Metaphysio-diaphyseal angle (MDA) shows a significant positive correlation with radiographic severity of knee osteoarthritis (OA) and can serve as a reliable radiographic marker in OA assessment. In contrast, posterior tibial slope (PTS), despite its biomechanical relevance, does not show a statistically significant correlation with OA severity (Kellgren–Lawrence grade) in this study.
Dr. Rutvik Jain, Department of Orthopaedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India. E-mail: drrutvikjain@gmail.com
Introduction: Posterior tibial slope (PTS) and metaphysio-diaphyseal angle (MDA) are key anatomical angles influencing knee biomechanics. Their alterations may affect load distribution, contributing to osteoarthritis (OA) progression.
Objective: To evaluate the association of PTS and MDA with Kellgren–Lawrence (KL) grades of knee OA and investigate their correlation.
Materials and Methods: In this observational cross-sectional study, 92 patients with radiologically confirmed knee OA were recruited. Standard lateral and anteroposterior radiographs were used to measure PTS and MDA. OA severity was graded using the KL scale. Pearson’s correlation and multiple regression analyses were performed using Statistical Package for the Social Sciences v24.
Results: The mean PTS was 14.67° (standard deviation [SD] ± 3.03), and the mean MDA was 22.22° (SD ± 2.20). PTS and MDA showed a moderate positive correlation (r = 0.335, P < 0.01). MDA was significantly associated with KL grades (ρ = 0.3186, P = 0.0021), whereas PTS showed no statistically significant correlation (P = 0.157). Multiple regression confirmed MDA as a significant predictor of KL grade (P = 0.031).
Conclusion: MDA demonstrates potential as a reliable radiographic marker for assessing OA severity. Although PTS shows biomechanical importance, it did not correlate significantly with radiographic severity in this study. These findings highlight the clinical utility of MDA in OA evaluation and surgical planning.
Keywords: Posterior tibial slope, metaphysio-diaphyseal angle, osteoarthritis, Kellgren–Lawrence, knee biomechanics, radiographic severity.
Osteoarthritis (OA) of the knee is one of the most prevalent single human degenerative joint diseases, characterized by progressive erosion of articular cartilage, subchondral bone, and inflammation of synovium. It affects very much the quality of life in terms of pain, disability, and limited mobility, primarily among geriatric populations. Knee OA will continue to grow in its disease burden since current projections suggest that as many as 130 million persons will be affected globally by this condition by the year 2050; hence, a great deal of emphasis should be paid to understanding the pathophysiology, early diagnosis, and risk factors for appropriate management of the disease [1]. 28.7% of the Indian population suffers from symptomatic OA knee [2].
The metaphysio-diaphyseal angle (MDA) and posterior tibial slope (PTS) are important angles to consider in terms of tibial biomechanics concerning the physiological alignment of the knee joint [3], influencing load distribution, joint stability, and mechanical forces and, therefore, being relevant in the consideration of knee pathologies, including OA [3]. PTS is the posterior tilt of the tibial plateau in the sagittal plane, which varies from individual to individual depending on anatomical and genetic diverse factors [4]. Imbalance in the distribution of forces results in faster degeneration of cartilage, especially in the posterior compartments, and thus predisposes to OA [5]. MDA is the angular relationship between the metaphysis and diaphysis of the tibia, normally measured on radiographs [6]. Abnormalities in this angle can cause malalignment of the tibial axis, leading to abnormal load distribution through the knee joint [6]. This malalignment results in increased stress on the medial or lateral compartments, thus enhancing degenerative changes in the joint and structural collapse [6].
Radiographic imaging continues to be the prime method of diagnosing OA of the knee. The “Kellgren–Lawrence (KL) scale,” which grades the severity of OA from 0 (normal) to 4 (severe), is generally used to study progression and to guide treatment decisions [7]. Structural parameters such as PTS and MDA have gained an upsurge of interest in their role in OA pathogenesis. These anatomical parameters affect joint alignment and stress distribution, thereby offering them as potential early indicators or prognostic parameters for the disease [7].
This study was carried out for concurrent evaluation of PTS and MDA in ascertaining the primary biomechanical factors influencing knee OA. They could be considered markers to diagnose early-stage OA and those who are at greater risk of progression [8]. They are also very important for pre-operative planning of knees in surgery, such as total knee arthroplasty, where restoration of perfect alignment and biomechanical factors is paramount [8].
