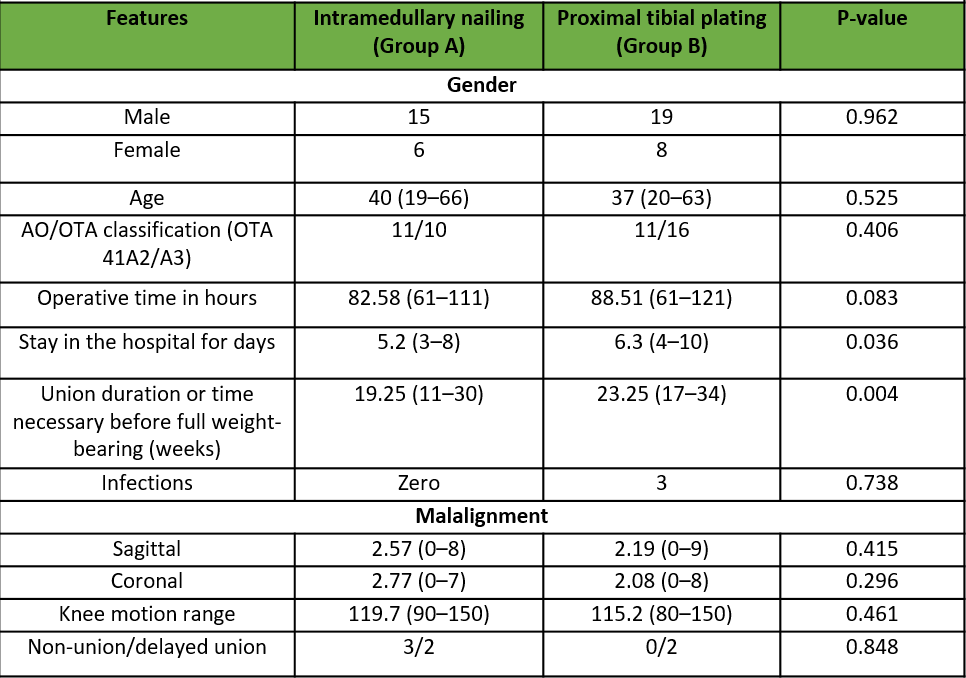
Table 1: Comparison of the post-operative and demographic details for the two groups
There are few studies that compare minimally invasive plating and tibial nail treatment for extra-articular proximal tibial fractures. The main objective of this study was to compare the outcomes of minimally invasive plating and tibial nailing from a number of angles. As a result of the smaller cut created during nailing, individuals in the IMN group in this study had a considerably shorter hospitalization compared to individuals in the PTP group (P < 0.05). This shows that IMN causes less of a financial burden as well as lowers medical expenses for humanity. These findings are consistent with Monahan et al., 2024, who reported shorter hospital stays using IMN compared to plating in extra-articular proximal tibia fractures [4]. There is no specific time window at which full bearing weight should begin with either therapy, even though early weight-bearing naturally comes with a load-sharing technique such as an IMN. Several readings have consistently concluded that it should begin as soon as the individual is able to tolerate it [1]. A surgeon’s preference, the pattern, and the location, complete weight-bearing was started at different intervals between 0 and 16 weeks in earlier trials of extra-articular proximal tibial fractures treated with IMN [6,7]. Likewise, for the same reasons, the period to complete weight-bearing following PLP treatment for extra-articular proximal tibial fractures has varied from 6 to 13 weeks [1,10]. In our study, the IMN group needed 19.25 weeks less than the PTP group to reach complete weight-bearing, which was only accomplished with the whole radiological union (23.25 weeks). Even though these periods are longer than those reported in other studies, we did not begin full weight-bearing until after the fractures had fully healed clinically and visually. In light of this, we began using supported motions, both passive and active, on day two and then moved on to partial weight-bearing. Thus, there were no appreciable variations in the groups’ knee range of motion. Studies such as Prabhat et al., 2025 also emphasize earlier union time with expert interlocking IM nails versus plate fixation [6]. Infection rates in nailing patients are reported to vary from 0% to 8% [6,7]. However, the study done by Lindvall et al. found noticeably greater infection rates: 28% in the nailing group versus 24% in the group that used plating. The greater percentage (42%) of individuals with fractures that were open in their study is most likely the cause of this [1]. The rate of infections was 2.5% in the nailing group and 14% in the plating group, according to the systematic review by Bhandari et al. In our series, the IMN group had an infection rate of 6%, whereas the PTP group had an infection rate of 9% (P = 0.738) [2]. Recent meta-analyses (Monahan et al., 2024) show that IMN is associated with a significantly lower superficial infection risk compared to locking plating techniques (RR ~0.65, p = 0.028) in closed extra-articular proximal tibial fractures [4]. A known consequence of nailing proximal tibia fractures is malunion, which has been found to happen in 3–100% of instances in previous studies [8,9]. In our study, three of the participants in the IMN group experienced delayed union, for which the distal screw was removed during dynamization. Two of the nailing group’s patients developed non-union, requiring fibular osteotomy and replacement of nailing with bone grafting. Two of the participants in the PTP category experienced non-union in this instance; bone grafting was performed, ultimately resulting in fracture