Bilateral anterior hip dislocations are rare; it results from high-energy trauma, and early reduction is crucial to minimize complications
Dr. Jean de Dieu Tumusifu Manegabe, Department of Orthopaedic and Trauma, Hôpital Provincial General de Référence de Bukavu, Bukavu, Democratic Republic of Congo, Faculty of Medicine, Université Catholique de Bukavu, Bukavu, Democratic Republic of Congo, Bugabo 02, AV. Mission, Kadutu, Bukavu, R.D. Congo, Department of Orthopaedic and Trauma, Cliniques Universitaires Saint-Luc UCLouvain, av Hippocrate 10, 1200-Bruxelles, Belgium. E-mail: jeandedieutumusifu7@gmail.com
Introduction: Bilateral anterior hip dislocations are exceedingly rare, accounting for only 2–5% of all traumatic hip dislocations. They typically result from high-energy trauma, with most cases reported in road traffic accidents. Early reduction is crucial to minimize complications such as avascular necrosis, irreducibility, and post-traumatic osteoarthritis.
Case Report: We report the case of a 32-year-old male who sustained bilateral anterior hip dislocations, pubic type on the right and obturator type on the left, following a high-energy trauma involving a fall astride a roadside ravine. The patient presented with complete functional disability of both lower limbs. Radiographs confirmed the diagnosis, and an urgent closed reduction was performed using the modified Bigelow’s maneuver for the right hip and the Allis maneuver, followed by a levering maneuver for the left hip. Post-operative management included analgesia and a progressive mobilization protocol. At the 3-month follow-up, the patient had achieved pain-free ambulation, with only mild movement restriction.
Conclusion: This case highlights the rarity of bilateral anterior hip dislocations and the importance of early recognition and reduction to ensure optimal recovery. A structured management approach with timely reduction, imaging, and rehabilitation is crucial for a favorable outcome. Rehabilitation includes strict bed rest for a week, progressive return to walking with crutches for a week, then full support.
Keywords: Hip, traumatic, dislocation.
Traumatic hip dislocation (THD) in young individuals typically results from high-energy trauma. Bilateral anterior dislocation of the hip is exceptionally rare, accounting for only 2–5% of all THDs [1,2], with only a few cases previously reported [3]. Most of these cases are associated with road traffic accidents or high-impact trauma [2,3,4,5]. The literature contains numerous case reports and series discussing the etiology, mechanisms, classification, treatment, and prognosis of THD [2,3,4,5]. There is a consensus among authors that early reduction, ideally within 6 h after injury, is crucial to minimizing the risk of complications, such as avascular necrosis (AVN), irreducibility, and osteoarthritis. However, no clear consensus exists regarding the post-reduction management protocol [1,3,5].
In this report, we present a case that illustrates this rare and unusual injury.
A 32-year-old male patient was brought to the emergency department with complete functional disability of both lower limbs and extensive wounds. According to the bystanders who transported him, he had been struck by a vehicle and had fallen astride a roadside ravine. Both lower limbs were widely abducted, with the left limb in external rotation, abduction, and flexion, whereas the right limb was in external rotation, abduction, and extension at the hips. His buttocks had impacted the ground, acting as a force in this hip position. He did not lose consciousness but was unable to move. On examination, he was unable to move his right upper limb, which exhibited abnormal mobility at the mid-to-distal two-thirds of the right arm, with bone crepitus. Despite these findings, the vascular and neurological assessments of the arm were normal. The left lower limb was flexed, abducted, and externally rotated, with palpable displacement of the femoral head in the Scarpa’s triangle and an empty acetabulum. The lower right limb was extended, abducted, and externally rotated (Fig. 1). The neurovascular examination of both lower limbs was normal.

Figure 1: Clinical presentation of the patient.
The diagnoses were bilateral hip dislocations: obturator type on the left and pubic type on the right.
Radiographs of the pelvis and right arm confirmed bilateral hip dislocations with an associated fracture of the inferior acetabular margin of the right hip (Fig. 2).