This was a cross-sectional, observational study conducted at the Department of Orthopaedics, Teerthanker Mahaveer Medical College and Research Centre, over a period of 18 months. Ethical approval was obtained from the Institutional Ethics Committee (IEC No.-TMU/IEC November 23/114). Informed consent was secured from all participants.
Inclusion criteria included patients aged 18 years and above with clinically and radiographically confirmed primary OA of the knee, KL grade ≥2. Exclusion criteria were: History of prior knee surgery, traumatic injuries, inflammatory arthritis, or congenital bone deformities.
Radiographic evaluation
Standardized anteroposterior and lateral radiographs of the affected knees were obtained in a weight-bearing position. The landmarks in the study included the tibial tuberosity, patella, and femoral condyles. DICOM software or the Angulus mobile app was used to analyze “Posterior Tibial Slope” and “Metaphysio-Diaphyseal Angle” after the radiographs were taken.
The PTS was measured by the anterior tibial cortex method. A line was drawn along the anterior border of the upper tibial cortex in a lateral radiographic view, which followed the longitudinal axis of the tibial shaft. The uppermost articular surface was then represented by a second line, drawn parallel to the tibial plateau. Moreover, we measured the angle between these two lines, which was the posterior inclination or slope, of the tibial plateau (Fig. 1).
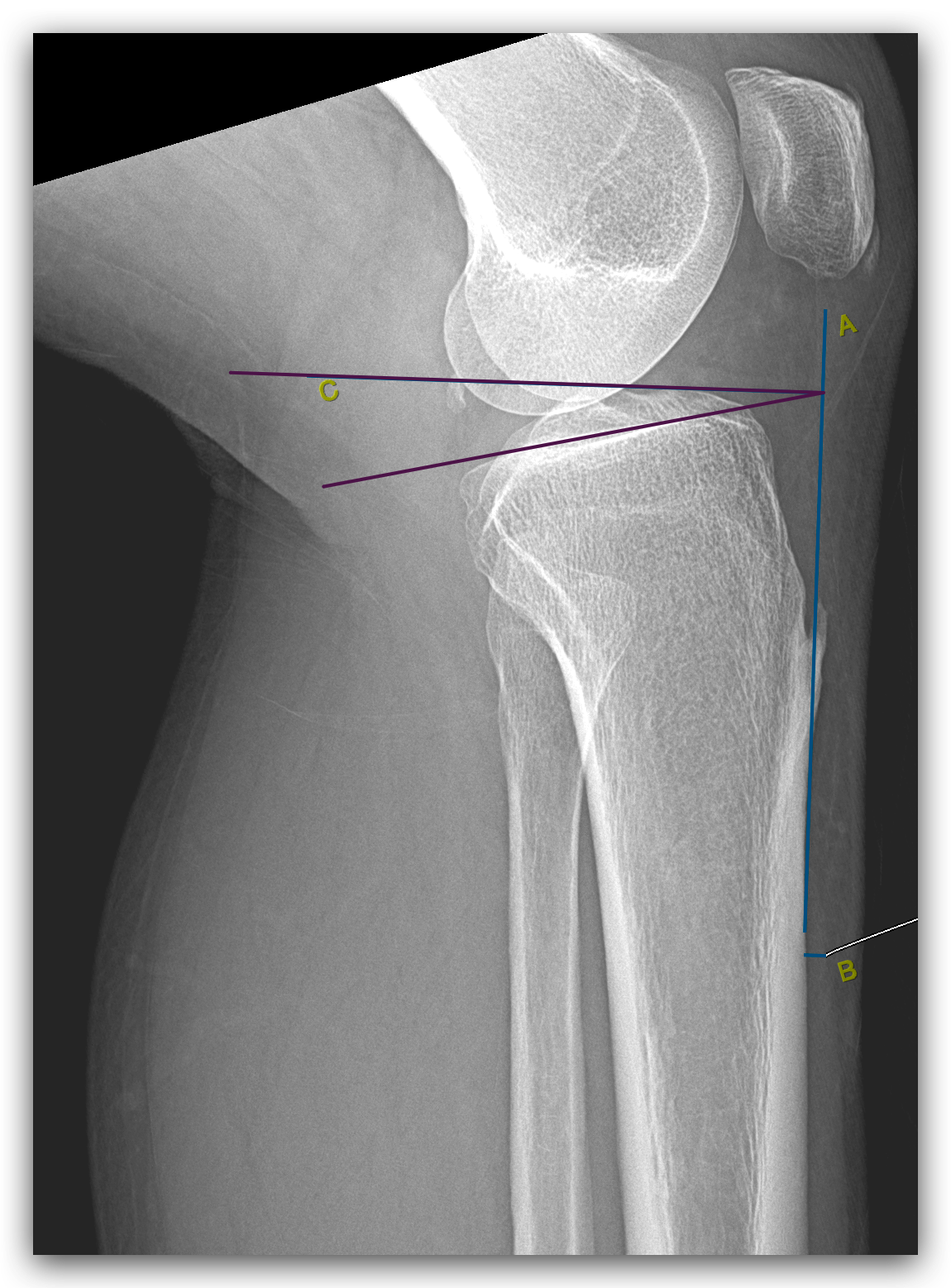
Figure 1: Posterior tibial slope measurement.