repair. In the X-rays taken immediately after surgery and 1 year later, the tibia’s alignment as determined by an independent observer did not significantly differ between the groups, suggesting that there was no subsequent loss of reduction. Bhandari et al. conducted a systematic evaluation of 17 papers and found that the nailing group had a greater malunion rate (20%) compared to the plating group (10%) [2]. Apex anterior mal-reduction happened in 36% of the individuals in the IMN group and 15% of participants in the plating group, according to Lindvall et al., who also noted a greater malunion incidence in the nailing group, but this difference was not statistically significant [1]. Our study’s analysis of union rates following the first fixation revealed that the PTP group had a 97% union rate (P = 0.849) while the IMN group had a 95% union rate. Our series’ high union rates are in line with those reported in other published publications, which vary from 91% to 100% [1,11,12]. Our findings, however, were superior to those of a research conducted by Lindvall et al., in which the authors reported that the PTP group had a 94% union rate and the IMN group had a 77% union level. We think that the reason for this discrepancy in union rates was not the surgery type, but rather the exclusion of open fractures from our sample. The locking nail method shows advantages when considering the duration of the surgical procedure, hospitalization, early full bearing of weight, and time for union of bone [1]. In terms of short hospital stays, faster union times, and prompt full bearing of weight, we found that the nailing procedure is superior to the plating approach. However, neither technique clearly outperformed the other when taking about operation duration, rate of infection, or rates of malunion and non-union. Both implants offered stiff fixation that avoided subsequent fracture collapse and showed encouraging outcomes with extra-articular proximal tibial fractures [11,13,14].
Limitations
This study has several limitations. The sample size was small (48 patients), it was conducted at a single center, and follow-up was limited to 12 months, reducing statistical power, generalizability, and assessment of long-term complications. Loss to follow-up (22.5%) may have introduced attrition bias. The involvement of multiple surgeons and the use of both titanium and stainless-steel implants could have affected outcomes. Functional assessments such as return to work, quality of life, pain scores, or validated scoring systems were not performed. Fracture complexity was not stratified, and assessors were not blinded, which may have introduced observer bias. Finally, rehabilitation protocols and patient compliance were not systematically monitored, which could have influenced recovery.
The current study concluded that there was no noteworthy difference between the two techniques in relation with operating time, rate of infection, knee motion range, and rates of malunion and non-union. However, IMN is better than minimally invasive plating in terms of the duration of hospital stay, speed of union, and early full weight bearing.
Both intramedullary nailing and minimally invasive proximal tibial plating provide stable fixation for extra-articular proximal tibial fractures with comparable rates of infection, malunion, and non-union. However, intramedullary nailing offers distinct advantages, including shorter hospital stay, faster fracture union, and earlier full weight bearing. Surgeons may consider IM nailing as a preferred option when early mobilization and reduced hospitalization are priorities, while remaining mindful that careful technique is required to avoid malalignment.