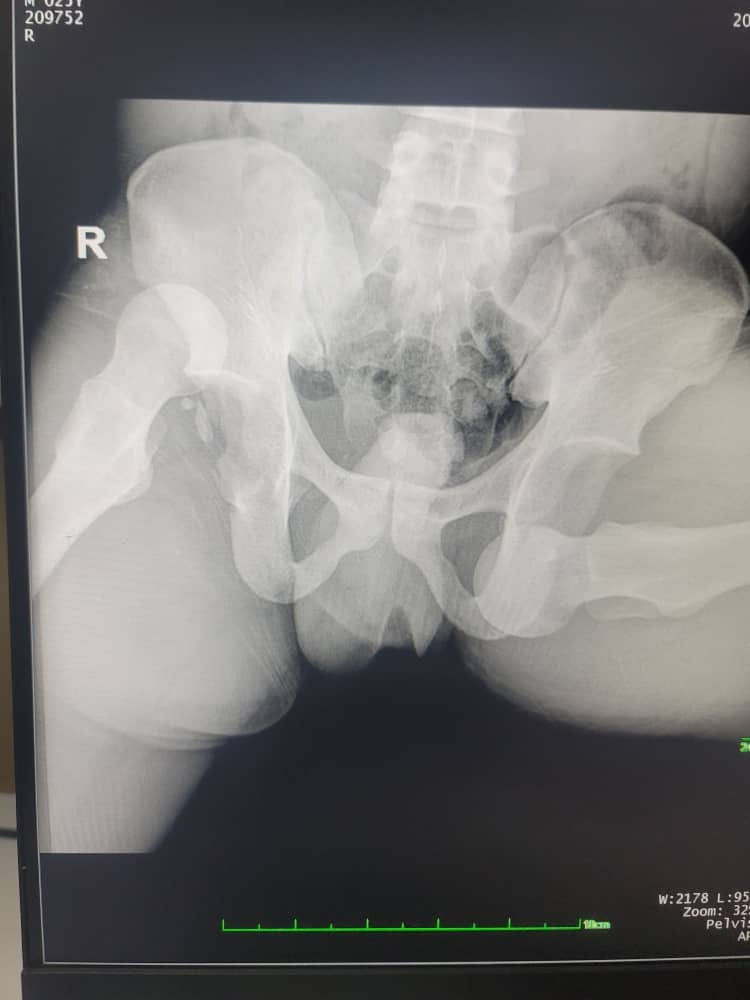
Figure 2: Initial X-ray.
The patient was taken to the operating room 30 min after trauma, where we performed a closed reduction of the right pubic dislocation and a challenging reduction of the left obturator dislocation under general anesthesia without fluoroscopy control. For the anterior and superior right hip dislocation, the surgeon applied traction in slight flexion, abduction, and external rotation to unlock the femoral head from its displaced position. Then, with continuous traction, the hip was gradually flexed and adducted while applying a gentle posterior force to guide the femoral head back into the acetabulum. Controlled maneuvers were essential to avoid complications, particularly iatrogenic fractures or neurovascular injuries. For the left hip dislocation (anterior), reduction was achieved by the Allis maneuver: flexing the hip and knee to approximately 90° to align the femur. Gentle longitudinal traction was applied along the femoral axis. Progressive adduction and internal rotation helped disengage the femoral head from the obturator foramen. A levering maneuver was then performed by applying a posterior and superior force to guide the femoral head back into the acetabulum. A control X-ray performed 4 h after trauma (Fig. 3) confirmed successful reduction of the hip dislocations and the associated fracture of the inferior acetabular margin of the right hip. A computed tomography (CT) scan was recommended, but the patient could not afford the examination.
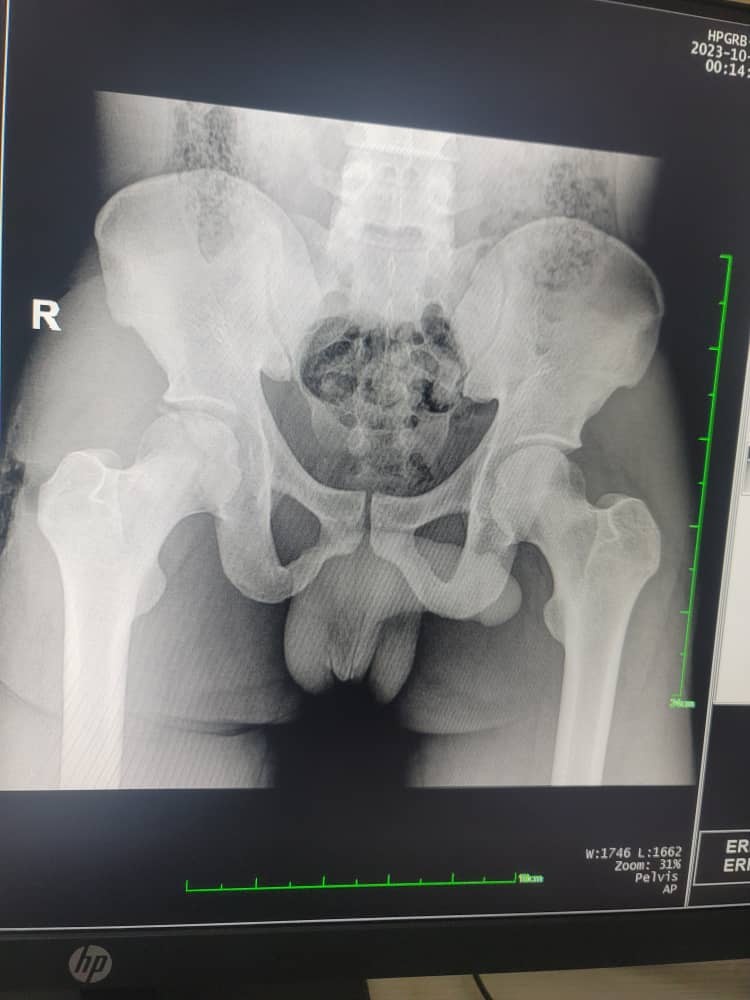
Figure 3: X-ray control after reduction.