MDA, on a lateral radiograph, a line was drawn through the centers of the outer edges of the tibia at 5 cm and 15 cm below the knee. The MDA was estimated by measuring the angle between the anterior and posterior portions of the metaphysis, a line connecting the center of each surface of the proximal tibia metaphysis (Fig. 2).
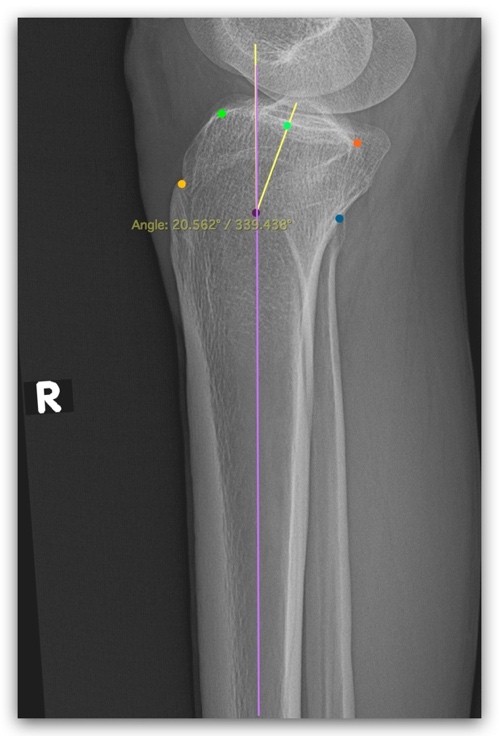
Figure 2: Metaphysio-diaphyseal angle measurement.
The KL grading was used to classify OA severity into grades 2, 3, and 4.
Sample size
A total of 92 patients (n = 92) were enrolled. Demographic and clinical data, including age, sex, laterality, and pain severity, were documented. Radiological parameters were independently evaluated by two senior orthopaedic consultants to reduce interobserver error.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 24. Descriptive statistics were used for demographic characteristics. The Pearson correlation coefficient was applied to analyze the relationship between PTS and MDA. Spearman’s rank correlation was used to correlate both angles with KL grade. Multiple linear regression was used to identify predictors of OA severity. P < 0.05 was considered statistically significant (Figs. 1 and 2).
The mean age of participants was 53.6 ± 10.4 years. Of the 92 patients, 70.6% were female, and 96.7% presented with bilateral symptoms. Severe pain was reported by 63.1% of patients. The mean PTS was 14.67° (range: 8.56°–23.24°) and the mean MDA was 22.22° (range: 17.79°–27.00°).
There is a statistically significant moderate positive correlation between PTS and MDA (r = 0.335, P < 0.01). This indicates that as the “PTS increases,” the “MDA tends to increase” as well. The relationship, while not strong, is meaningful and suggests a biomechanical link that may warrant further exploration in osteoarthritic knee evaluation and surgical planning (Table 1 and Graph 1).