References
- 1. Lindvall E, Sanders R, DiPasquale T, Herscovici D, Haidukewych G, Sagi C. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009;23(7):485-492. doi:10.1097/BOT.0b013e3181b013d2. [Google Scholar]
- 2. Bhandari M, Audigé L, Ellis T, Hanson B; Evidence-Based Orthopaedic Trauma Working Group. Operative treatment of extra-articular proximal tibial fractures. J Orthop Trauma. 2003;17(8):591-595. doi:10.1097/00005131-200309000-00013. [Google Scholar]
- 3. Hiesterman TG, Shafiq BX, Cole PA. Intramedullary nailing of extra-articular proximal tibia fractures. J Am Acad Orthop Surg. 2011;19(11):690-700. doi:10.5435/00124635-201111000-00005. [Google Scholar]
- 4. Monahan KT, Zavras AG, Angelides GW, Altman GT, Altman DT, Westrick ER. Extra-articular proximal tibia fracture fixation with locked plating versus intramedullary nailing: meta-analysis. Injury. 2024;55(10):111718. doi:10.1016/j.injury.2024.111718. [Google Scholar]
- 5. Naik MA, Arora G, Tripathy SK, Sujir P, Rao SK. Clinical and radiological outcome of percutaneous plating in extra-articular proximal tibia fractures: a prospective study. Injury. 2013;44(8):1081-1086. doi:10.1016/j.injury.2013.03.002. [Google Scholar]
- 6. Prabhat V, Topno R, Kundu S, et al. A randomized trial comparing the outcome of expert tibial nail versus proximal tibial plate in the management of fractures of proximal tibia in adults. Ann Afr Med. 2025;24(2):361-369. doi:10.4103/aam.aam_209_24. [Google Scholar]
- 7. Koval KJ, Clapper MF, Brumback RJ, Ellison PS Jr., Poka A, Bathon GH, et al. Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma. 1991;5(2):184-189. [Google Scholar]
- 8. Buehler KC, Green J, Woll TS, Duwelius PJ. A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma. 1997;11(3):218-223. doi:10.1097/00005131-199704000-00014. [Google Scholar]
- 9. Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res. 1995;(315):25-33. [Google Scholar]
- 10. Krettek C, Stephan C, Schandelmaier P, Richter M, Pape HC, Miclau T. The use of Poller screws as blocking screws in stabilising tibial fractures treated with small-diameter intramedullary nails. J Bone Joint Surg Br. 1999;81(6):963-968. doi:10.1302/0301-620X.81B6.10000. [Google Scholar]
- 11. Meena RC, Meena UK, Gupta GL, Gahlot N, Gaba S. Intramedullary nailing versus proximal plating in the management of closed extra-articular proximal tibial fracture: a randomized controlled trial. J Orthop Traumatol. 2015;16(3):203-208. doi:10.1007/s10195-014-0332-9. [Google Scholar]
- 12. Ren C, Li M, Sun L, et al. Comparison of intramedullary nailing fixation and percutaneous locked plating fixation for the treatment of proximal tibial fractures: a meta-analysis. J Orthop Surg (Hong Kong). 2021;29(2):23094990211024395. doi:10.1177/23094990211024395. [Google Scholar]
- 13. Lu Y, Zheng J, Zhang L, et al. Combined medial plate and intramedullary nailing for extra-articular proximal tibial fractures: a biomechanical model. Front Bioeng Biotechnol. 2022;10:859512. doi:10.3389/fbioe.2022.859512. [Google Scholar]
- 14. Bogdan Y, Dedhia N. Proximal tibia and tibial plateau nail-plate combinations: technical trick and case series. OTA Int. 2022;5(3):e181. doi:10.1097/OI9.0000000000000181. [Google Scholar]