Postoperatively, the patient was managed with a regimen of two analgesics (paracetamol and tramadol) and two antibiotics for 1 week (ampicillin and gentamicin). Strict bed rest for a week, progressive return to walking with crutches for a week, then full support and discharge after 3 weeks in hospital. At the 3-month follow-up, the reduction remained stable, and despite some mild movement restrictions, the patient was able to walk without pain, demonstrating good functional recovery.
THD is a critical emergency requiring immediate evaluation and treatment. Various mechanisms have been proposed for bilateral hip dislocation, including traffic accidents, excessive anterior and posterior forces, and falling on the back in a flexed position [6]. Hip dislocations occur more frequently in males, particularly in younger and working-age individuals, due to greater exposure to high-energy trauma. Gender and age are thus considered independent risk factors [2]. Although bilateral hip dislocations are rare, their management does not typically differ from unilateral cases, provided that prompt reduction is achieved.
High-energy trauma is typically required to dislocate the hip joint, and multiple complications may arise, especially in cases involving fractures. Reported complications include post-traumatic arthritis, AVN, heterotopic ossification (myositis ossificans), sciatic neuropathy, deep vein thrombosis, and recurrent dislocation [7]. Several factors influence the prognosis, including the time elapsed before reduction, the type of fracture-dislocation, the stability and accuracy of the reduction, and the extent of soft-tissue damage [8]. Anterior hip dislocations are less common than the posterior type, representing 10–15% of all cases [7]. Inferior dislocation accounts for more than 70% of anterior dislocations [9]. Anterior hip dislocations include different patterns: superior or pubic type, inferior or obturator type, and luxatio erecta of the hip [9]. The principles of closed hip reduction vary based on the type of dislocation [9]. In posterior dislocations, reduction involves flexion, internal rotation, and adduction of the hip. Techniques, such as the Böhler maneuver [10], Allis maneuver, Bigelow maneuver, and Captain Morgan approach, are commonly used [7,8,11]. In anterior dislocations, the modified Bigelow’s maneuver, consisting of linear traction in the axis of the deformation with the hip in external rotation, is usually required due to the anterior displacement of the femoral head. Obturator and pubic dislocations require external rotation to disengage the femoral head from the obturator foramen before using standard reduction techniques [2,11]. After reduction, careful documentation of the degree of flexion, adduction, and rotation during sedation is mandatory [6,11]. Cold packs, analgesics, and radiographic confirmation of proper hip alignment after reduction are also required. Irreducibility remains a rare complication of THD. It accounts for only 3% [12] of cases, and among the various potential causes, soft-tissue incarceration is the most frequent etiology. Surgical exploration allows for an initial assessment of the injuries and subsequently enables surgical reduction of the dislocation after removing the obstacle. The incidence of AVN after THD is variable, and it depends on causative factors. For anterior hip dislocations, the event rate for AVN ranged from 0.087 to 0.333, whereas posterior hip dislocations revealed that the event rate for AVN ranged from 0.106 to 0.430; the odds ratio of AVN for those hip dislocations reduced after 12 h versus those reduced before 12 h was 5.627 [13]. The time between injury and reduction strongly influences the occurrence of femoral head necrosis. Failure to perform reduction within 6 h after the injury can lead to a 50% incidence of femoral head necrosis [14]. Rehabilitation includes, in our case, strict bed rest for a week, progressive return to walking with crutches for a week, and, finally, full support allowing a nearly complete functional recovery at 3 months.