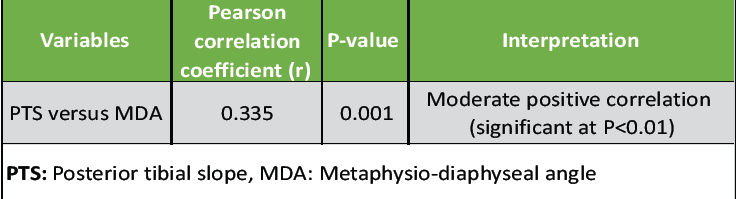 Table 1: Association between PTS and MDA
Table 1: Association between PTS and MDA
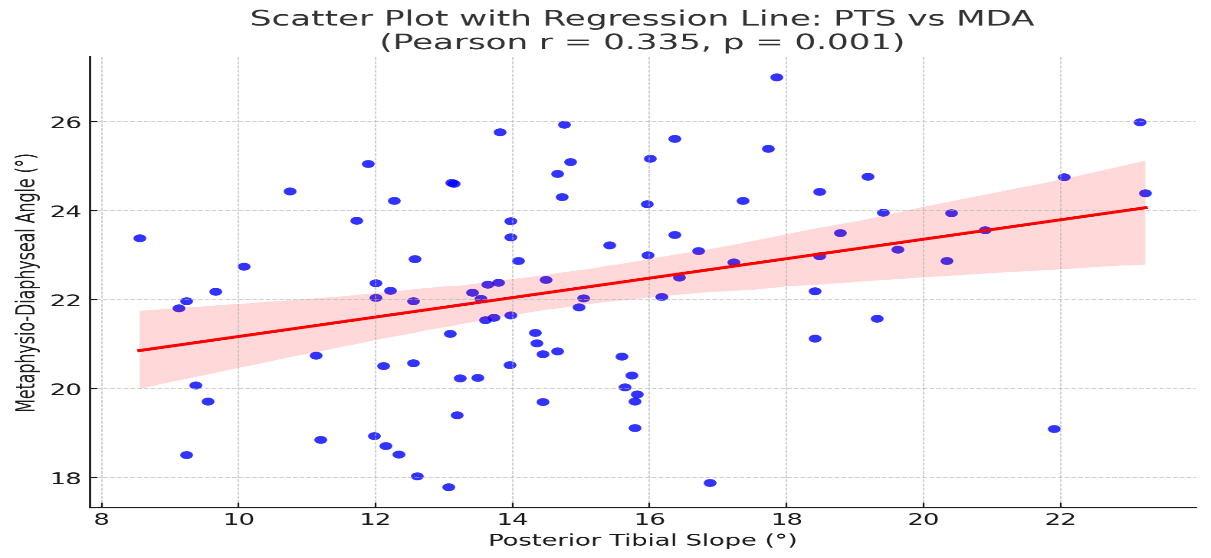 Graph 1: Scatter plot with regression line: Posterior tibial slope versus metaphysio-diaphyseal angle.
Graph 1: Scatter plot with regression line: Posterior tibial slope versus metaphysio-diaphyseal angle.
There is a clear trend of increasing mean PTS from KL Grade 2 (13.44°) to Grade 4 (15.33°), indicating a possible association between higher tibial slope and advanced OA severity. While MDA values remain relatively close across grades, a slight increase is seen in Grade 4 (22.65°), which may suggest structural adaptation or changes with disease progression. These findings suggest that both PTS and MDA show potential as radiographic markers for assessing OA severity. The statistical significance of these differences was confirmed using “ANOVA and post hoc analysis” (Table 2).
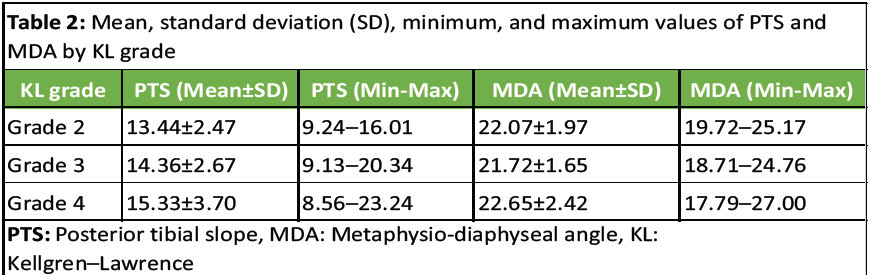 Table 2: Mean, standard deviation (SD), minimum, and maximum values of PTS and MDA by KL grade
Table 2: Mean, standard deviation (SD), minimum, and maximum values of PTS and MDA by KL grade
MDA shows a moderate positive correlation with KL grade, indicating that as OA severity increases (KL grade), the MDA tends to increase significantly. PTS, on the other hand, shows only a weak and statistically insignificant correlation with KL grade (Table 3).
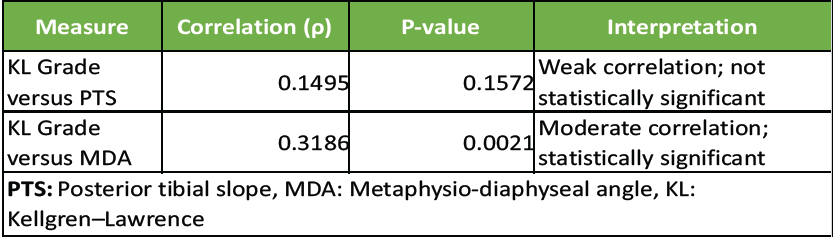 Table 3: Correlation analysis results (Spearman’s rank correlation)
Table 3: Correlation analysis results (Spearman’s rank correlation)
MDA is a statistically significant predictor of KL grade (P = 0.031), suggesting it could serve as a valid radiographic indicator of OA severity. PTS is not a significant predictor (P = 0.316) in this model. Although statistically significant, the model has a modest explanatory power (R² = 8.6%), indicating other factors may also contribute to KL grade determination (Table 4 and Graph 2).
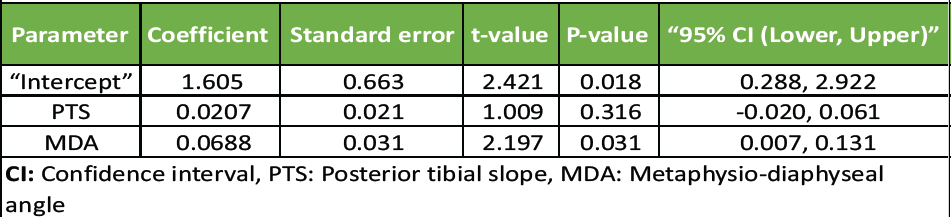 Table 4: Model summary (OLS regression results)
Table 4: Model summary (OLS regression results)
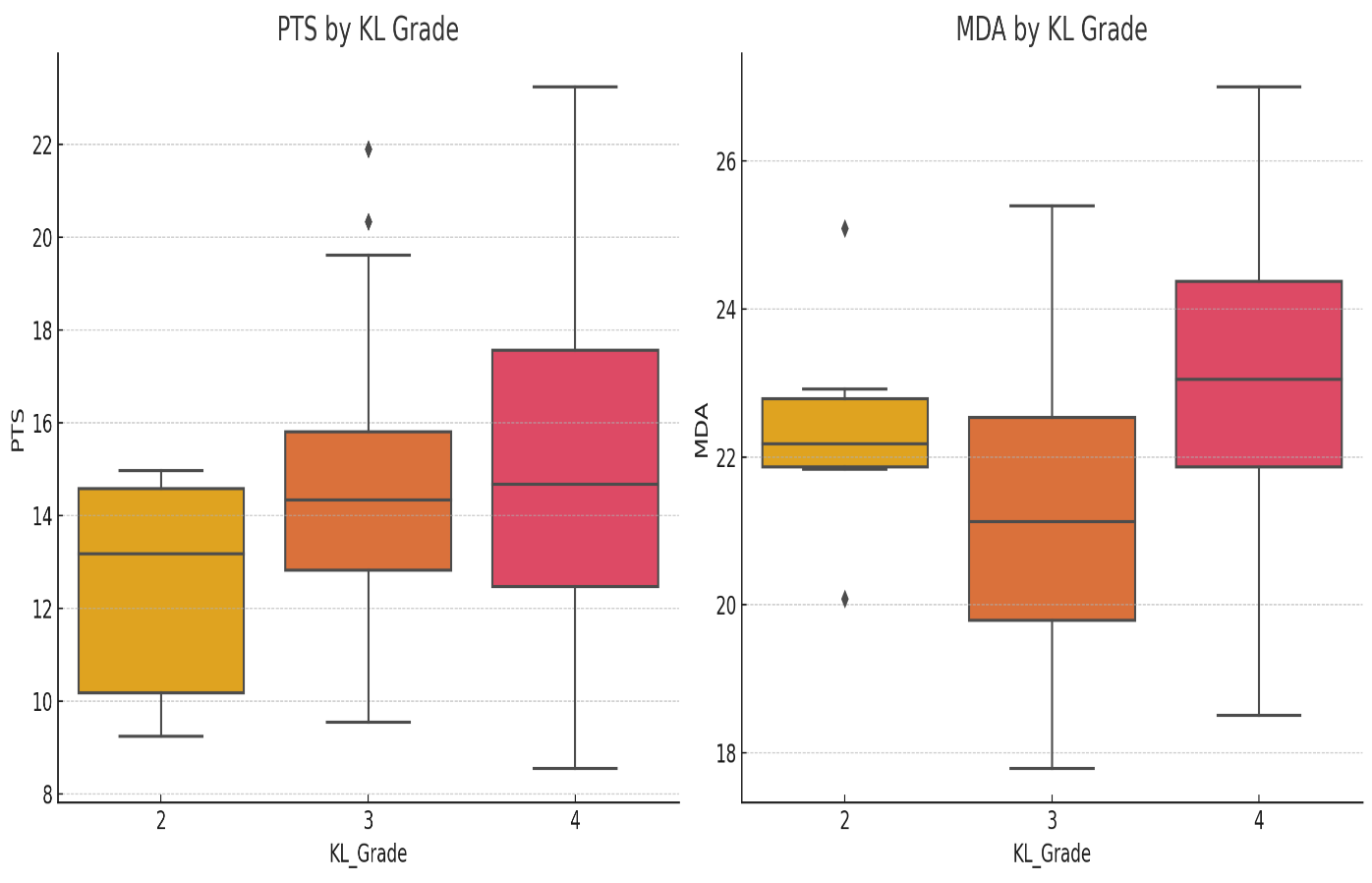 Graph 2: Box plot graph showing the relation of posterior tibial slope and metaphysio-diaphyseal angle with Kellgren–Lawrence grade.
Graph 2: Box plot graph showing the relation of posterior tibial slope and metaphysio-diaphyseal angle with Kellgren–Lawrence grade.
The purposes of the present study were to determine whether PTS, MDA, and KL grading of knee OA were associated. Findings significant to this investigation were the statistically significant correlation between MDA and OA severity, the moderate positive correlation between PTS and MDA, and no strong statistical correlation between PTS alone and KL grade. Observations are congruous with and often in contradistinction to previous work to further explicate the biomechanical influence of anatomical parameters on the radiographic progression of knee OA. More women (70.65%) took part in this study, which supports epidemiological studies that link postmenopausal hormonal changes to a higher OA risk. Yet, PTS changes by gender have not yet been studied using data analysis, so there is a need for further exploration, particularly with the discoveries from Pangaud et al. [9] and ALJuhani et al. [10].