Double hip dislocation is an exceptionally rare injury typically resulting from high-energy trauma without a predisposing factor such as underlying disease, hip dysplasia, or medication use. Early recognition and prompt reduction are essential to minimize complications. Radiographs determine the direction of dislocation, whereas CT scans, when available, can assess associated fractures or soft-tissue injuries. Bed rest for 1 week followed by walking with crutches for 1 week allowed rapid recovery without further complications.
This case highlights the rarity of bilateral anterior hip dislocations and the importance of early reduction to prevent complications. It underscores the role of high-energy trauma in such injuries and the need for prompt orthopedic management. Proper imaging and timely intervention with appropriate reduction maneuvers ensure optimal functional recovery. Rehabilitation includes strict bed rest for a week and a progressive return to walking with crutches for a short period to achieve full recovery.
References
- 1. Gupta V, Goyal S, Garg R, Gupta N, Mohinadra M. Simultaneous anterior and posterior dislocation of hips: A case report and review of literature. Chin J Traumatol 2012;15:309-11. [Google Scholar] [PubMed]
- 2. Rufer B, Keel MJ, Schnüriger B, Deml MC. Bilateral hip dislocation: An indicator for emergent full-body computed tomography scan in polytraumatized patients? A case report and review of the literature. J Emerg Trauma Shock 2018;11:53-6. [Google Scholar] [PubMed]
- 3. Chung KJ, Eom SW, Noh KC, Kim HK, Hwang JH, Yoon HS, et al. Bilateral traumatic anterior dislocation of the hip with an unstable lumbar burst fracture. Clin Orthop Surg 2009;1:114-7. [Google Scholar] [PubMed]
- 4. Mandell JC, Marshal RA, Weaver MJ, Harris MB, Sodickson AD, Khrana B. Traumatic hip dislocation: What the orthopedic surgeon wants to know. Radiographics 2017;37:2181-201. [Google Scholar] [PubMed]
- 5. Amghar J, Aharram S, Benhammou M, Agoumi O, Daoudi A. Bilateral traumatic dislocation diverging from the hip. Int Arch Orthop Surg 2022;5:027. [Google Scholar] [PubMed]
- 6. Alexa O, Cozma T, Puha B, Alexa ID. Bilateral hip dislocation in a 79 years patient. Chirurgia (Bucur) 2012;107:122-5. [Google Scholar] [PubMed]
- 7. Schwartz SA, Taljanovic MS, Ruth JT, Miller MD. Bilateral asymmetric hip dislocation: Case report and literature review. Emerg Radiol 2003;10:105-8. [Google Scholar] [PubMed]
- 8. Shaw KA, Hire JM, Cearley DM. Salvage treatment options for painful hip dislocations in nonambulatory cerebral palsy patients. J Am Acad Orthop Surg 2020;28:363-75. [Google Scholar] [PubMed]
- 9. Rodríguez-Pérez M, Dávila-Parrilla A, Rivera L, Olivella G, Muñiz A, et al. Socioeconomic factors influencing self-reported outcomes after posterior wall fractures of the acetabulum: Lessons learned from a Hispanic population. J Am Acad Orthop Surg Glob Res Rev 2020;4:e20.00162. [Google Scholar] [PubMed]
- 10. Böhler J. Konservative therapie der luxationsfrakturen im hüftbereich [Conservative therapy of luxation fractures of the hip]. Langenbecks Arch Chir 1966;316:417-21. [Google Scholar] [PubMed]
- 11. Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:7-10. [Google Scholar] [PubMed]
- 12. EI-Andaloussi Y, Ait Essi F, Arssi M, Cohen D, Trafen M. Irreducible traumatic dislocation of the hip caused by labral and capsular entrapment with a buttonhole effect. Rev Chir Orthop Reparatrice Appar Mot 2006;92:279-82. [Google Scholar] [PubMed]
- 13. Kellam P, Ostrum RF. Systematic review and meta-analysis of avascular necrosis and posttraumatic arthritis after traumatic hip dislocation. J Orthop Trauma 2016;30:10-6. [Google Scholar] [PubMed]
- 14. Tekin AÇ, Çabuk H, Büyükkurt CD, Dedeoğlu SS, İmren Y, Gürbüz H. Inferior hip dislocation after falling from height: A case report. Int J Surg Case Rep 2016;22:62-5. [Google Scholar] [PubMed]