This study included a total of 92 participants diagnosed with knee OA. The majority of respondents (39.13%) were in the age group of 51–60 years, followed by 28.26% above 60 years, “indicating a higher prevalence of osteoarthritis” in older adults. Thirunarayanan et al. [11] likewise observed the study group’s age distribution with a mean age of 56.34 years; people in the 50–60 age range are more likely to have OA.
On the mean PTS values from this dataset (14.67° ± 3.03°), mean rates from OA patients were higher (P < 0.05) than normative values (11.2° ± 3.0°) reported by Ho et al. [12] for healthy knees, suggesting an increase in slope among OA patients. Thirunarayanan et al. [11] likewise observed increased mean PTS between osteoarthritic knees (14.05° ± 2.38°) compared with normal knees (9.69° ± 1.81°), also consistent with the result that the OA group had greater PTS.
However, contrary to this study, which demonstrated no statistically significant correlation between PTS and the KL grade, as found by Meriç et al. [13] in arthritic patients, their study shows wide variability from PTS but without a direct linear correlation with OA severity. The data further suggest that PTS alone may not be a reliable predictor for radiographic grading of OA, as opposed to studies such as Moon et al. [14] that determined biomechanical influence on medial meniscus injury and OA progression due to increased PTS. The multifactorial nature of OA pathogenesis is reflected in an outcome influenced by dynamic mechanical loading and patient-specific variability.
Findings well support the role of MDA as a diagnostic and prognostic tool. A statistically significant correlation (ρ = 0.3186, P = 0.0021) between MDA and KL grade was found. Application to the work of Thirunarayanan et al. [11] shows that MDA in osteoarthritic knees is 25.03° ± 3.05°, compared to normal controls at 19.87° ± 2.70°, and that MDA is 90.1% sensitive and 84.7% specific as an OA indicator. Furthermore, Juneja et al. [15] reported that MDA had a significant impact on the surgical outcomes through monitoring the post-operative PTS alignment (P < 0.05), especially in varus knees.
Together, these findings suggest that when the knee deflects varus, a modified MDA makes the knee load more on the medial side, quickening the progression of degeneration. When the results tie in with what other studies have shown, it strengthens the idea that MDA should be added to standard imaging.
An important finding is that there is a weak but positive relationship between PTS and MDA (r = 0.335, P < 0.01). Mohanty et al. [16] commented similarly that combined changes in joint angles have impacts on joint movements and can lead to problems when setting up prosthetics during TKA. It also confirms the theory of Goyal et al. [17] that the combination of MDA errors happening with a greater tibial slope (PTS) applies more pressure on either side of the knee, increasing the risk of OA.
Because data have not “shown a strong relationship between the metrics” and the severity of “OA related to PTS,” looking further into such interdependence is still important for personalized surgery and prevention.
Based on the study, medical experts now have more reason to include MDA checks in regular imaging for knee OA. When modestly correlated and statistically relevant, MDA can be considered along with KL grading, mostly in early-stage conditions or borderline radiographic findings. As Bhattacharyya et al. [18] pointed out, a particular MDA value reliably detects early OA in Indian populations, so our results support using MDA in different groups worldwide.
Surprisingly, there was no strong link between PTS and KL grades that measure OA severity, even though PTS is of biomechanical importance. It is likely as useful or even more so for dynamic analysis or pre-operative preparation than for traditional grading on X-rays.
The PTS and MDA have significance in patients with knee OA. It focused on determining how useful these anatomical measurements are in assessing OA severity, according to the “Kellgren–Lawrence grading.” The findings suggest that the PTS and MDA could be useful aids in clinically measuring and tracking the development of OA.
Finally, this research puts forth MDA as a possible radiographic supporting indicator for the severity of OA. Interestingly, while the PTS was not a statistically strong independent marker, there is still clinical relevance to an interaction between PTS and MDA. These findings need further confirmation using advanced imaging techniques than those available today in larger-scale, longitudinal studies, and then additional biomechanical parameters should be explored. Such radiographic tools may be incorporated into the routine diagnostic algorithms and then provide earlier detection, targeted intervention, and more efficient management for knee OA patients.
Limitations
While this study provides useful insights, several limitations must be acknowledged. First, the cross-sectional design restricts the ability to establish causal relationships between tibial anatomical parameters and OA progression. Second, the study was conducted at a single tertiary care center, which may limit generalizability to wider or more diverse populations. Third, the relatively small sample size (n = 92) may have reduced the statistical power to detect subtle associations or perform robust subgroup analyses such as gender- or age-specific differences. Fourth, the absence of longitudinal follow-up prevents evaluation of dynamic changes in PTS or MDA over time and their role in disease progression. Fifth, radiographic assessments relied solely on plain radiographs, without advanced imaging modalities such as magnetic resonance imaging or computed tomography, which might have provided greater accuracy in structural evaluation. Sixth, although two senior consultants performed the measurements, inter- and intra-observer reliability was not formally assessed with statistical tools such as intraclass correlation coefficients. Seventh, the reliance on KL grading as the only marker of OA severity may not fully capture the clinical spectrum, as functional outcomes and patient-reported measures were not included. Eighth, potential confounders such as body mass index, activity level, comorbidities, or occupational loading patterns were not controlled for, which may have influenced the observed associations. Ninth, the study did not compare Indian population data with other ethnic groups, limiting external validity across global populations. Finally, the modest explanatory power of regression models (R2 = 8.6%) highlights that additional biomechanical, biological, or lifestyle factors likely play a significant role in disease severity, warranting further large-scale, multicenter, longitudinal research.
MDA is a valuable radiographic parameter that correlates significantly with the severity of knee OA and can be used as a supplementary tool for diagnosis, staging, and surgical planning. Although PTS is biomechanically important, it does not independently predict OA severity on radiographs and should not be solely relied upon for assessing disease progression. Incorporating MDA measurement into routine knee OA evaluations can enhance early detection, risk stratification, and better pre-operative alignment planning in total knee arthroplasty.
References
- 1. Bhattacharyya TD, Das P, Gogoi P, Sarmah R, Deka B, Haldar A. Comparative study of posterior tibial slope & metaphysio-diaphyseal angle in osteoarthritis knee and normal knee attending tertiary care centre in North-east India. J Orthop Rep 2025;4:100486. [Google Scholar] [PubMed]
- 2. Kumar H, Pal CP, Sharma YK, Kumar S, Uppal A. Epidemiology of knee osteoarthritis using Kellgren and lawrence scale in Indian population. J Clin Orthop Trauma 2020;11:S125-9. [Google Scholar] [PubMed]
- 3. Salamanna F, Caravelli S, Marchese L, Carniato M, Vocale E, Gardini G, et al. Proprioception and mechanoreceptors in osteoarthritis: A systematic literature review. J Clin Med 2023;12:6623. [Google Scholar] [PubMed]
- 4. Favero M, Ramonda R, Goldring MB, Goldring SR, Punzi L. Early knee osteoarthritis. RMD Open 2015;1 Suppl 1:e000062. [Google Scholar] [PubMed]
- 5. Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C. Knee osteoarthritis and obesity. Int J Obes Metab Disord 2001;25:622-7. [Google Scholar] [PubMed]
- 6. Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Deutsch Arztebl Int 2010;107:152-62. [Google Scholar] [PubMed]
- 7. Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop 2016;50:518-22. [Google Scholar] [PubMed]
- 8. Dulay GS, Cooper C, Dennison EM. Knee pain, knee injury, knee osteoarthritis & work. Best Pract Res Clin Rheumatol 2015;29:454-61. [Google Scholar] [PubMed]
- 9. Pangaud C, Blanchard C, Kerboull L, Courpied JP, Hamadouche M. Gender-related differences in femoral anatomy and component positioning in primary total knee arthroplasty. Orthop Traumatol Surg Res 2020;106:269-73. [Google Scholar] [PubMed]
- 10. AlJuhani A, Abdelhady A, Alzahrani MM, Alturki A, Khan WS. Gender-specific variations in tibial plateau anatomy and relevance for knee arthroplasty: A systematic review. J Orthop Surg Res 2020;15:95. [Google Scholar] [PubMed]
- 11. Thirunarayanan V, Sharma P, Mohan B. Posterior tibial slope and metaphysio-diaphyseal angle in osteoarthritic and normal knees: A comparative study. J Orthop Surg (Hong Kong) 2021;29:23094990211033334. [Google Scholar] [PubMed]
- 12. Ho CP, James EW, Surowiec RK, Stanish WD, LaPrade RF. Systematic review of the posterior tibial slope in healthy individuals. Orthop J Sports Med 2017;5:2325967117739846. [Google Scholar] [PubMed]
- 13. Meriç G, Selek H, Erdil M, Uluyardımcı E, Tümer H, Tuncay I. Posterior tibial slope angles in osteoarthritic knees: Correlation with the severity of osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2015;23:374-9. [Google Scholar] [PubMed]
- 14. Moon YW, Kim YH, Kwon SY, Kim JS. Influence of posterior tibial slope on the development of osteoarthritis in the medial compartment of the knee joint. J Bone Joint Surg Am 2020;102:388-95. [Google Scholar] [PubMed]
- 15. Juneja G, Marks A, Dunbar M. Influence of metaphyseal-diaphyseal angle on posterior tibial slope correction in total knee arthroplasty. Knee 2018;25:695-702. [Google Scholar] [PubMed]
- 16. Mohanty SS, Ghosh A, Das S. Kinematic and kinetic influence of lower limb alignment: A biomechanical review. Indian J Orthop 2013;47:581-8. [Google Scholar] [PubMed]
- 17. Goyal T, Tripathy SK, Sen RK, Kumar A. The combined influence of posterior tibial slope and coronal plane alignment on knee biomechanics and osteoarthritis progression. Orthop Rev (Pavia) 2017;9:7355. [Google Scholar] [PubMed]
- 18. Bhattacharyya M, Prakash M, Dutta A. Early radiographic signs of knee osteoarthritis in Indian adults: Predictive value of metaphyseal-diaphyseal angle. Indian J Radiol Imaging 2025;35:22-8. [Google Scholar] [PubMed]